Chapter 59 1. Compare and contrast the etiology, clinical manifestations, collaborative care, and nursing management of tension-type, migraine, and cluster headaches. 2. Differentiate the etiology, clinical manifestations, diagnostic studies, collaborative care, and nursing management of seizure disorders, multiple sclerosis, Parkinson’s disease, and myasthenia gravis. 3. Describe the clinical manifestations and nursing and collaborative management of restless legs syndrome, amyotrophic lateral sclerosis, and Huntington’s disease. 4. Explain the potential impact of chronic neurologic disease on physical and psychologic well-being. 5. Outline the major goals of treatment for the patient with a chronic, progressive neurologic disease. 1. Reports satisfaction with pain relief 2. Uses pharmacologic and nonpharmacologic measures appropriately to manage pain Experiences breathing pattern adequate to meet oxygen needs • Monitor respiratory and oxygenation status to determine presence and extent of breathing problem and to initiate appropriate interventions. • Position patient (side-lying) to maximize ventilation potential and decrease risk of aspiration. • Identify patient requiring actual/potential airway insertion to facilitate intubation as necessary. • Perform endotracheal or nasotracheal suctioning to maintain airway. Experiences no seizure-related injury 1. Expresses acceptance of seizure disorder by admitting presence of epilepsy and maintaining compliant behavior 1. Describes