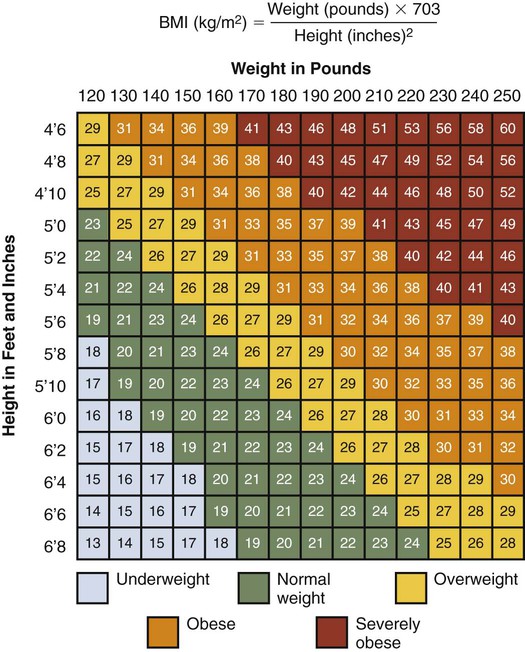
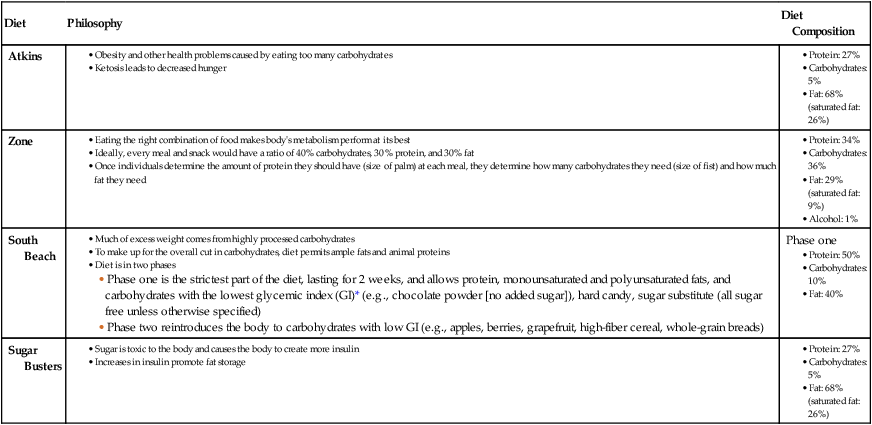
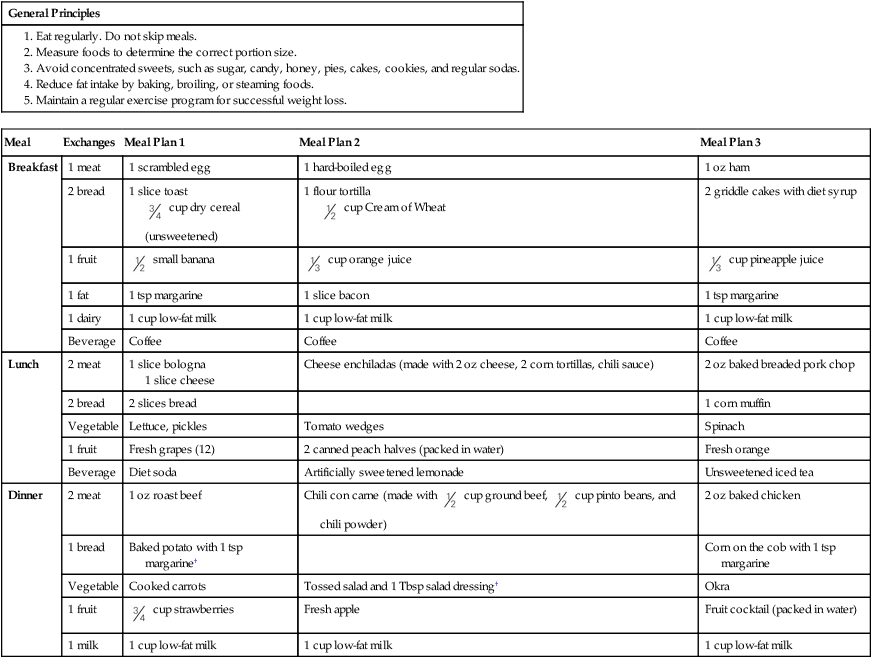
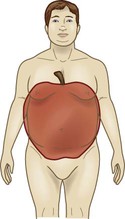
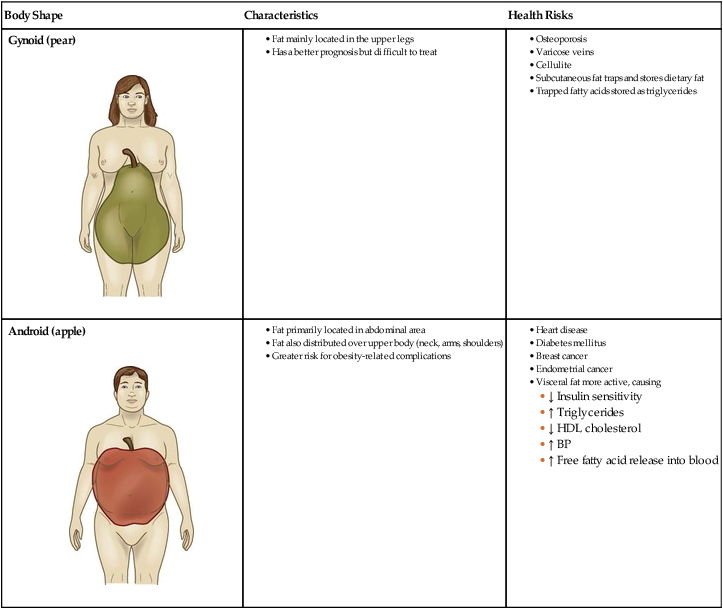
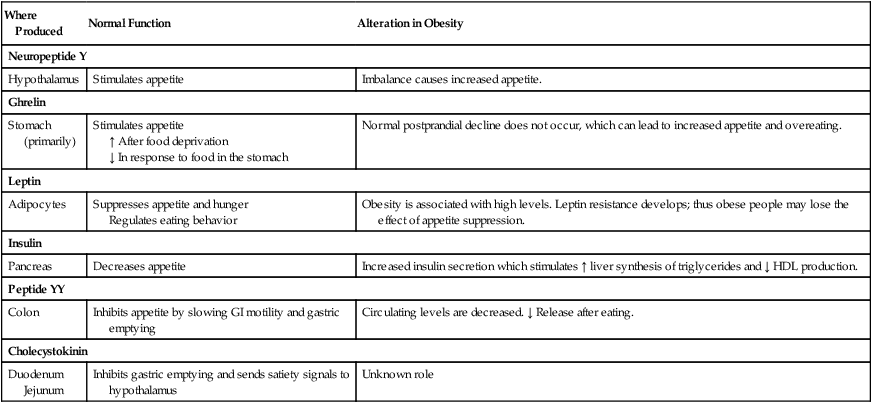
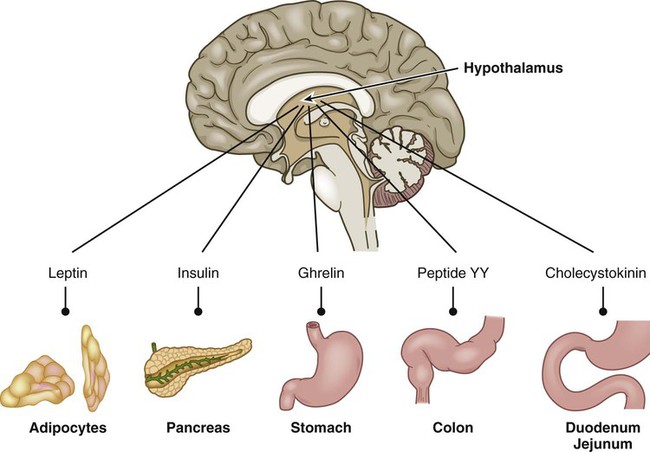
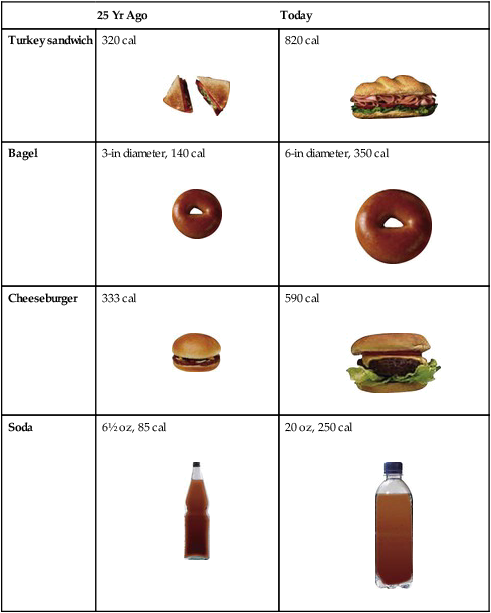
Chapter 41 1. Discuss the epidemiology and etiology of obesity. 2. Compare the classification systems for determining a person’s body size. 3. Explain the health risks associated with obesity. 4. Discuss nutritional therapy and exercise plans for the obese patient. 5. Describe the different bariatric surgical procedures used to treat obesity. 6. Describe the nursing management related to conservative and surgical therapies for obesity. 7. Describe the etiology, clinical manifestations, and nursing and collaborative management of metabolic syndrome. Obesity is an excessively high amount of body fat or adipose tissue (Fig. 41-1). Obesity is a major health problem because it increases the risk of numerous other diseases such as diabetes and cancer.1 An important part of your patient assessment is to determine and classify a patient’s body weight. A number of assessment methods are available, including body mass index (BMI), waist circumference, waist-to-hip ratio (WHR), and body shape. The most widely used and endorsed measures are BMI and waist circumference.2 These measures are cost-effective with acceptable reliability and are easily used in all practice settings. The most common measure of obesity is the body mass index (BMI). BMI is calculated by dividing a person’s weight (in kilograms) by the square of the height in meters (Fig. 41-2). Individuals with a BMI less than 18.5 kg/m2 are considered underweight, whereas those with a BMI between 18.5 and 24.9 kg/m2 reflect a normal body weight. A BMI of 25 to 29.9 kg/m2 is classified as being overweight, and those with values at 30 kg/m2 or above are considered obese. The term severely (morbidly, extremely) obese is used for those with a BMI greater than 40 kg/m2 (eFig. 41-1 on the website shows individuals who are severely obese). eTABLE 41-1 *Glycemic index is the term used to describe the rise in blood glucose levels after a person has consumed a carbohydrate-containing food. eTABLE 41–2 NUTRITIONAL THERAPY *For 1000 calories, omit 1 fruit exchange and change low-fat milk to skim milk. For 1500 calories, add 1 meat, 1 fruit, and 2 fat exchanges; change low-fat milk to whole milk. For 1800 calories, add 2 bread, 3 meat, 3 fat, and 1 fruit exchanges; change low-fat milk to whole milk. †One extra fat exchange allowed for each cup of 2% low-fat milk; 2 extra fat exchanges allowed for each cup of skim milk. Table 41-1 shows the classification of overweight and obesity by BMI. The BMI, which provides an overall assessment of fat mass, must be considered in relation to the patient’s age, gender, and body build. For example, a body builder may have a BMI associated with obesity but because of a high muscle mass, the BMI would not be an accurate assessment. In contrast, in individuals