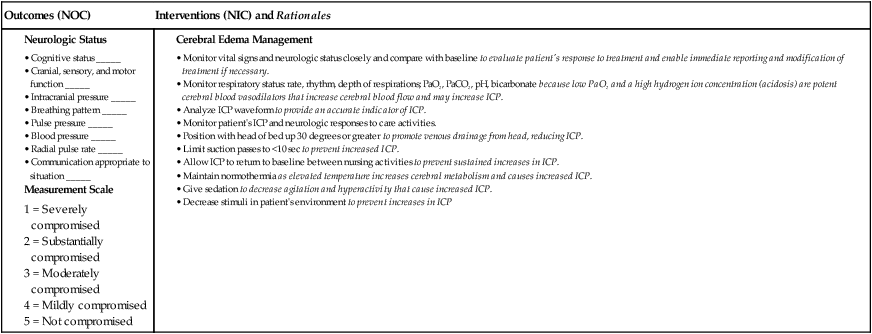
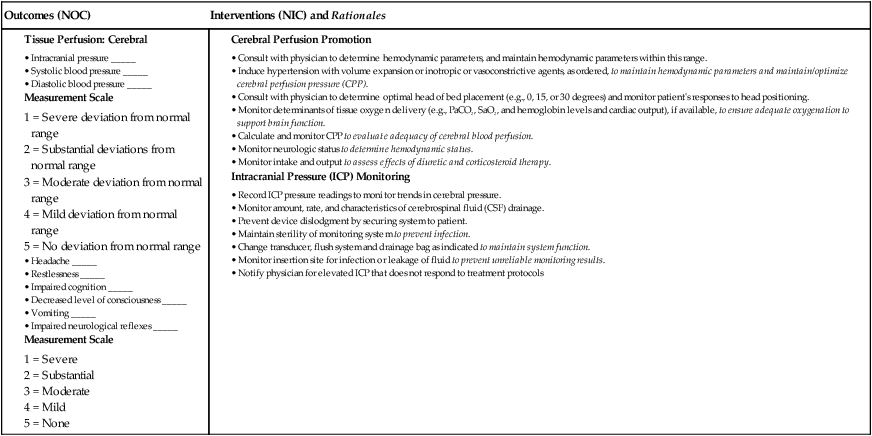
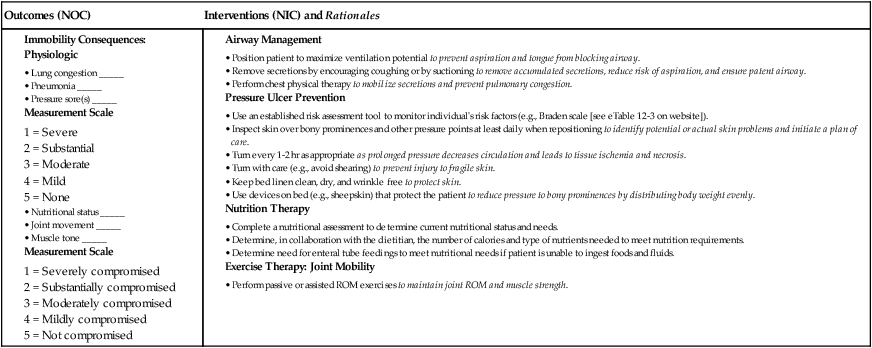
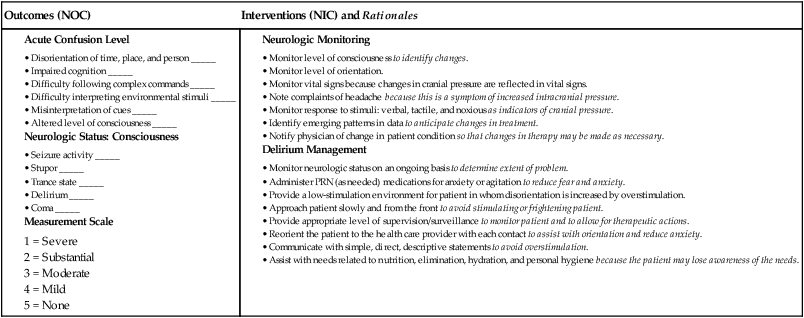
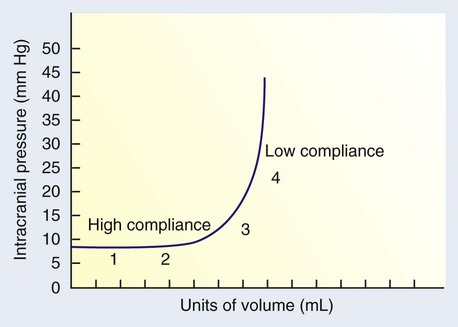
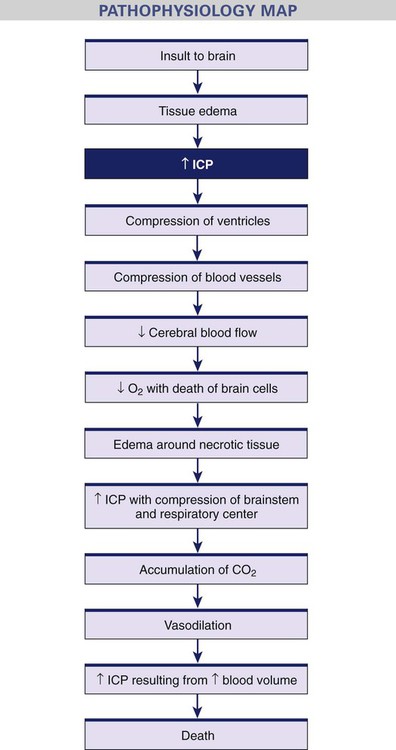
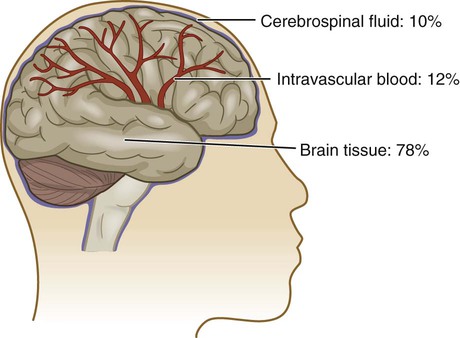
Chapter 57 1. Explain the physiologic mechanisms that maintain normal intracranial pressure. 2. Describe the common etiologies, clinical manifestations, and collaborative care of the patient with increased intracranial pressure. 3. Describe the collaborative and nursing management of the patient with increased intracranial pressure. 4. Differentiate types of head injury by mechanism of injury and clinical manifestations. 5. Describe the collaborative care and nursing management of the patient with a head injury. 6. Compare the types, clinical manifestations, and collaborative care of patients with brain tumors. 7. Discuss the nursing management of the patient with a brain tumor. 8. Describe the nursing management of the patient undergoing cranial surgery. 9. Differentiate among the primary causes, collaborative care, and nursing management of brain abscess, meningitis, and encephalitis. Understanding the dynamics associated with ICP is important in caring for patients with many different neurologic problems. The skull is like a closed box with three essential volume components: brain tissue, blood, and cerebrospinal fluid (CSF) (Fig. 57-1). The intracellular and extracellular fluids of brain tissue make up approximately 78% of this volume. Blood in the arterial, venous, and capillary network makes up 12% of the volume, and the remaining 10% is the volume of the CSF. The Monro-Kellie doctrine states that the three components must remain at a relatively constant volume within the closed skull structure. If the volume of any one of the three components increases within the cranial vault and the volume from another component is displaced, the total intracranial volume will not change.1 This hypothesis is only applicable in situations in which the skull is closed. The hypothesis is not valid in persons with displaced skull fractures or hemicraniectomy. ICP can be measured in the ventricles, subarachnoid space, subdural space, epidural space, or brain tissue using a pressure transducer.2 Normal ICP ranges from 5 to 15 mm Hg. A sustained pressure greater than 20 mm Hg is considered abnormal and must be treated. Cerebral blood flow (CBF) is the amount of blood in milliliters passing through 100 g of brain tissue in 1 minute. The global CBF is approximately 50 mL/min/100 g of brain tissue.3 The maintenance of blood flow to the brain is critical because the brain requires a constant supply of oxygen and glucose. The brain uses 20% of the body’s