Nursing Care During Labor
Objectives
2. Describe three variations in cultural practices.
3. Compare alternative birth settings.
4. Outline three nursing assessments and interventions during each stage of labor.
5. Discuss the significance of psychological support during labor.
6. Review ways to protect the woman from infection.
7. Compare external and internal fetal monitoring during labor.
8. Compare the advantages and disadvantages of electronic fetal monitoring during labor.
9. Describe the cleansing of the woman’s perineum in preparation for birth.
10. Compare reassuring and nonreassuring fetal heart rates.
11. Relate the nurse’s role in fetal monitoring.
12. Describe the purpose of amnioinfusion.
13. Discuss the role of a doula in the delivery room.
14. Explain the common nursing responsibilities during birth.
15. Identify nursing priorities when assisting in an emergency (precip) delivery.
16. List four items that are important to record about the infant’s birth.
17. Discuss the immediate care of the newborn.
18. Explain the reason the neonate requires administration of vitamin K at birth.
19. Describe the nursing assessments that are important in the woman’s recovery period after birth.
20. Illustrate two ways to encourage maternal-newborn bonding after birth.
Key Terms
accelerations (ăk-sĕl-ĕr-Ā-shŭnz, p. 123)
amnioinfusion (ăm-nē-ō-ĭn-FŪ-zhăn, p. 127)
Apgar score (p. 140)
decelerations (dē-sĕl-ĕr-Ā-shŭnz, p. 123)
doula (DOO-lă, p. 132)
Duncan mechanism (p. 136)
early decelerations (p. 125)
external fetal monitoring (p. 121)
ferning (p. 127)
fetal pulse oximetry (ŏk-SĬM-ĕ-trē, p. 125)
internal fetal monitoring (p. 122)
late decelerations (p. 125)
Leopold’s maneuvers (p. 127)
Nitrazine paper test (NĪ-tră-zēn, p. 127)
nonreassuring heart rate pattern (p. 120)
precipitate delivery (p. 143)
reassuring heart rate pattern (p. 120)
Schultze mechanism (p. 136)
variable decelerations (p. 125)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
The labor and birth process is an exciting, anxiety-provoking, but rewarding time for the woman and her family. They are about to undergo one of the most meaningful and stressful events in life. The adequacy of their preparation for childbirth will now be tested. Labor begins with regular uterine contractions, continues with hours of hard work, and ends as the woman and her family begin the attachment process with their newborn.
The primary goal of nursing care is to ensure the best possible outcome for the mother and the newborn. Nursing care focuses on establishing a meaningful, open relationship; determining the fetal status; encouraging the woman’s self-direction and ability to cope; and supporting the woman and her family throughout the labor and birth process. Research-based goals for normal labor and delivery include allowing labor to start on its own, allowing freedom of movement during labor, providing continuous labor support without routine interventions, allowing spontaneous pushing in a non-supine position, and keeping mother and infant together in skin-to-skin contact immediately after birth (AWHONN, 2007).
Birth Settings
Birth settings can include traditional hospital birth settings, independent birthing centers, or home birth services. They often are designed, in principle, to emphasize the naturalness of childbirth. The nurse-midwife, in collaboration with the physician, assumes the overall management of the birth and prenatal and postpartum care. However, some alternative birth settings are managed by a nurse-midwife without a physician present. In these settings, the nurse assumes a variety of responsibilities, including childbirth education and assistance with the birth itself.
An important advantage of alternative birth settings to the woman and family is that they have more control over the events surrounding the birth experience. The woman has an opportunity to decide on her activities during labor. She is usually allowed to modify her eating and drinking patterns and can select different positions for comfort during labor and birth. In addition, her companions and family are given the opportunity to participate more in the birth process. Some common obstetric practices, such as artificial rupture of the membranes, intravenous administration of fluids, and administration of drugs, are minimized in alternative birth settings. If complications occur, the woman is transferred to a labor and delivery unit in a hospital.
In-Hospital Birthing Rooms
An in-hospital birthing room is a hospital room or suite furnished to provide a homelike atmosphere conducive to the parents’ participation in the birth (Figure 7-1). The woman stays in the same room for labor, delivery, and recovery; thus, the setting is called an LDR room. In some hospitals, the woman also remains in the same room during the postpartum stay, and that setting is known as an LDRP room. Siblings can visit and become acquainted with the newborn shortly after birth.
