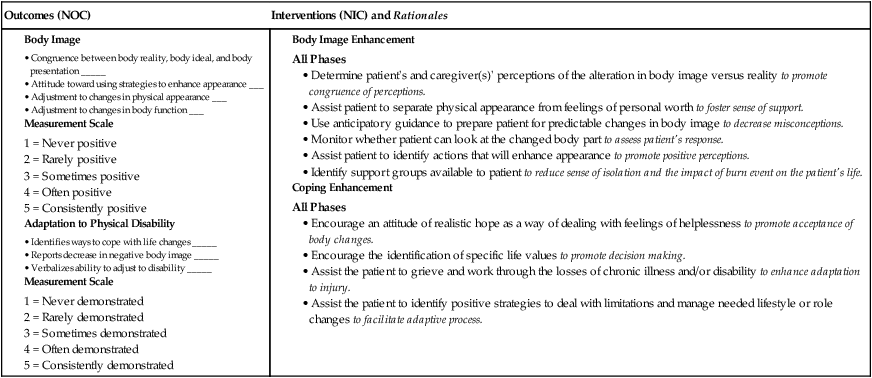
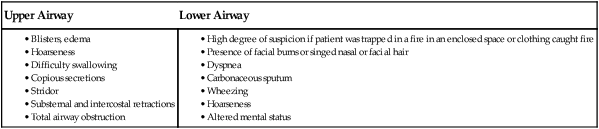
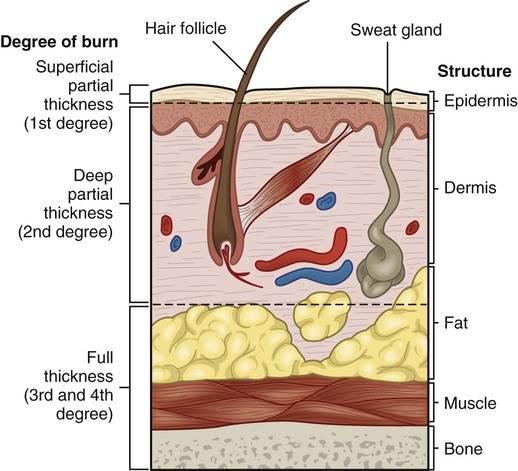
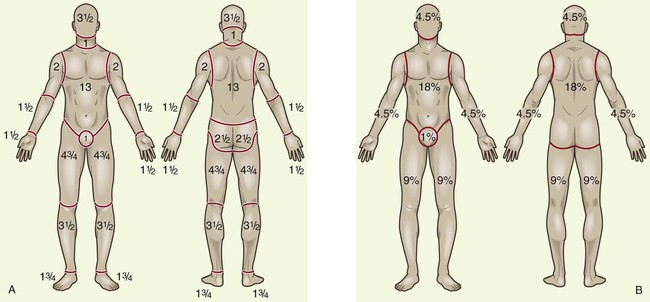
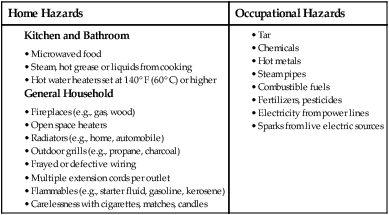
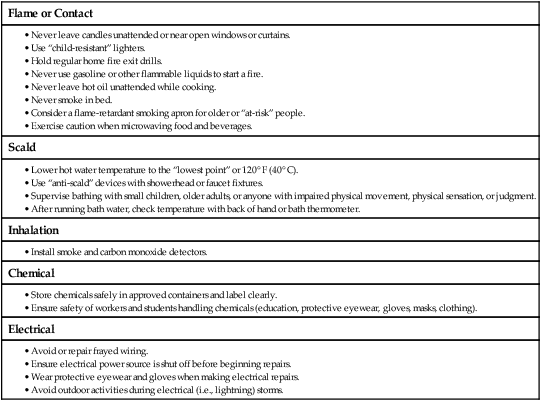
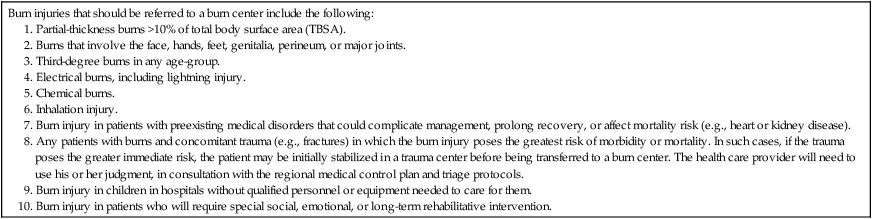
Chapter 25 1. Relate the causes of and prevention strategies for burn injuries. 2. Differentiate between partial-thickness and full-thickness burns. 3. Apply the tools used to determine the severity of burns. 4. Compare the pathophysiology, clinical manifestations, complications, and collaborative management throughout the three burn phases. 5. Compare the fluid and electrolyte shifts during the emergent and acute burn phases. 6. Differentiate the nutritional needs of the burn patient throughout the three burn phases. 7. Compare the various burn wound care techniques and surgical options for partial-thickness versus full-thickness burn wounds. 8. Prioritize nursing interventions in the management of the burn patient’s physiologic and psychosocial needs. 9. Examine the various physiologic and psychosocial aspects of burn rehabilitation. 10. Design a plan of care to prepare the burn patient and caregiver for discharge. An estimated 450,000 Americans seek medical care each year for burns.1,2 Approximately 45,000 people are hospitalized, one half of whom require care in specialized burn centers. About 3500 Americans die annually as a direct result of their injuries. The highest fatality rates occur in children ages 4 years and younger and adults over age 65. Around the world, nearly 11 million people need medical attention annually for burn injuries, and about 300,000 die.3 Although burn incidence has decreased over the past 20 years, burn injuries still occur too frequently and mainly to people at a lower socioeconomic level. Most burn incidents should be viewed as preventable. Today, the focus of burn prevention programs has shifted from blaming individuals and changing behaviors to making legislative changes and collecting global burn data to address the unique prevention needs of developing countries.4 Coordinated national programs in developed countries have focused on child-resistant lighters, nonflammable children’s clothing, tap water anti-scald devices, fire-safe cigarettes, stricter building codes, hardwired smoke detectors and alarms, and fire sprinklers. As a nurse, you can advocate for burn risk reduction strategies in the home and at work, and you can teach workers to reduce burn injuries in both settings (Tables 25-1 and 25-2). TABLE 25-1 TABLE 25-2 STRATEGIES TO REDUCE BURN INJURY Thermal burns, caused by flame, flash, scald, or contact with hot objects, are the most common type of burn injury (Fig. 25-1). The severity of the injury depends on the temperature of the burning agent and the duration of contact time. Scald injuries can occur in the bathroom or while cooking. Flash, flame, or contact burns can occur while cooking, smoking, burning leaves in the backyard, or using gasoline or hot oil. Smoke and inhalation injuries from breathing hot air or noxious chemicals can cause damage to the respiratory tract. Three types of smoke and inhalation injuries can occur: metabolic asphyxiation, upper airway injury, and lower airway injury. Because smoke inhalation injuries are a major predictor of mortality in burn patients, rapid assessment is critical.5 Upper airway injury results from an inhalation injury to the mouth, oropharynx, and/or larynx. The injury may be caused by thermal burns or the inhalation of hot air, steam, or smoke. Mucosal burns of