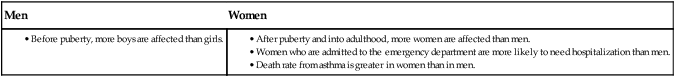
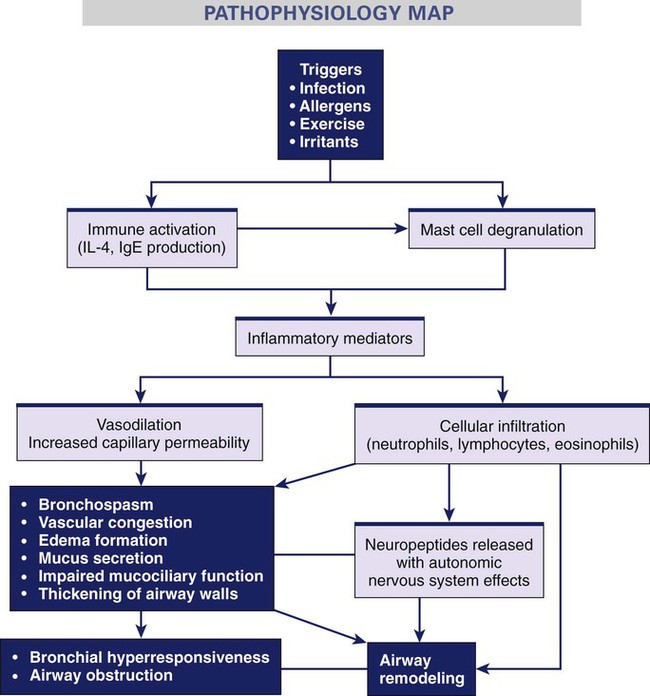
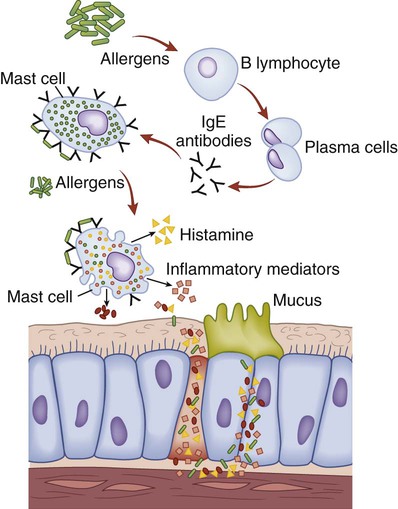
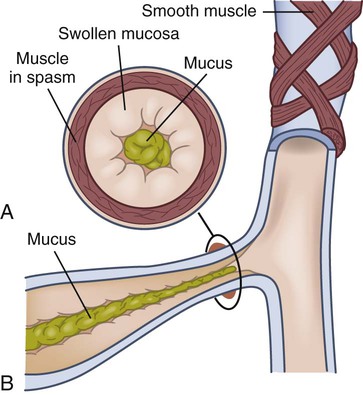
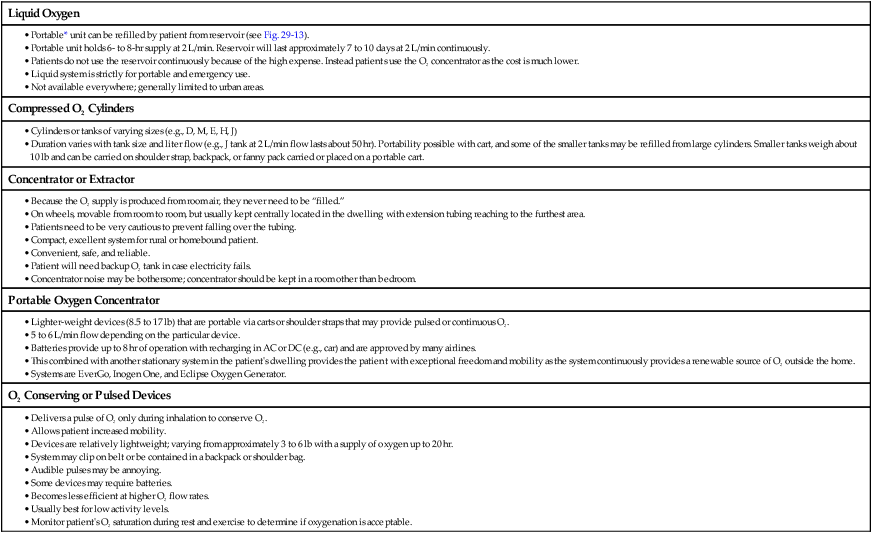
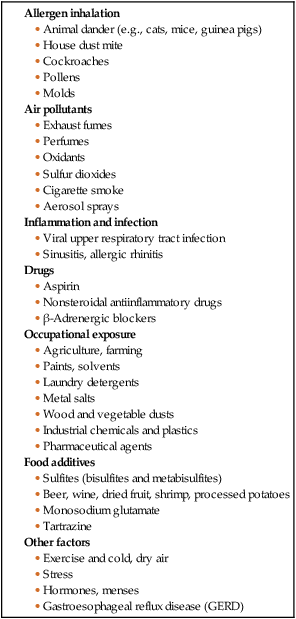
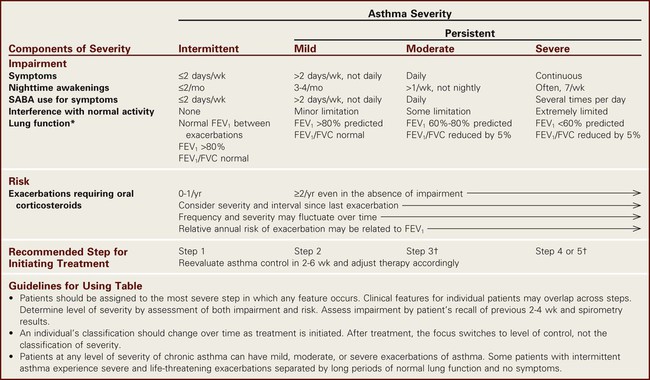
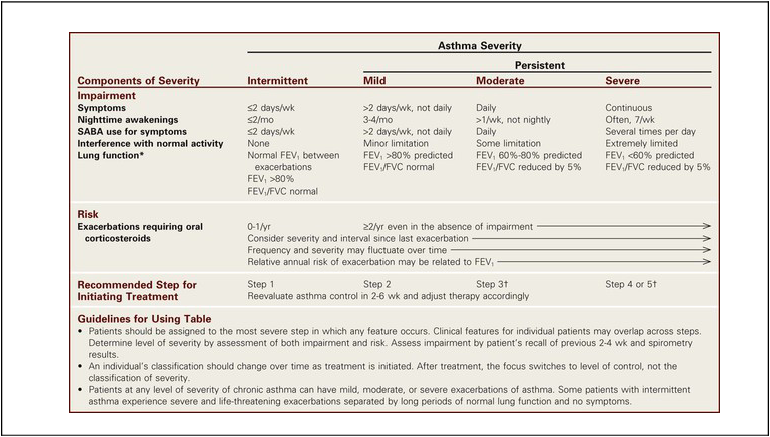
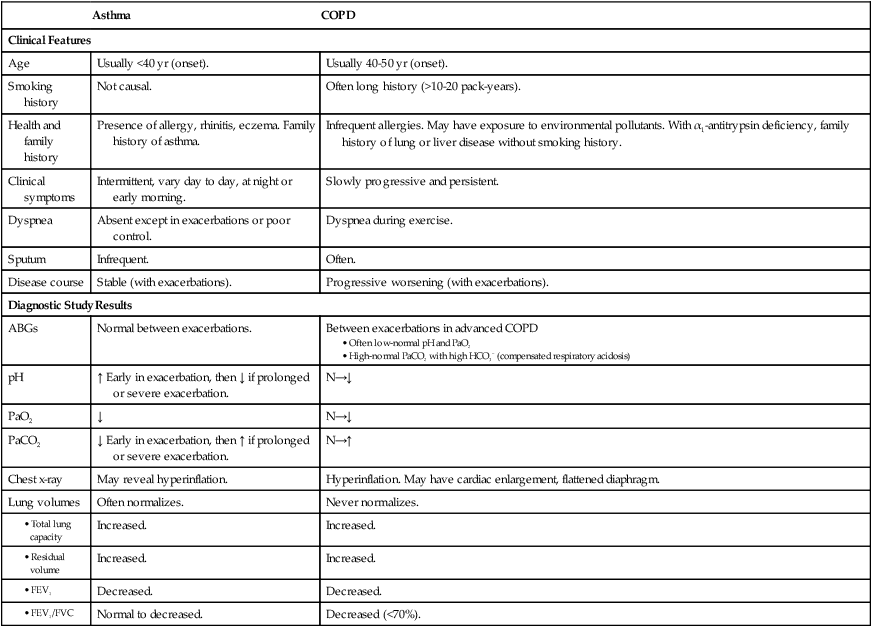
Chapter 29 1. Describe the etiology, pathophysiology, clinical manifestations, and collaborative care of asthma. 2. Describe the nursing management of the patient with asthma. 3. Describe the etiology, pathophysiology, clinical manifestations, and collaborative care of the patient with chronic obstructive pulmonary disease (COPD). 4. Describe the effects of cigarette smoking on the lungs. 5. Identify the indications for O2 therapy, methods of delivery, and complications of O2 administration. 6. Explain the nursing management of the patient with COPD. 7. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with cystic fibrosis. 8. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with bronchiectasis. Imagine needing to consciously think about every breath that you take for minutes, hours, or days. Many individuals with obstructive lung disease have this experience. Approximately 31.5 million adult Americans are living with asthma or chronic obstructive pulmonary disease (COPD).1,2 eTABLE 29-1 DRUG THERAPY *For patient instructions in English and Spanish for the devices, see www.chestnet.org/accp/patient-guides/patient-instructions-inhaled-devices-english-and-spanish. eTABLE 29-4 MODIFIED MEDICAL RESEARCH COUNCIL (mMRC) DYSPNEA SCALE Source: Fletcher CM, Elmes PC, Wood CH: The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population, BMJ 2:257, 1959. eTABLE 29-5 *Portable usually refers to units weighing more than 10 lb (4.5 kg); ambulatory units weigh less than 10 lb. Asthma is a chronic inflammatory disorder of the airways. The chronic inflammation leads to recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or in the early morning. These episodes are associated with widespread but variable airflow obstruction that is usually reversible, either spontaneously or with treatment. The clinical course of asthma is unpredictable, ranging from periods of adequate control to exacerbations with poor control of symptoms.3 Asthma affects an estimated 18.8 million adult Americans. Among adults, women are 62% more likely to have asthma than men. Asthma is a public health concern, with more than 14.2 million lost workdays in adults. However, the good news is that after a long period of an increasing incidence of asthma, the mortality and use of health care services are continuing to plateau and/or decrease. Despite the decline in the number of deaths from asthma over the past 10 years, more than 3300 people still die from asthma yearly.1 Risk factors for asthma and triggers of asthma attacks can be related to the patient (e.g., genetic factors) or the environment (e.g., pollen) (Table 29-1). Male gender is a risk factor for asthma in children (but not adults). Obesity is also a risk factor for asthma.4 Other factors and triggers are discussed in this section. TABLE 29-1 Asthma has a component that is inherited, but the genetics are complex. Numerous genes may be involved in the development of asthma and a person’s response to various asthma medications.3,4 Atopy, the genetic predisposition to develop an allergic (immunoglobulin E [IgE]–mediated) response to common allergens, is a major risk factor for asthma. The hygiene hypothesis suggests that a newborn baby’s immune system must be educated so it will function properly during infancy and the rest of life. People who are exposed to certain infections early in life, use few antibiotics, are exposed to other children (e.g., siblings, day care), or live in the country or with pets have a lower incidence of asthma. People for whom these factors are not present in childhood have a higher incidence of asthma.3 Various air pollutants, such as cigarette or wood smoke or vehicle exhaust, can trigger asthma attacks. In heavily industrialized or densely populated areas, climatic conditions often lead to concentrated pollution in the atmosphere, especially with thermal inversions and stagnant air masses. Ozone alert days are regularly noted on the news reports, and patients should minimize outdoor activity during these times. Cigarette smoking is associated with an accelerated decline of lung functioning in a person with asthma, increases the severity of the disease, may cause the patient to be less responsive to treatment, and reduces the chance of the asthma being controlled. Despite the relationship of pollutants in triggering asthma attacks, the role of outdoor air pollution as a cause of asthma development remains controversial.4 Occupational asthma is the most common occupational respiratory disorder, with up to 15% of new asthma cases arising from job-related exposures to more than 300 agents.4,5 Irritants cause a change in the responsiveness of the airways. However, the development of symptoms from this alteration may not occur until the patient has had months to years of exposure. Agricultural worker, baker, hospital worker, plastics manufacturer, and beautician are occupations with a high risk of occupational asthma. Characteristically people with occupational asthma give a history of arriving at work feeling well but gradually develop symptoms by the end of the day. Most patients with asthma have a history of allergic rhinitis. Treatment of allergic rhinitis usually improves the symptoms of asthma. Additional information on the relationship of rhinitis and asthma can be found at www.whiar.org. Acute and chronic sinusitis may worsen asthma. Some patients with asthma have chronic sinus problems that cause inflammation of the mucous membranes. Sinusitis must be