oxygen and 25% of its glucose.4 The lower limit of systemic arterial pressure at which autoregulation is effective in a normotensive person is a mean arterial pressure (MAP) of 70 mm Hg. Below this, CBF decreases, and symptoms of cerebral ischemia, such as syncope and blurred vision, occur. The upper limit of systemic arterial pressure at which autoregulation is effective is a MAP of 150 mm Hg.3 When this pressure is exceeded, the vessels are maximally constricted, and further vasoconstrictor response is lost. The cerebral perfusion pressure (CPP) is the pressure needed to ensure blood flow to the brain. CPP is equal to the MAP minus the ICP (CPP = MAP − ICP) (see example in Table 57-1). This formula is clinically useful, although it does not consider the effect of cerebrovascular resistance. Cerebrovascular resistance, generated by the arterioles within the cranium, links CPP and blood flow as follows: CPP = Flow × Resistance. TABLE 57-1 CALCULATION OF CEREBRAL PERFUSION PRESSURE CPP = MAP − ICP Example: Systemic blood pressure = 122/84 mm Hg MAP = 97 mm Hg ICP = 12 mm Hg CPP = 85 mm Hg The relationship of pressure to volume is depicted in the pressure-volume curve (Fig. 57-2). The curve is affected by the brain’s compliance. Compliance is the expandability of the brain. It is represented as the volume increase for each unit increase in pressure. With low compliance, small changes in volume result in greater increases in pressure. Increased ICP is a potentially life-threatening situation that results from an increase in any or all of the three components (brain tissue, blood, CSF) within the skull. Elevated ICP is clinically significant because it diminishes CPP, increases risks of brain ischemia and infarction, and is associated with a poor prognosis.5 Common causes of increased ICP include a mass (e.g., hematoma, contusion, abscess, tumor) and cerebral edema (associated with brain tumors, hydrocephalus, head injury, or brain inflammation). These cerebral insults, which may result in hypercapnia, cerebral acidosis, impaired autoregulation, and systemic hypertension, increase the formation and spread of cerebral edema. This edema distorts brain tissue, further increasing the ICP, and leads to even more tissue hypoxia and acidosis. Fig. 57-3 illustrates the progression of increased ICP.
Nursing Management
Acute Intracranial Problems
Intracranial Pressure
Regulation and Maintenance of Intracranial Pressure
Normal Intracranial Pressure.
Cerebral Blood Flow
Autoregulation of Cerebral Blood Flow.
Pressure Changes.

Increased Intracranial Pressure
Mechanisms of Increased Intracranial Pressure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Management: Acute Intracranial Problems
Get Clinical Tree app for offline access