Chapter 66 Linda Bucher and Maureen A. Seckel 1. Differentiate the various certification opportunities for critical care nurses. 2. Select appropriate nursing interventions to manage common problems and needs of critically ill patients. 3. Develop strategies to manage issues related to caregivers of critically ill patients. 4. Apply the principles of hemodynamic monitoring to the collaborative care and nursing management of patients receiving this intervention. 5. Differentiate the purpose of, indications for, and function of circulatory assist devices and related collaborative care and nursing management. 6. Differentiate the indications for and modes of mechanical ventilation. 7. Select appropriate nursing interventions related to the care of an intubated patient. 8. Relate the principles of mechanical ventilation to the collaborative care and nursing management of patients receiving this intervention. The American Association of Critical-Care Nurses (AACN) defines critical care nursing as that specialty dealing with human responses to life-threatening problems.1 Critical care nurses care for patients with acute and unstable physiologic problems, and their caregivers. This involves assessing life-threatening conditions, initiating appropriate interventions, evaluating the outcomes of the interventions, and providing education and emotional support to caregivers. Critical care units (CCUs) or intensive care units (ICUs) are designed to meet the special needs of acutely and critically ill patients. In many hospitals the concept of ICU care has expanded from delivering care in a standard unit to bringing ICU care to patients wherever they might be. For example, the electronic or teleICU assists the bedside ICU team by monitoring the patient from a remote location (Fig. 66-1). Similarly, the development of rapid response teams (RRTs) provides for the delivery of advanced care by specialized teams usually composed of a critical care nurse, a respiratory therapist, and a critical care physician or an advanced practice registered nurse (APRN). The team brings rapid and immediate care to unstable patients in noncritical care units. Patients often exhibit early and subtle signs of deterioration (e.g., mild confusion, tachypnea) 6 to 8 hours before cardiac or respiratory arrest. Early critical care intervention has made significant contributions to reducing mortality rates in these patients.2 The technology available in the ICU is extensive and always evolving. It is possible to continuously monitor the electrocardiogram (ECG), blood pressure (BP), oxygen (O2) saturation, cardiac output (CO), intracranial pressure, and temperature. More advanced monitoring devices measure cardiac index (CI), stroke volume (SV), stroke volume variation (SVV), ejection fraction (EF), end-tidal carbon dioxide (CO2), and tissue O2 consumption. Patients may receive ongoing support from mechanical ventilators, intraaortic balloon pumps (IABPs), circulatory assist devices (CADs), or dialysis machines. Fig. 66-2 shows a typical ICU. Advanced practice critical care nurses currently have a graduate (master’s or doctorate) degree with a proposed transition to a doctor of nursing practice (DNP) by 2015.3 These nurses function in a variety of roles: patient and staff educators, consultants, administrators, researchers, or expert practitioners. The advanced practice critical care nurse who is a clinical nurse specialist (CNS) typically functions in one or more of these roles. Certification for the CNS in acute and critical care is available through the AACN. Another advanced practice role is the acute care nurse practitioner (ACNP). This APRN provides comprehensive care to select critically ill patients and their caregivers. The ACNP conducts comprehensive assessments, orders and interprets diagnostic tests, manages health problems and disease-related symptoms, prescribes treatments, and coordinates care during transitions in settings. Certification as an ACNP is available through the AACN. Prescriptive authority and licensure regulations for APRNs vary by state. AACN defines a critically ill patient as one who is at high risk for actual or potential life-threatening health problems and who requires intense and vigilant nursing care.1 A patient is generally admitted to the ICU for one of three reasons. First, the patient may be physiologically unstable, requiring advanced clinical judgments by you and a physician. Second, the patient may be at risk for serious complications and require frequent assessments and often invasive interventions. Third, the patient may require intensive and complicated nursing support related to the use of IV polypharmacy (e.g., sedation, thrombolytics, drugs requiring titration [e.g., vasopressors]) and advanced technology (e.g., mechanical ventilation, intracranial pressure monitoring, continuous renal replacement therapy, hemodynamic monitoring). Despite the emphasis on caring for patients who are expected to survive, the incidence of death is higher in ICU patients than in non-ICU patients. In general, nonsurvivors are older, have co-morbidities (e.g., liver disease, obesity), and experience longer ICU stays.4 Consequently, it is important that you are skilled in palliative and end-of-life care (see Chapter 10). The patient admitted to the ICU is at risk for numerous complications and special problems. Critically ill patients are usually immobile and at high risk for skin problems (see Chapter 24) and venous thromboembolism (see Chapter 38). The use of multiple, invasive devices predisposes the patient to health care–associated infections (HAIs). Sepsis and multiple organ dysfunction syndrome (MODS) may follow (see Chapter 67). Adequate nutrition for the critically ill patient is essential. Other special problems relate to anxiety, pain, impaired communication, sensory-perceptual problems, and sleep disorders. Patients often arrive at ICUs with conditions that result in either hypermetabolic states (e.g., burns, sepsis) or catabolic states (e.g., acute kidney injury). Other times, patients are in severely malnourished states (e.g., chronic heart, pulmonary, or liver disease). In general, inadequate nutrition is linked to increased mortality and morbidity rates. One