treated and large nasal polyps removed for an asthma patient to have good control. (Sinusitis is discussed in Chapter 27.) Gastroesophageal reflux disease (GERD) is more common in people with asthma than in the general population. GERD may worsen asthma symptoms. Reflux may trigger bronchoconstriction and cause aspiration. On the other hand, asthma medications may worsen GERD symptoms. β2-Agonists (especially given orally), which are used to treat asthma, relax the lower esophageal sphincter, thus allowing stomach contents to reflux into the esophagus and possibly be aspirated into the lungs. Medications used to treat GERD usually do not reduce asthma symptoms in most people.4,6 (GERD is discussed in Chapter 42.) Asthma is not a psychosomatic disease. However, many people with asthma report that symptoms worsen with stress. Certainly psychologic factors cause bronchoconstriction via stimulation of the cholinergic reflex pathways. Extreme emotional expressions (e.g., crying, laughing, anger, fear) can lead to hyperventilation and hypocapnia, which can cause airway narrowing.4 The primary pathophysiologic process in asthma is persistent but variable inflammation of the airways. The airflow is limited because the inflammation results in bronchoconstriction, airway hyperresponsiveness (hyperreactivity), and edema of the airways. Exposure to allergens or irritants initiates the inflammatory cascade (Fig. 29-1). A variety of inflammatory cells are involved, including mast cells, macrophages, eosinophils, neutrophils, T and B lymphocytes, and epithelial cells of the airways.3 As the inflammatory process begins, mast cells (found beneath the basement membrane of the bronchial wall) degranulate and release multiple inflammatory mediators (Fig. 29-2). IgE antibodies are linked to mast cells, and the allergen cross-links the IgE. Then inflammatory mediators such as leukotrienes, histamine, cytokines, prostaglandins, and nitric oxide are released. Some inflammatory mediators have effects on the blood vessels, causing vasodilation and increasing capillary permeability. Some mediators result in the airways being infiltrated by eosinophils, lymphocytes, and neutrophils. The resulting inflammatory process causes vascular congestion, edema, production of thick and tenacious mucus, bronchial muscle spasm, thickening of airway walls, and increased bronchial hyperresponsiveness (Fig. 29-3). This whole process is sometimes referred to as the early-phase response in asthma. Clinically it can occur within 30 to 60 minutes after exposure to an allergen or irritant. Chronic inflammation may result in structural changes in the bronchial wall known as remodeling. A progressive loss of lung function occurs that is not prevented or fully reversed by therapy. The changes in structure may include fibrosis of the subepithelium, smooth muscle hypertrophy of the airways, mucus hypersecretion, continued inflammation, and