who have lost body mass (e.g., older adults), the BMI would underestimate the degree of obesity. For this reason, other measures must be combined with the BMI for an accurate evaluation of a person’s weight. TABLE 41-1 CLASSIFICATION OF OVERWEIGHT AND OBESITY *Disease risk for type 2 diabetes, hypertension, and cardiovascular disease relative to person of normal weight. †Increased waist circumference can also be a marker for increased risk in persons of normal weight. Source: National Heart, Lung, and Blood Institute: Classification of overweight and obesity by BMI, waist circumference, and associated disease risks. Retrieved from www.nhlbi.nih.gov/health/public/heart/obesity/lose_wt/bmi_dis.htm. Waist circumference is another way to assess and classify a person’s weight (see Table 41-1). People who have visceral fat with truncal obesity are at an increased risk for cardiovascular disease and metabolic syndrome (discussed later in this chapter). Health risks increase if the waist circumference is greater than 40 inches in men and greater than 35 inches in women.1 Body shape is another method of identifying those who are at a higher risk for health problems (Table 41-2). Individuals with fat located primarily in the abdominal area, an apple-shaped body, have android obesity. Those with fat distribution in the upper legs, a pear-shaped body, have gynoid obesity. Genetics has an important role in determining a person’s body shape. Weight and shape are influenced by genetics.3 TABLE 41-2 RELATIONSHIP BETWEEN BODY SHAPE AND HEALTH RISKS Currently, more than 35% of adults in the United States are obese. Unless Americans change their ways, 50% of the U.S. population will be obese by 2030.4 Women having a slightly higher incidence of obesity than men. When those who are overweight are included, the incidence of the adult population with a BMI greater than 25 kg/m2 increases to more than 68%.5 The highest prevalence of obesity occurs between ages 40 and 59 for women and after 60 years of age for men.5 African Americans have the highest incidence of obesity followed by Hispanics (see Cultural & Ethnic Health Disparities box above). Obesity in adulthood is often a problem that begins in childhood or adolescence. Nearly one third of children and teens are currently obese or overweight. It is estimated that almost half of overweight adults were overweight in childhood, and two thirds of obese children remained obese into adulthood.6 Reversing the childhood obesity crisis is key to addressing the overall obesity epidemic. In obesity, there is an increase in the number of adipocytes (hyperplasia) and an increase in their size (hypertrophy). Adipocyte hypertrophy is a process by which adipocytes can increase their volume several thousand–fold to accommodate large increases in lipid storage. In addition, preadipocytes are triggered to become adipocytes once storage of existing fat cells is exceeded.2 This process primarily occurs in the visceral (intraabdominal) and subcutaneous tissues. The process of hyperplasia (increase in numbers) of adipocytes is greatest from