factors involved in effective management of seizure disorder 2. Makes decisions about health and lifestyle modifications necessary for management of seizure disorder 1. Maintains or improves muscle strength and mobility 2. Uses assistive devices appropriately for ambulation and mobility 1. Maintains urinary continence 2. Experiences post-urination residual urine volume <50 mL 3. Uses intermittent catheterization to maintain urinary function if necessary 1. Maintains open communication within the family 2. Utilizes financial, social, and health services to maintain family processes 1. Describes activities required to manage the disease process 2. Makes decisions about health and lifestyle modifications necessary for management of multiple sclerosis 1. Performs physical exercise appropriately to deter muscle atrophy and joint contractures 2. Uses assistive devices appropriately for ambulation and mobility 1. Experiences safe passage of fluids and/or solids from the mouth to the stomach 2. Performs actions to prevent the passage of fluid and solid particles into the lung
Nursing Management
Chronic Neurologic Problems
Headaches
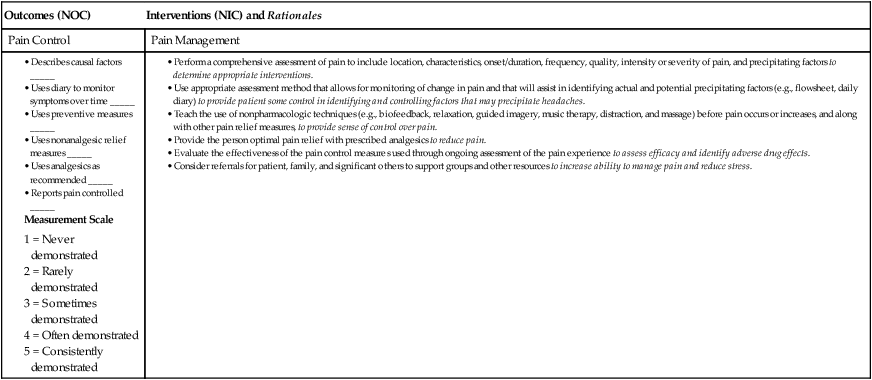
![]() eNursing Care Plan 59-1 Patient With Headache
eNursing Care Plan 59-1 Patient With Headache
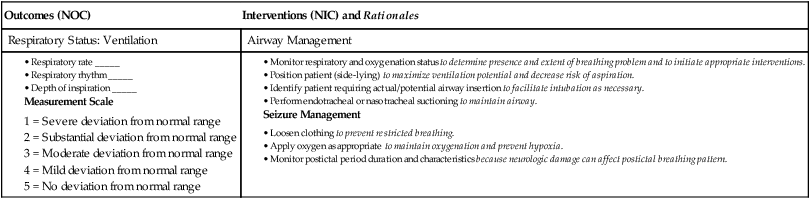
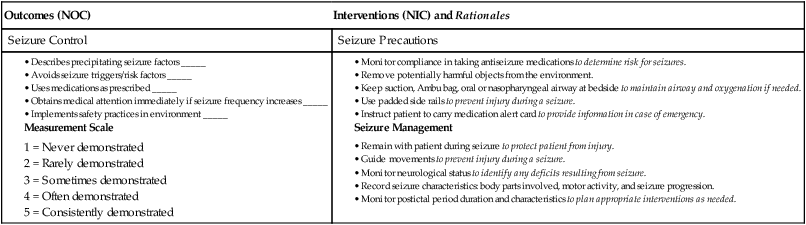
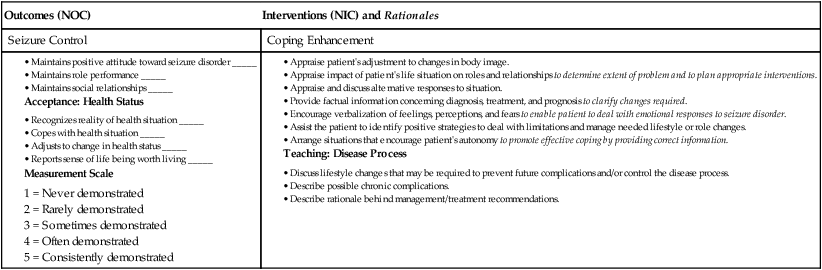
![]() eNursing Care Plan 59-2 Patient With Seizure Disorder or Epilepsy