angiogenesis (proliferation of new blood vessels). Remodeling is thought to explain why some individuals have persistent asthma and limited response to therapy.3,4 Hyperventilation occurs during an asthma attack as lung receptors respond to increased lung volume from trapped air and airflow limitation. Decreased perfusion and ventilation of the alveoli and increased alveolar gas pressure lead to ventilation-perfusion abnormalities in the lungs. The patient is hypoxemic early on with decreased PaCO2 and increased pH (respiratory alkalosis) because he or she is hyperventilating. As the airflow limitation worsens with air trapping, the patient works much harder to breathe. The PaCO2 normalizes as the patient tires, and then it increases to produce respiratory acidosis, which is an ominous sign of respiratory failure.6 Wheezing is an unreliable sign to gauge the severity of an attack. Many patients with minor attacks wheeze loudly, whereas others with severe attacks do not wheeze. The patient with severe asthma attacks may have no audible wheezing because of the marked reduction in airflow. For wheezing to occur, the patient must be able to move enough air to produce the sound. Wheezing usually occurs first on exhalation. As asthma progresses, the patient may wheeze during inspiration and expiration. The term wheezing may also be used to describe sounds arising from the nose and upper airways.7 Asthma can be classified as intermittent, mild persistent, moderate persistent, or severe persistent (Table 29-2). The classification system is used to determine the treatment. Patients may move to different asthma classifications over the course of their disease. TABLE 29-2 CLASSIFICATION OF ASTHMA SEVERITY †Consider short-term corticosteroid therapy. Source: Adapted from National Asthma Education and Prevention Program, National Heart, Lung, and Blood Institute: Expert Panel Report 3: guidelines for the diagnosis and management of asthma, NIH pub no 08-4051, Bethesda, Md, 2007, National Institutes of Health. Retrieved from www.nhlbi.nih.gov/guidelines. Severe asthma exacerbations occur when the patient is dyspneic at rest and the patient speaks in words, not sentences, because of the difficulty of breathing. The patient is usually sitting forward to maximize the diaphragmatic movement with prominent wheezing, a respiratory rate higher than 30 breaths/minute, and pulse greater than 120 beats/minute. Accessory muscles in the neck are straining to lift the chest wall, and the patient is often agitated. The peak flow (peak expiratory flow rate [PEFR]) is 40% of the personal best or less than 150 L/minute. Arterial blood gas (ABG) changes are listed in Table 29-3. Neck vein distention may result. These patients usually are seen in emergency departments (EDs) or hospitalized.6 TABLE 29-3 COMPARISON OF ASTHMA AND COPD* ABGs, Arterial blood gases; FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity.