infancy through adolescence. Studies of twins, adoptees, and families all suggest the existence of genetic factors in obesity.7,8 The heritability of obesity estimated from twin studies is high, with only slightly lower values in twins raised apart than in those raised together. Similarly, in adoptees the children’s BMI correlated with that of their biologic parents rather than their adoptive parents.9 Estimates of obesity as an inherited problem are more than 50%.8 A number of genes have been identified as being linked to obesity. Genes actually may influence how calories are stored and energy released. “Energy-thrifty” genes, once protective against long periods where food was not available, are now maladaptive in societies where food availability is no longer a primary issue.7 Genes may be responsible for why two individuals living in the same environment can vary considerably in body size. A strong link exists between a gene known as FTO (fat mass and obesity-associated gene) and BMI. Variants of this gene may explain why some people become overweight whereas others do not. People with two copies of a certain allele at the FTO gene weigh 7 to 8 lb more and have a greater risk of obesity than those who do not have the risk allele.10 More research is needed to better understand the role of genes in obesity. The hypothalamus, gut, and adipose tissue synthesize hormones and peptides that inhibit or stimulate the appetite (Fig. 41-3). The hypothalamus is a major site for regulating appetite. Neuropeptide Y, produced in the hypothalamus, is a powerful appetite stimulant. When it is imbalanced, it leads to overeating and obesity. Hormones and peptides produced in the gut and adipocyte cells affect the hypothalamus and have a critical role in appetite and energy balance (Table 41-3). TABLE 41-3 HORMONES AND PEPTIDES IN OBESITY Leptin, secreted from adipocytes when they fill with fat, acts in the hypothalamus to suppress appetite, increase physical activity, and increase fat metabolism. A genetic deficiency of leptin causes extreme obesity. In obesity the level of leptin is actually increased, which has raised the question of whether obese people are insensitive to leptin.2 Possible causes include failure to produce enough leptin receptors or production of receptors that are faulty. An increased release of cytokines from fat cells may disrupt immune factors, thus predisposing the person to certain cancers. Because visceral fat accumulation is associated with more alterations of these adipokines, people with abdominal obesity have more complications of obesity.11 Environmental factors play an important role in obesity. In today’s culture, people have greater access to food, particularly prepackaged and fast foods, and soft drinks, which have poor nutritional quality. Portion size of meals has increased dramatically (Table 41-4). The Centers for Disease Control and Prevention has developed visual programs that demonstrate how portions have increased over time.12 Underestimating portion sizes and therefore caloric intake is common. In addition, eating outside