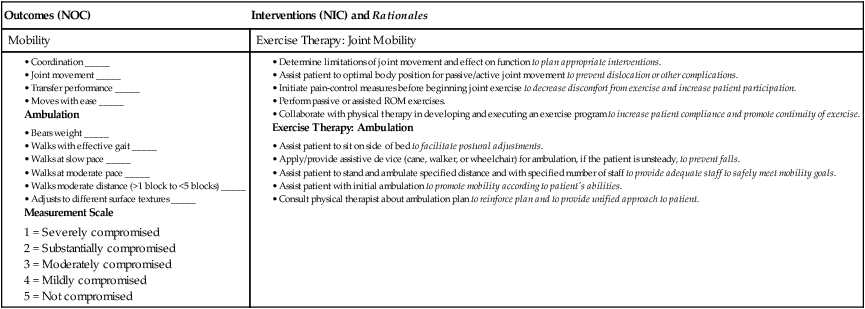
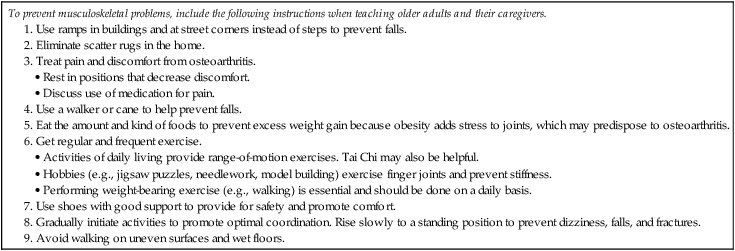
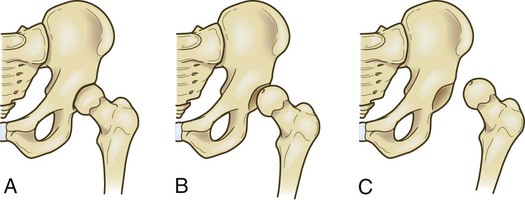
Chapter 63 1. Differentiate among the etiology, pathophysiology, clinical manifestations, and collaborative care of soft tissue injuries, including strains, sprains, dislocations, subluxations, bursitis, repetitive strain injury, carpal tunnel syndrome, and injuries to the rotator cuff, meniscus, and anterior cruciate ligament. 2. Relate the sequential events involved in fracture healing. 3. Compare closed reduction, cast immobilization, open reduction, and traction in terms of purpose, complications, and nursing management. 4. Evaluate the neurovascular assessment of an injured extremity. 5. Explain common complications associated with a fracture and fracture healing. 6. Describe the collaborative care and nursing management of patients with various kinds of fractures. 7. Describe the indications for and the collaborative care and nursing management of the patient with an amputation. 8. Describe the types of joint replacement surgery for arthritis and connective tissue disorders. 9. Prioritize the preoperative and postoperative management of the patient having joint replacement surgery. The most common cause of musculoskeletal injuries is a traumatic event resulting in fracture, dislocation, and/or soft tissue injuries. Although most of these injuries are not fatal, the cost in terms of pain, disability, medical expense, and lost wages is enormous. For all age-groups, accidents are exceeded only by heart disease, cancer, chronic lower respiratory tract diseases, and strokes as a cause of death.1 Accidental injuries (e.g., motor vehicle collisions, drowning, burns) are the leading cause of death in young adults in the United States. Ways to prevent common musculoskeletal problems in the older adult are listed in Table 63-1. TABLE 63-1 PATIENT & CAREGIVER TEACHING GUIDE Soft tissue injuries, which include sprains, strains, dislocations, and subluxations, are usually caused by trauma. The increasing number of people involved in a fitness program or participating in sports has contributed to the increased incidence of soft tissue injuries. Common sports-related injuries are summarized in Table 63-2. The most common sports injuries that result in a visit to the emergency department for younger patients are bruises, sprains and strains, tendinitis, and fractures.2 TABLE 63-2 A sprain is an injury to the ligamentous structures surrounding a joint, usually caused by a wrenching or twisting motion. Most sprains occur in the ankle, wrist, and knee joints.3 A sprain is classified according to the degree of ligament damage. A first-degree (mild) sprain involves tears in only a few fibers, resulting in mild tenderness and minimal swelling. A second-degree (moderate) sprain is partial disruption of the involved tissue with more swelling and tenderness. A third-degree (severe) sprain is complete tearing of the ligament in association with moderate to severe swelling. A gap in the muscle may be apparent or palpated through the skin if the muscle is torn. Because areas around joints are rich in nerve endings, the injury can be extremely painful. Warming up muscles before exercising and vigorous activity, followed by stretching, may significantly reduce the risk of sprains and strains. Strength, balance, and endurance exercises are also important. Strengthening exercises that involve working against resistance build up muscle strength and bone density. Balance exercises, which may overlap with some strengthening exercises, help to prevent falling. Endurance exercises should start at a low level of effort and progress gradually to a moderate level.4 Exercise instructions for these types of physical activity are available at www.weboflife.ksc.nasa.gov/exerciseandaging. If an injury occurs, the immediate care focuses on (1) stopping the activity and limiting movement, (2) applying ice compresses to the injured area, (3) compressing the involved extremity, (4) elevating the extremity, and (5) providing analgesia as necessary (Table 63-3). EMERGENCY MANAGEMENT Dislocations characteristically result from forces transmitted to the joint that disrupt the soft tissue support structures surrounding it. The joints most frequently dislocated in the upper extremity include the thumb, elbow, and shoulder. In the lower extremity, the hip is vulnerable to dislocation as a result of severe trauma, often associated with motor vehicle collisions (Fig. 63-1). The patella may dislocate because of a sharp blow to the kneecap or after a sudden twisting inward motion while the planted foot is pointed outward.5 A dislocation requires prompt attention and is often considered an orthopedic emergency. It may be associated with significant vascular injury. The longer the joint remains unreduced, the greater the possibility of avascular necrosis. The hip joint is particularly susceptible to avascular necrosis. Compartment syndrome (discussed on p. 1522) may also occur after a dislocation. Neurovascular assessment is critical (see pp. 1517–1518).