Nursing Management
Obstructive Pulmonary Diseases
Asthma and Chronic Obstructive Pulmonary Disease (enhanced)
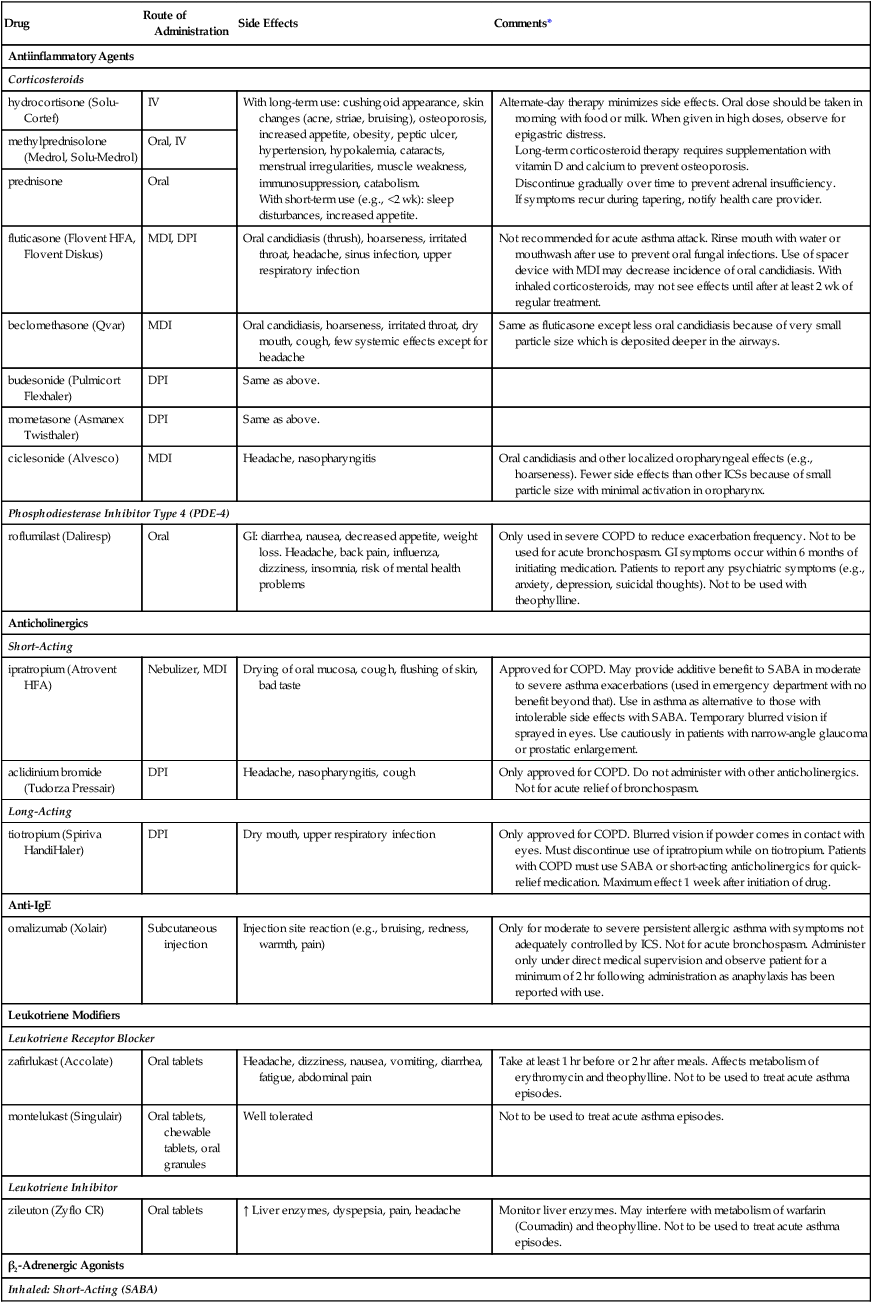
Drug
Route of Administration
Side Effects
Comments*
Antiinflammatory Agents
Corticosteroids
hydrocortisone (Solu-Cortef)
IV
With long-term use: cushingoid appearance, skin changes (acne, striae, bruising), osteoporosis, increased appetite, obesity, peptic ulcer, hypertension, hypokalemia, cataracts, menstrual irregularities, muscle weakness, immunosuppression, catabolism.