of the home interferes with the ability to control the quality and quantity of food. TABLE 41-4 PORTION SIZES: YESTERDAY VS TODAY Socioeconomic status is a known risk factor for obesity in a variety of ways.13 People with low incomes may attempt to stretch their food dollars by purchasing less expensive foods that often have poor nutritional quality with a greater caloric content. For example, people with low incomes are more likely to purchase pasta, bread, and canned fruit packed with sugar rather than chicken and fresh fruits and vegetables. Low-income residents may also live in environments that do not accommodate outdoor activities (e.g., safe playgrounds, walking tracks, tennis, swimming pools). People use food for many reasons besides their nutritional value. Associations with food begin in childhood, such as the use of food for comfort or rewards. Furthermore, when overeating develops at an early age and continues into adulthood, one’s ability to sense fullness (satiety) is compromised. Whether triggered by specific foods or by the wide variety of choices, some people consume more food than their bodies need. The lack of hunger that drives eating has been termed “mindless eating” and leads to consumption of unnecessary calories and increase in body weight.13,14 Hippocrates wrote that “corpulence is not only a disease itself, but the harbinger of others,” thus recognizing that obesity has major adverse effects on health. Many problems occur in obese people at higher rates than people of normal weight (Fig. 41-4). The medical cost of adult obesity in the United States is difficult to calculate, but estimates range from $147 billion to nearly $210 billion per year. The bulk of the spending is from treating obesity-related diseases such as diabetes. Obese people spend 42% more on health care costs than healthy-weight people.4 Mortality rates rise as obesity increases, especially when obesity is associated with visceral fat. For obese persons, mortality rates from all causes, especially from cardiovascular disease, are increased by 50% to 100% above those of persons with a normal BMI. Being overweight in midlife, once thought to have fewer health consequences than being obese, confers a 20% to 40% increase in mortality rate for both men and women.11 In addition to these problems, obese patients have a reduced quality of life. Fortunately, most of these conditions can improve if an individual loses weight. Obesity is a significant risk factor for cardiovascular disease in both men and women.11 Android obesity is the best predictor of these risks and is linked with increased low-density lipoproteins (LDLs), high triglycerides, and decreased high-density lipoproteins (HDLs). Obesity is also associated with hypertension, which can occur because of increased circulating blood volume, abnormal vasoconstriction, increased inflammation (damaging blood vessels), and increased risk of sleep apnea (raises blood pressure [BP]). Altered lipid metabolism and hypertension can increase the long-term risk of heart disease and stroke. Excess body fat can also