eNursing Care Plan 59-2 Patient With Seizure Disorder or Epilepsy
Outcomes (NOC)
Interventions (NIC) and Rationales
Respiratory Status: Ventilation
Airway Management
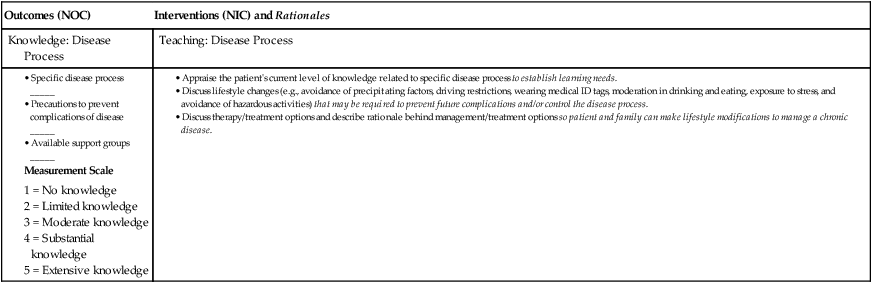
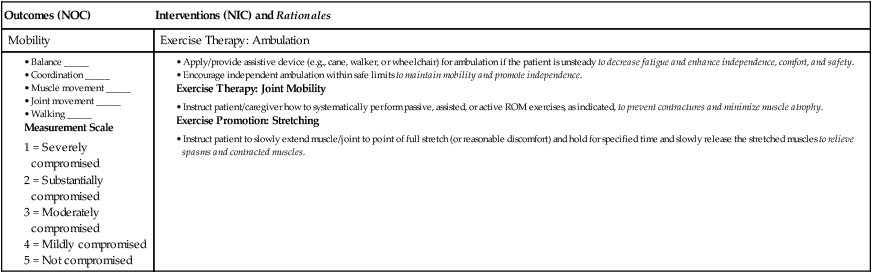
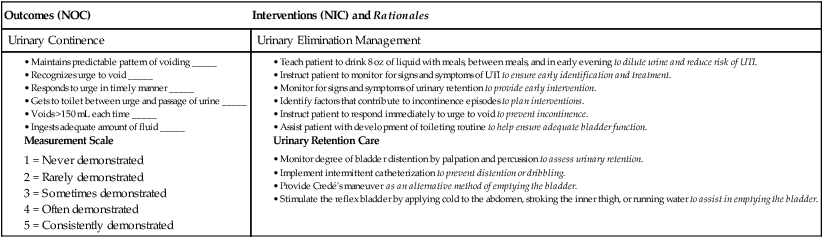
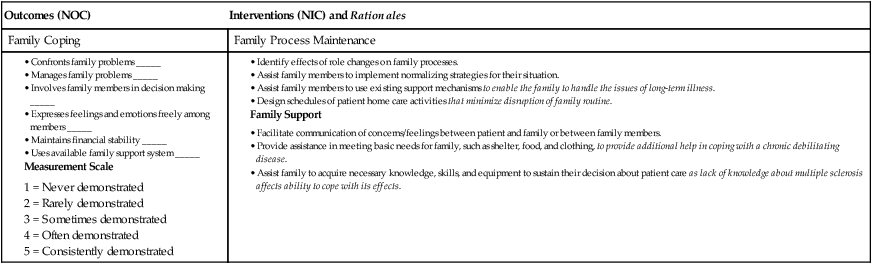
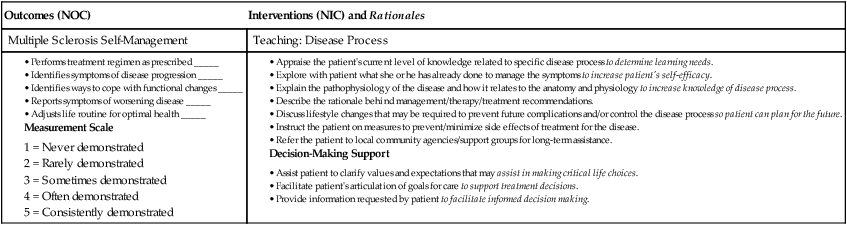
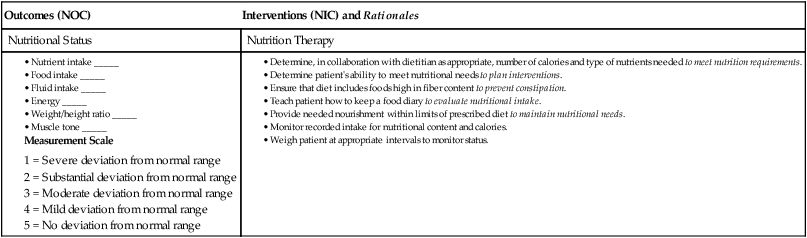
![]() eNursing Care Plan 59-3 Patient With Multiple Sclerosis
eNursing Care Plan 59-3 Patient With Multiple Sclerosis
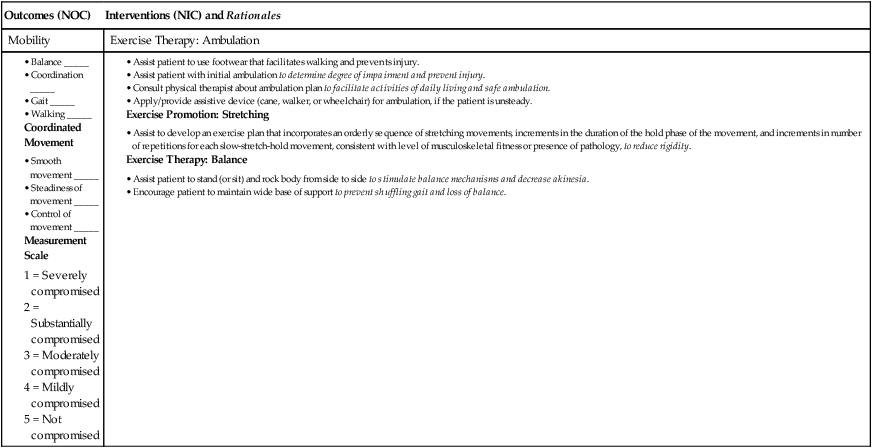
![]() eNursing Care Plan 59-4 Patient With Parkinson’s Disease
eNursing Care Plan 59-4 Patient With Parkinson’s Disease
Nursing Management: Chronic Neurologic Problems
Chapter 59 1. Compare and contrast the etiology, clinical manifestations, collaborative care, and nursing management of tension-type, migraine, and cluster headaches. 2. Differentiate the etiology, clinical manifestations, diagnostic studies, collaborative care, and nursing management of seizure disorders, multiple sclerosis, Parkinson’s disease, and myasthenia gravis. 3. Describe the clinical manifestations and nursing and collaborative management of restless legs syndrome, amyotrophic lateral sclerosis, and Huntington’s disease. 4. Explain the potential impact of chronic neurologic disease on physical and psychologic well-being. 5. Outline the major goals of treatment for the patient with a chronic, progressive neurologic disease.
Nursing Management
Chronic Neurologic Problems