With short-term use (e.g., <2 wk): sleep disturbances, increased appetite.
Alternate-day therapy minimizes side effects. Oral dose should be taken in morning with food or milk. When given in high doses, observe for epigastric distress.
Long-term corticosteroid therapy requires supplementation with vitamin D and calcium to prevent osteoporosis.
Discontinue gradually over time to prevent adrenal insufficiency.
If symptoms recur during tapering, notify health care provider.
methylprednisolone (Medrol, Solu-Medrol)
Oral, IV
prednisone
Oral
fluticasone (Flovent HFA, Flovent Diskus)
MDI, DPI
Oral candidiasis (thrush), hoarseness, irritated throat, headache, sinus infection, upper respiratory infection
Not recommended for acute asthma attack. Rinse mouth with water or mouthwash after use to prevent oral fungal infections. Use of spacer device with MDI may decrease incidence of oral candidiasis. With inhaled corticosteroids, may not see effects until after at least 2 wk of regular treatment.
beclomethasone (Qvar)
MDI
Oral candidiasis, hoarseness, irritated throat, dry mouth, cough, few systemic effects except for headache
Same as fluticasone except less oral candidiasis because of very small particle size which is deposited deeper in the airways.
budesonide (Pulmicort Flexhaler)
DPI
Same as above.
mometasone (Asmanex Twisthaler)
DPI
Same as above.
ciclesonide (Alvesco)
MDI
Headache, nasopharyngitis
Oral candidiasis and other localized oropharyngeal effects (e.g., hoarseness). Fewer side effects than other ICSs because of small particle size with minimal activation in oropharynx.
Phosphodiesterase Inhibitor Type 4 (PDE-4)
roflumilast (Daliresp)
Oral
GI: diarrhea, nausea, decreased appetite, weight loss. Headache, back pain, influenza, dizziness, insomnia, risk of mental health problems
Only used in severe COPD to reduce exacerbation frequency. Not to be used for acute bronchospasm. GI symptoms occur within 6 months of initiating medication. Patients to report any psychiatric symptoms (e.g., anxiety, depression, suicidal thoughts). Not to be used with theophylline.
Anticholinergics
Short-Acting
ipratropium (Atrovent HFA)
Nebulizer, MDI
Drying of oral mucosa, cough, flushing of skin, bad taste
Approved for COPD. May provide additive benefit to SABA in moderate to severe asthma exacerbations (used in emergency department with no benefit beyond that). Use in asthma as alternative to those with intolerable side effects with SABA. Temporary blurred vision if sprayed in eyes. Use cautiously in patients with narrow-angle glaucoma or prostatic enlargement.
aclidinium bromide (Tudorza Pressair)
DPI
Headache, nasopharyngitis, cough
Only approved for COPD. Do not administer with other anticholinergics. Not for acute relief of bronchospasm.
Long-Acting
tiotropium (Spiriva HandiHaler)
DPI
Dry mouth, upper respiratory infection
Only approved for COPD. Blurred vision if powder comes in contact with eyes. Must discontinue use of ipratropium while on tiotropium. Patients with COPD must use SABA or short-acting anticholinergics for quick-relief medication. Maximum effect 1 week after initiation of drug.
Anti-IgE
omalizumab (Xolair)
Subcutaneous injection
Injection site reaction (e.g., bruising, redness, warmth, pain)
Only for moderate to severe persistent allergic asthma with symptoms not adequately controlled by ICS. Not for acute bronchospasm. Administer only under direct medical supervision and observe patient for a minimum of 2 hr following administration as anaphylaxis has been reported with use.
Leukotriene Modifiers
Leukotriene Receptor Blocker
zafirlukast (Accolate)
Oral tablets
Headache, dizziness, nausea, vomiting, diarrhea, fatigue, abdominal pain
Take at least 1 hr before or 2 hr after meals. Affects metabolism of erythromycin and theophylline. Not to be used to treat acute asthma episodes.
montelukast (Singulair)
Oral tablets, chewable tablets, oral granules
Well tolerated
Not to be used to treat acute asthma episodes.