lead to chronic inflammation throughout the body, especially in blood vessels, thus increasing the risk of heart disease. More than 80% of people with type 2 diabetes are obese or overweight.4 Hyperinsulinemia and insulin resistance, common features of type 2 diabetes, are also found in obesity, especially when visceral fat is increased. Excess weight decreases the effectiveness of insulin. When insulin does not work effectively, too much glucose stays in the bloodstream. Thus more insulin is made to compensate. Pancreatic β cells (cells that make insulin) may get overworked and become worn out. Over time, the pancreas is no longer able to keep blood glucose in normal range. It appears that adiponectin, a peptide that increases insulin sensitivity, is decreased in obese people. Obesity is a major risk factor for development of type 2 diabetes. Furthermore, obesity complicates the management of type 2 diabetes by increasing insulin resistance and glucose intolerance, which makes drug treatment for diabetes less effective. A weight reduction of 7% can decrease the risk of diabetes by 58%.15
Nursing Management
Obesity
Obesity
Classifications of Body Weight and Obesity
Body Mass Index.
Meal Plans for 1200–Calorie–Restricted Weight-Reduction Diet*
Meal
Exchanges
Meal Plan 1
Meal Plan 2
Meal Plan 3
Breakfast
1 meat
1 scrambled egg
1 hard-boiled egg
1 oz ham
2 bread
1 slice toast  cup dry cereal (unsweetened)
cup dry cereal (unsweetened)
1 flour tortilla  cup Cream of Wheat
cup Cream of Wheat
2 griddle cakes with diet syrup
1 fruit
 small banana
small banana
 cup orange juice
cup orange juice
 cup pineapple juice
cup pineapple juice
1 fat
1 tsp margarine
1 slice bacon
1 tsp margarine
1 dairy
1 cup low-fat milk
1 cup low-fat milk
1 cup low-fat milk
Beverage
Coffee
Coffee
Coffee
Lunch
2 meat
1 slice bologna
1 slice cheese
Cheese enchiladas (made with 2 oz cheese, 2 corn tortillas, chili sauce)
2 oz baked breaded pork chop
2 bread
2 slices bread
1 corn muffin
Vegetable
Lettuce, pickles
Tomato wedges
Spinach
1 fruit
Fresh grapes (12)
2 canned peach halves (packed in water)
Fresh orange
Beverage
Diet soda
Artificially sweetened lemonade
Unsweetened iced tea
Dinner
2 meat
1 oz roast beef
Chili con carne (made with  cup ground beef,
cup ground beef,  cup pinto beans, and chili powder)
cup pinto beans, and chili powder)
2 oz baked chicken
1 bread
Baked potato with 1 tsp margarine†
Corn on the cob with 1 tsp margarine
Vegetable
Cooked carrots
Tossed salad and 1 Tbsp salad dressing†
Okra
1 fruit
 cup strawberries
cup strawberries
Fresh apple
Fruit cocktail (packed in water)
1 milk
1 cup low-fat milk
1 cup low-fat milk
1 cup low-fat milk
Disease Risk Based on Waist Circumference*
BMI (kg/m2)
Obesity Class
Men ≤40 in (102 cm)
Women ≤35 in (89 cm)
Men >40 in (102 cm)
Women >35 in (89 cm)
Underweight
<18.5
—
—
—
Normal†
18.5-24.9
—
—
—
Overweight
25.0-29.9
—
Increased
High
Obese
30.0-34.9
Class I
High
Very high
35.0-39.9
Class II
Very high
Very high
Severely obese
≥40.0
Class III
Extremely high
Extremely high
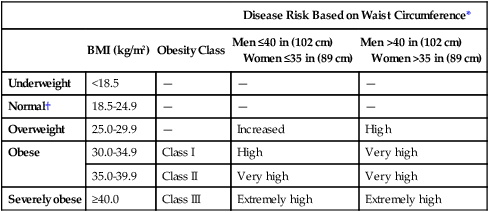
Waist Circumference.