contributing factor to underfeeding patients is the frequent interruptions in enteral feedings because of medication administration and multiple tests and procedures. Determining who to feed, what to feed, when to feed, and how to feed (e.g., route of administration) is crucial when caring for critically ill patients.5 Collaborate with the physician and the dietitian to determine how best to meet the nutritional needs of ICU patients. The primary goal of nutritional support is to prevent or correct nutritional deficiencies. This is usually done by the early provision of enteral nutrition (i.e., delivery of calories via the gastrointestinal [GI] tract) or parenteral nutrition (i.e., IV delivery of calories).5 Enteral nutrition preserves the structure and function of the gut mucosa and stops the movement of gut bacteria across the intestinal wall and into the bloodstream. In addition, early enteral nutrition is associated with fewer complications and shorter hospital stays and is less expensive than parenteral nutrition.5 (Enteral and parenteral nutrition are discussed in Chapter 40.) To help reduce anxiety, encourage patients and caregivers to express concerns, ask questions, and state their needs. Include the patient and caregiver in all conversations and explain the purpose of equipment and procedures. Be sure to structure the patient’s environment in a way that decreases anxiety. For example, encourage caregivers to bring in photographs and personal items. Appropriate use of antianxiety drugs (e.g., lorazepam [Ativan]) and relaxation techniques (e.g., music therapy) may reduce the stress response that can be triggered by anxiety.6 The control of pain in the ICU patient is vital. As many as 70% of ICU patients have moderate to severe unrelieved pain. Inadequate pain control is often linked with agitation and anxiety and is known to add to the stress response. ICU patients at high risk for pain include those who (1) have medical conditions that include ischemic, infectious, or inflammatory processes; (2) are immobilized; (3) have invasive monitoring devices, including endotracheal tubes; and (4) require invasive or noninvasive procedures.7 For some critically ill patients (e.g., those needing mechanical ventilation), continuous IV sedation (e.g., propofol [Diprivan]) and an analgesic agent (e.g., fentanyl [Sublimaze]) are effective strategies for sedation and pain control. However, patients getting deep sedation are unresponsive. This prevents you and other health care providers from fully assessing the patient’s neurologic status. To address this problem, guidelines should include a daily, scheduled interruption of sedation, or “sedation holiday.” These daily interruptions allow you to awaken the patient to conduct a neurologic examination.8 (Pain management is discussed in Chapter 9.) Inability to communicate is distressing for patients who cannot speak because of the use of sedative and paralyzing drugs or an endotracheal tube. As part of every procedure, explain what will happen or is happening to the patient. When the patient cannot speak, explore alternative methods of communication, such as picture boards, notepads, magic slates, or computer keyboards. When speaking with the patient, look directly at the patient and use hand gestures when appropriate. For patients and caregivers who do not speak English, an approved translator or translator phone service must be provided (see Chapter 4). Acute and reversible sensory-perceptual changes are common in ICU patients. The combination of alterations in mentation (e.g., delusions, short attention span, loss of recent memory), psychomotor behavior (e.g., restlessness, lethargy), and sleep-wake cycle (e.g., daytime sleepiness, nighttime agitation) has been inappropriately called ICU psychosis. The patient experiencing these changes is not psychotic but is suffering from delirium. It is estimated that the prevalence of delirium in ICU patients is as high as 80%.9 Significant risk factors for delirium include preexisting dementia, history of baseline hypertension or alcohol abuse, and severe illness on admission. Environmental factors that can contribute to delirium include sleep deprivation, anxiety, sensory overload, and immobilization. Physical conditions such as hemodynamic instability, hypoxemia, hypercarbia, electrolyte disturbances, and severe infections can lead to delirium. Last, certain drugs (e.g., sedatives [benzodiazepines], analgesics [opioids], and antimicrobials [aminoglycosides]) have been linked with the development of delirium.9 (Chapter 60 discusses delirium.) Monitor all ICU patients for delirium. Assessment tools include the Confusion Assessment Method for the ICU and the Intensive Care Delirium Screening Checklist9 (both available at www.icudelirium.org). It is critical to address physiologic factors (e.g., correction of oxygenation, perfusion, and electrolyte problems). The use of clocks and calendars can help orient the patient. If the patient demonstrates hyperactivity, insomnia, or delusions, management with sedative drugs with anxiolytic effects (e.g., dexmedetomidine [Precedex]) can be considered.9 In addition, the presence of a caregiver may help orient the patient and reduce agitation. (See eTable 66-1 on the website for this chapter.) Sensory overload can also result in patient distress and anxiety. Environmental noise levels are particularly high in the ICU.10 You can limit noise and assist the patient in understanding noises that cannot be prevented. Conversation is a particularly stressful noise, especially when the discussion concerns the patient and is held in the presence of, but without participation from, the patient.10 Reduce this source of stress by finding suitable places for patient-related discussions. Whenever possible, include the patient or the caregiver in the discussion.
Nursing Management
Critical Care
Critical Care Nursing
Critical Care Units
Critical Care Nurse
Critical Care Patient
Common Problems of Critical Care Patients.
Nutrition.
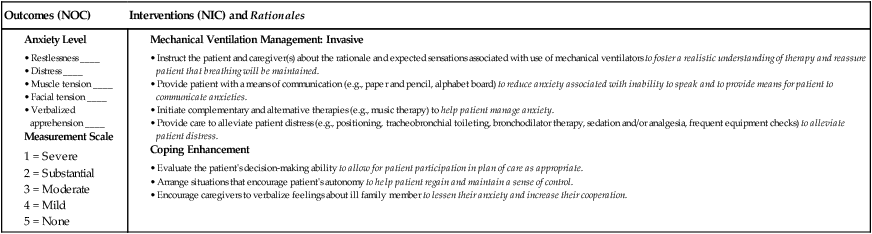
Anxiety.
Pain.
Impaired Communication.
Sensory-Perceptual Problems.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Management: Critical Care
Get Clinical Tree app for offline access