Leukotriene Inhibitor
zileuton (Zyflo CR)
Oral tablets
↑ Liver enzymes, dyspepsia, pain, headache
Monitor liver enzymes. May interfere with metabolism of warfarin (Coumadin) and theophylline. Not to be used to treat acute asthma episodes.
β2-Adrenergic Agonists
Inhaled: Short-Acting (SABA)
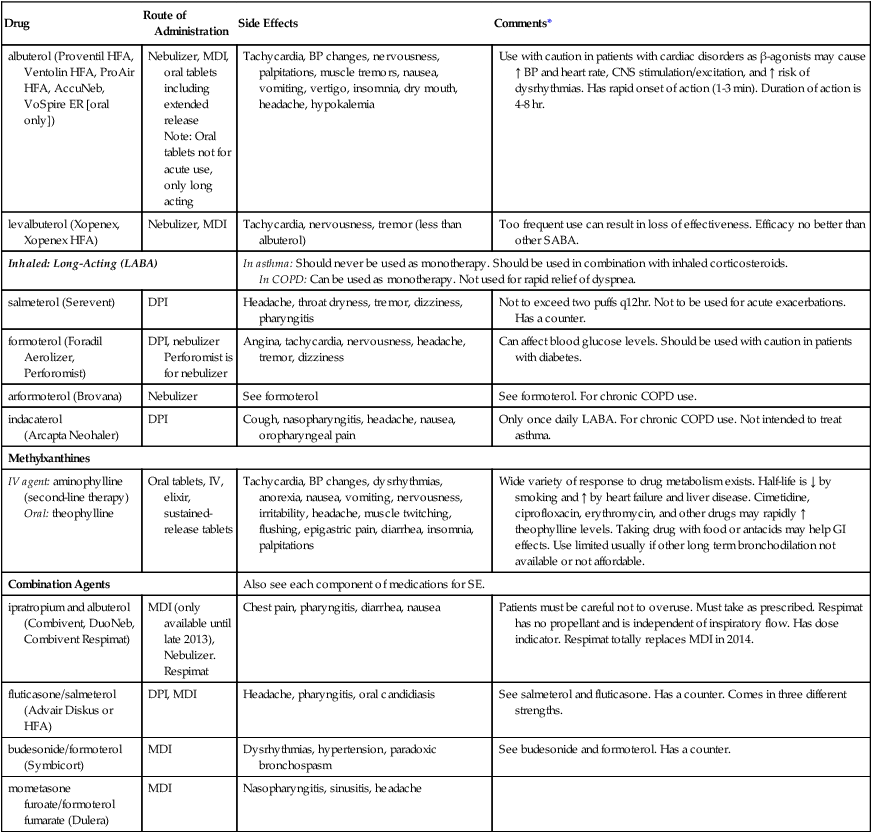
albuterol (Proventil HFA, Ventolin HFA, ProAir HFA, AccuNeb, VoSpire ER [oral only])
Nebulizer, MDI, oral tablets including extended release
Note: Oral tablets not for acute use, only long acting
Tachycardia, BP changes, nervousness, palpitations, muscle tremors, nausea, vomiting, vertigo, insomnia, dry mouth, headache, hypokalemia
Use with caution in patients with cardiac disorders as β-agonists may cause ↑ BP and heart rate, CNS stimulation/excitation, and ↑ risk of dysrhythmias. Has rapid onset of action (1-3 min). Duration of action is 4-8 hr.
levalbuterol (Xopenex, Xopenex HFA)
Nebulizer, MDI
Tachycardia, nervousness, tremor (less than albuterol)
Too frequent use can result in loss of effectiveness. Efficacy no better than other SABA.
Inhaled: Long-Acting (LABA)
In asthma: Should never be used as monotherapy. Should be used in combination with inhaled corticosteroids.
In COPD: Can be used as monotherapy. Not used for rapid relief of dyspnea.
salmeterol (Serevent)
DPI
Headache, throat dryness, tremor, dizziness, pharyngitis
Not to exceed two puffs q12hr. Not to be used for acute exacerbations. Has a counter.
formoterol (Foradil Aerolizer, Perforomist)
DPI, nebulizer
Perforomist is for nebulizer
Angina, tachycardia, nervousness, headache, tremor, dizziness
Can affect blood glucose levels. Should be used with caution in patients with diabetes.
arformoterol (Brovana)
Nebulizer
See formoterol
See formoterol. For chronic COPD use.
indacaterol
(Arcapta Neohaler)
DPI
Cough, nasopharyngitis, headache, nausea, oropharyngeal pain
Only once daily LABA. For chronic COPD use. Not intended to treat asthma.