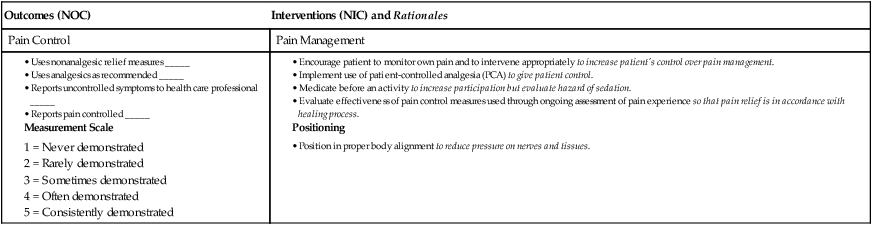
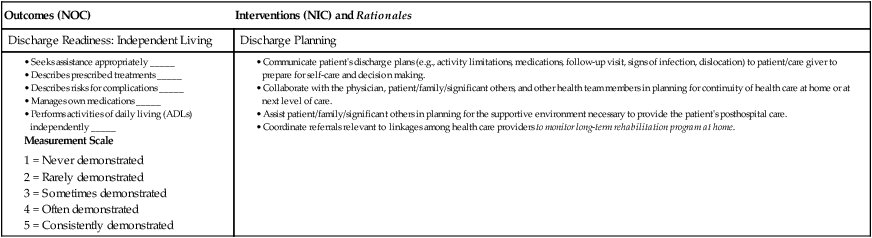
Nursing Management
Musculoskeletal Trauma and Orthopedic Surgery
Prevention of Musculoskeletal Problems in Older Adults
Soft Tissue Injuries
Injury
Description
Treatment
Impingement syndrome
Entrapment of soft tissue structures under coracoacromial arch of shoulder.
NSAIDs. Rest until symptoms decrease and then gradual ROM and strengthening exercises.
Rotator cuff tear
Tear within muscle or tendinoligamentous structures around shoulder.
If minor tear: Rest, NSAIDs, and gradual mobilization with ROM and strengthening exercises.
If major tear: Surgical repair.
Shin splints
Inflammation along anterior aspect of calf from periostitis caused by improper shoes, overuse, or running on hard pavement.
Rest, ice, NSAIDs, proper shoes. Gradual increase in activity.
If pain persists, x-ray to rule out stress fracture of tibia.
Tendinitis
Inflammation of tendon as a result of overuse or incorrect use.
Rest, ice, NSAIDs. Gradual return to sport activity. Protective brace (orthosis) may be necessary if symptoms recur.
Ligament injury
Tearing or stretching of ligament. Usually occurs as a result of inversion, eversion, shearing, or torque applied to a joint.
Characterized by sudden pain, swelling, and instability.
Rest, ice, elevation of extremity if possible, NSAIDs. Protection of affected extremity by use of brace. If symptoms persist, surgical repair may be necessary.
Meniscus injury
Injury to fibrocartilage of knee characterized by popping, clicking, tearing sensation, effusion, and/or swelling.
Rest, ice, elevation of extremity if possible, NSAIDs. Gradual return to regular activities.
If symptoms persist, MRI to diagnose meniscus injury and possible arthroscopic surgery.
Anterior cruciate ligament tear
Traumatic tearing of ligament by deceleration forces together with pivoting or odd positions of the knee or leg.
Physical therapy with rehabilitation, knee brace.
If knee instability or continued injuries, reconstructive surgery may be done.
Sprains and Strains
Nursing Management Sprains and Strains
Nursing Implementation
Health Promotion.
Acute Intervention.
![]() TABLE 63-3
TABLE 63-3
Acute Soft Tissue Injury
Dislocation and Subluxation
Nursing and Collaborative Management Dislocation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access