the oropharynx and the larynx are manifested by redness, blistering, and edema (Table 25-3). The swelling can be massive and the onset rapid. Flame burns to the neck and the chest may make breathing more difficult because of the burn eschar, which becomes tight and constricting from the underlying edema. Swelling from scald burns to the face and the neck can also be lethal, as can external pressure from edema pressing on the airway. Mechanical obstruction can occur quickly, presenting a true medical emergency. An inhalation injury to the trachea, bronchioles, and alveoli is usually caused by breathing in toxic chemicals or smoke. Tissue damage is related to the duration of exposure to toxic fumes or smoke. Clinical manifestations of lower airway lung injury are presented in Table 25-3. Pulmonary edema may not appear until 12 to 24 hours after the burn, and then it may manifest as acute respiratory distress syndrome (ARDS) (see Chapter 68). Electrical burns result from intense heat generated from an electric current. Direct damage to nerves and vessels, causing tissue anoxia and death, can also occur. The severity of the electrical injury depends on the amount of voltage, tissue resistance, current pathways, surface area in contact with the current, and length of time that the current flow was sustained (Fig. 25-2). Tissue densities offer various amounts of resistance to electric current. For example, fat and bone offer the most resistance, whereas nerves and blood vessels offer the least resistance. Current that passes through vital organs (e.g., brain, heart, kidneys) produces more life-threatening sequelae than that which passes through other tissues. In addition, electric sparks may ignite the patient’s clothing, causing a flash injury. Electrical injury puts the patient at risk for dysrhythmias or cardiac arrest, severe metabolic acidosis, and myoglobinuria. The electric shock event can cause immediate cardiac standstill or ventricular fibrillation. Delayed cardiac dysrhythmias or arrest may also occur without warning during the first 24 hours after injury. Myoglobin from injured muscle tissue and hemoglobin from damaged red blood cells (RBCs) are released into the circulation whenever massive muscle and blood vessel damage occurs. The released myoglobin pigments travel to the kidneys and can block the renal tubules, which can result in acute tubular necrosis (ATN) and acute kidney injury (see Chapter 47). The treatment of burns is related to the severity of the injury.6 Severity is determined by (1) depth of burn, (2) extent of burn calculated in percent of total body surface area (TBSA), (3) location of burn, and (4) patient risk factors (e.g., age, past medical history). The American Burn Association (ABA) has established referral criteria to determine which burn injuries should be treated in burn centers with specialized facilities (Table 25-4). The majority of patients with minor burn injuries can be managed in community hospitals.7 TABLE 25-4 Source: Guidelines for the operation of burn centers. In American College of Surgeons, Committee on Trauma: Resources for optimal care of the injured patient, 2006. Retrieved from www.ameriburn.org/Chapter14.pdf. Burn injury involves the destruction of the integumentary system. The skin is divided into three layers: epidermis, dermis, and subcutaneous tissue (Fig. 25-3). The epidermis, or nonvascular protective outer layer of the skin, is approximately as thick as a sheet of paper. (The structure and function of the skin are discussed in Chapter 23.) Burns continue to be defined by degrees: first, second, third, and fourth degree. The ABA recommends a more precise definition and classifies burns according to depth of skin destruction: partial-thickness burns and full-thickness burns (see Fig. 25-3). Skin-reproducing (re-epithelializing) cells are located along the shafts of the hair follicles, sweat glands, and oil glands. If significant damage occurs to the dermis (i.e., a full-thickness burn), not enough skin cells remain to regenerate new skin. A permanent, alternative source of skin needs to be found. Table 25-5 compares the various burn classifications according to the depth of injury. TABLE 25-5 CLASSIFICATION OF BURN INJURY DEPTH Two commonly used guides for determining the TBSA affected or the extent of a burn wound are the Lund-Browder chart (Fig. 25-4, A) and the Rule of Nines (Fig. 25-4, B). (First-degree burns, equivalent to a sunburn, are not included when calculating TBSA.) The Lund-Browder chart is considered more accurate because it considers the patient’s age in proportion to relative body-area size. The Rule of Nines is often used for initial assessment of a burn patient because it is easy to remember. For irregular- or odd-shaped burns, the patient’s hand (including the fingers) is approximately 1% TBSA. The Sage Burn Diagram is a free, Internet-based tool for estimating TBSA burned (www.sagediagram.com). Burns to the ears and the nose are susceptible to infection because of poor blood supply to the cartilage. Burns to the buttocks or perineum are highly susceptible to infection from urine or feces contamination. Circumferential burns to the extremities can cause circulation problems distal to the burn, with possible nerve damage to the affected extremity. Patients may also develop compartment syndrome (see Chapter 63) from direct heat damage to the muscles, swelling, and/or preburn vascular problems. Any patient with preexisting cardiovascular, respiratory, or renal disease has a poorer prognosis for recovery because of the tremendous demands placed on the body by a burn injury. The patient with diabetes mellitus or peripheral vascular disease is at high risk for poor healing, especially with foot and leg burns.8 General physical debilitation from any chronic disease, including alcoholism, drug abuse, or malnutrition, makes it challenging for the patient to fully recover from a burn injury. In addition, the burn patient who has also sustained fractures, head injuries, or other trauma has a more difficult time recovering. Small thermal burns (10% or less of TBSA) should be covered with a clean, cool, tap water–dampened towel for the patient’s comfort and protection until medical care is available.9 Cooling of the injured area (if small) within 1 minute helps minimize the depth of the injury. If the burn is large (greater than 10% TBSA) or an electrical or inhalation burn is suspected, first focus your attention on the ABCs: • Airway: Check for patency, soot around nares and on the tongue, singed nasal hair, darkened oral or nasal membranes. • Breathing: Check for adequacy of ventilation. • Circulation: Check for presence and regularity of pulses, and elevate the burned limb(s) above the heart to decrease pain and swelling. Prehospital care and emergency management are presented in tables that describe thermal burns (Table 25-6), inhalation injury (Table 25-7), electrical burns (Table 25-8), and chemical burns (Table 25-9). EMERGENCY MANAGEMENT EMERGENCY MANAGEMENT
Nursing Management
Burns
Home Hazards
Occupational Hazards
Types of Burn Injury
Thermal Burns
Smoke and Inhalation Injury
Upper Airway Injury.