Body Shape.
Body Shape
Characteristics
Health Risks
Gynoid (pear)

Android (apple)
Epidemiology of Obesity
Etiology and Pathophysiology
![]() Genetic Link
Genetic Link
Physiologic Regulatory Mechanisms in Obesity.
Where Produced
Normal Function
Alteration in Obesity
Neuropeptide Y
Hypothalamus
Stimulates appetite
Imbalance causes increased appetite.
Ghrelin
Stomach (primarily)
Stimulates appetite
↑ After food deprivation
↓ In response to food in the stomach
Normal postprandial decline does not occur, which can lead to increased appetite and overeating.
Leptin
Adipocytes
Suppresses appetite and hunger
Regulates eating behavior
Obesity is associated with high levels. Leptin resistance develops; thus obese people may lose the effect of appetite suppression.
Insulin
Pancreas
Decreases appetite
Increased insulin secretion which stimulates ↑ liver synthesis of triglycerides and ↓ HDL production.
Peptide YY
Colon
Inhibits appetite by slowing GI motility and gastric emptying
Circulating levels are decreased. ↓ Release after eating.
Cholecystokinin
Duodenum
Jejunum
Inhibits gastric emptying and sends satiety signals to hypothalamus
Unknown role
Environmental Factors.
25 Yr Ago
Today
Turkey sandwich
320 cal

820 cal

Bagel
3-in diameter, 140 cal

6-in diameter, 350 cal

Cheeseburger
333 cal

590 cal

Soda
6½ oz, 85 cal

20 oz, 250 cal

Psychosocial Factors.
Health Risks Associated with Obesity
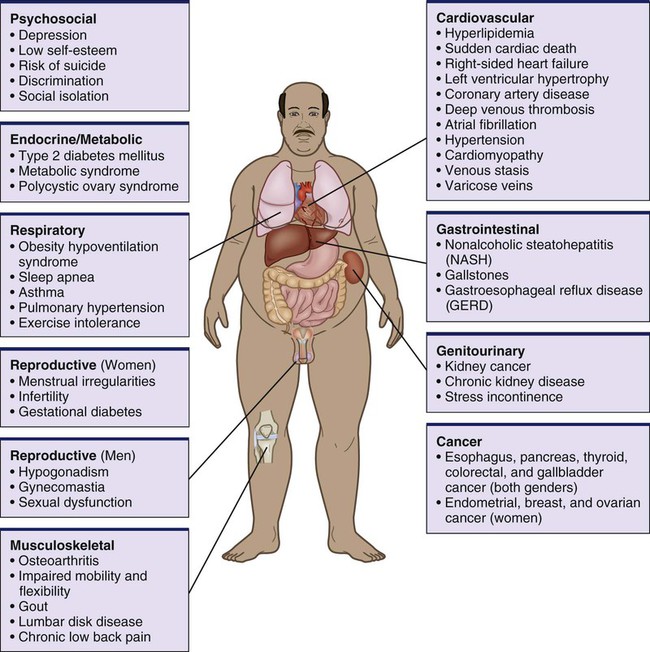
Cardiovascular Problems
Diabetes Mellitus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Management: Obesity
Get Clinical Tree app for offline access