Methylxanthines
IV agent: aminophylline (second-line therapy)
Oral: theophylline
Oral tablets, IV, elixir, sustained-release tablets
Tachycardia, BP changes, dysrhythmias, anorexia, nausea, vomiting, nervousness, irritability, headache, muscle twitching, flushing, epigastric pain, diarrhea, insomnia, palpitations
Wide variety of response to drug metabolism exists. Half-life is ↓ by smoking and ↑ by heart failure and liver disease. Cimetidine, ciprofloxacin, erythromycin, and other drugs may rapidly ↑ theophylline levels. Taking drug with food or antacids may help GI effects. Use limited usually if other long term bronchodilation not available or not affordable.
Combination Agents
Also see each component of medications for SE.
ipratropium and albuterol (Combivent, DuoNeb, Combivent Respimat)
MDI (only available until late 2013), Nebulizer. Respimat
Chest pain, pharyngitis, diarrhea, nausea
Patients must be careful not to overuse. Must take as prescribed. Respimat has no propellant and is independent of inspiratory flow. Has dose indicator. Respimat totally replaces MDI in 2014.
fluticasone/salmeterol (Advair Diskus or HFA)
DPI, MDI
Headache, pharyngitis, oral candidiasis
See salmeterol and fluticasone. Has a counter. Comes in three different strengths.
budesonide/formoterol (Symbicort)
MDI
Dysrhythmias, hypertension, paradoxic bronchospasm
See budesonide and formoterol. Has a counter.
mometasone furoate/formoterol fumarate (Dulera)
MDI
Nasopharyngitis, sinusitis, headache
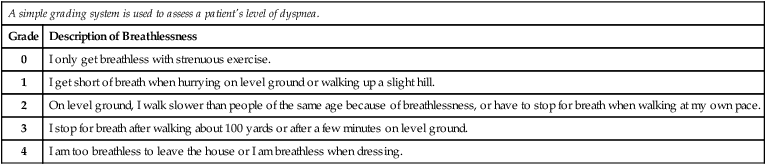
A simple grading system is used to assess a patient’s level of dyspnea.
Grade
Description of Breathlessness
0
I only get breathless with strenuous exercise.
1
I get short of breath when hurrying on level ground or walking up a slight hill.
2
On level ground, I walk slower than people of the same age because of breathlessness, or have to stop for breath when walking at my own pace.
3
I stop for breath after walking about 100 yards or after a few minutes on level ground.
4
I am too breathless to leave the house or I am breathless when dressing.
Asthma
Risk Factors for Asthma and Triggers of Asthma Attacks
Genetics.
Immune Response.
Air Pollutants.
Occupational Factors.
Nose and Sinus Problems.
Gastroesophageal Reflux Disease.
Psychologic Factors.
Pathophysiology
Clinical Manifestations
Classification of Asthma
Complications
Severe and Life-Threatening Asthma Exacerbations.
Asthma
COPD
Clinical Features
Age
Usually <40 yr (onset).
Usually 40-50 yr (onset).
Smoking history
Not causal.
Often long history (>10-20 pack-years).
Health and family history
Presence of allergy, rhinitis, eczema. Family history of asthma.
Infrequent allergies. May have exposure to environmental pollutants. With α1-antitrypsin deficiency, family history of lung or liver disease without smoking history.
Clinical symptoms
Intermittent, vary day to day, at night or early morning.
Slowly progressive and persistent.
Dyspnea
Absent except in exacerbations or poor control.
Dyspnea during exercise.
Sputum
Infrequent.
Often.
Disease course
Stable (with exacerbations).
Progressive worsening (with exacerbations).
Diagnostic Study Results
ABGs
Normal between exacerbations.
Between exacerbations in advanced COPD
pH
↑ Early in exacerbation, then ↓ if prolonged or severe exacerbation.
N→↓
PaO2
↓
N→↓
PaCO2
↓ Early in exacerbation, then ↑ if prolonged or severe exacerbation.
N→↑
Chest x-ray
May reveal hyperinflation.
Hyperinflation. May have cardiac enlargement, flattened diaphragm.
Lung volumes
Often normalizes.
Never normalizes.
Increased.
Increased.
Increased.
Increased.
Decreased.
Decreased.
Normal to decreased.
Decreased (<70%).
Nursing Management: Obstructive Pulmonary Diseases
Get Clinical Tree app for offline access