Lower Airway Injury.
Electrical Burns
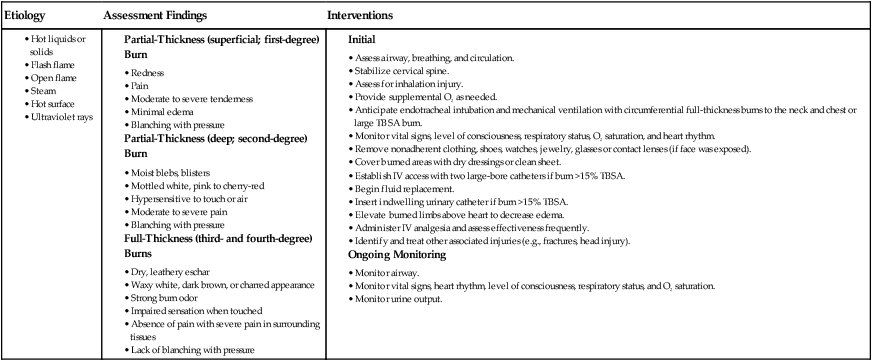
Classification of Burn Injury
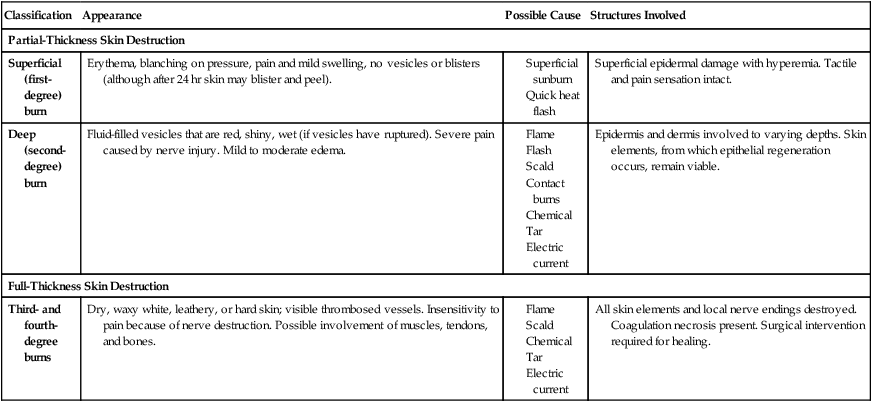
Depth of Burn
Classification
Appearance
Possible Cause
Structures Involved
Partial-Thickness Skin Destruction
Superficial (first-degree) burn
Erythema, blanching on pressure, pain and mild swelling, no vesicles or blisters (although after 24 hr skin may blister and peel).
Superficial epidermal damage with hyperemia. Tactile and pain sensation intact.
Deep (second-degree) burn
Fluid-filled vesicles that are red, shiny, wet (if vesicles have ruptured). Severe pain caused by nerve injury. Mild to moderate edema.
Epidermis and dermis involved to varying depths. Skin elements, from which epithelial regeneration occurs, remain viable.
Full-Thickness Skin Destruction
Third- and fourth-degree burns
Dry, waxy white, leathery, or hard skin; visible thrombosed vessels. Insensitivity to pain because of nerve destruction. Possible involvement of muscles, tendons, and bones.
All skin elements and local nerve endings destroyed. Coagulation necrosis present. Surgical intervention required for healing.
Extent of Burn
Location of Burn
Patient Risk Factors
Phases of Burn Management
Prehospital Care
![]() TABLE 25-6
TABLE 25-6
Thermal Burns
![]() TABLE 25-7
TABLE 25-7
Inhalation Injury