Freestanding Centers (Out-of-Hospital Birthing Centers)
Some families choose the out-of-hospital birthing center for maternity care. These centers combine a home environment with a short-stay, ambulatory health facility with access to in-hospital obstetric and newborn care. Their advantage over home birth is quick access to the hospital facility if needed. The program usually provides comprehensive prenatal, birth, and postpartum care.
Home Birth
A community-based nurse-midwife usually manages a home birth. The advantage of a home birth is that the woman is in familiar, comfortable surroundings during the labor and birth process with her family present. If hospitalization is not required, some couples decide on home birth because it is less expensive. However, the couple should know the risks involved in a home birth before making their decision. For example, there usually is a lack of emergency equipment and additional staff to handle emergencies, and their home may be too far from a hospital and medical care if any unforeseen complications arise.
Cultural Considerations
Knowledge about the beliefs, customs, and practices of different cultures should be incorporated in labor care (Table 7-1). Modesty is an important consideration for all women, but women in some cultures are particularly uncomfortable about exposure of their bodies. Exposure of as little of the woman’s body as possible is recommended.
Table 7-1
Birth Practices of Selected Cultural Groups
| Role of Woman in Labor and Delivery | Role of Father or Partner in Labor and Delivery |
| African American | |
| Participates actively Is vocal in labor Wants sponge bath postpartum only Avoids hair washing until lochia ceases | Female attendants are usually preferred. |
| American Indian | |
| Is stoic May have indigenous plants in room May wear special necklaces May use meditation chants Prefers water at room temperature to drink Prefers chicken soup and rice postpartum | Husband avoids eating meat during perinatal phase. Husband may provide support during labor. |
| Arabic | |
| Is passive but expressive Views keeping body covered as important May wear protective amulets May have low pain tolerance Values male newborn more than female Expects 20 days of bed rest after birth | Husband is not expected to participate but remains in control. Female family member is preferred as coach. Husband must be present if male health care provider examines woman. Husband may whisper praises in newborn’s ear. |
| Brazilian | |
| May not participate in coping techniques during delivery Needs to be offered pain relief options Stays at home for 40 days postpartum except for medical appointments | Presence of husband in delivery room is discouraged. |
| Cambodian (Khmer) | |
| Is stoic in labor If walking during labor, must not pause in doorway (thought to delay birth) Does not want the infant’s head touched without permission Colostrum discarded Will not nurse after delivery or eat vegetables in first week | Individual family preference decides whether father is present during delivery. |
| Central American (Guatemala, Nicaragua, El Salvador) | |
| Is vocal and active during labor May prefer to wear red (a protective color) If more affluent, prefers bottle feeding Prefers chicken soup, bananas, meat, and herbal tea Showers postpartum Avoids “cold foods” | Husband is expected to be present for support, but female family members participate more. |
| Chinese | |
| May be vocal during labor Must not pause in doorway if walking during labor (thought to delay birth) All doors and windows to be unlocked (thought to ease passage of infant) Do not use first name of woman May not shower for 30 days postpartum Covers ears to prevent air from entering body Prefers breastfeeding Needs to be encouraged to ask questions | Husband usually does not play an active role in labor and delivery, but oldest male makes decisions. Woman’s mother may participate. |
| Cuban | |
| Is vocal but passive during labor and delivery Uses formal name at introduction Must stay at home 41 days postpartum and be sheltered from stress | Mother of woman is preferred as coach. Husbands are not usually involved in labor but must be informed first of problems and progress. |
| Eritrean, Ethiopian | |
| Is stoic but takes active role Modesty very important; must remain covered Prefers breastfeeding for 2 years Remains in seclusion 40 days postpartum Consumes warm food and drinks during puerperium | Traditionally, husbands are not allowed to be present during labor and delivery. |
| Falkland Islands Native | |
| Places keys (unlock) and combs (untangle) under pillow of labor bed | |
| Filipino | |
| Prefers slippery foods (such as eggs) so infant will “slip through birth canal” Prefers midwife support Assumes active role in labor Prefers sponge baths postpartum | Husband is not usually with woman during labor. |
| Hindu, Sikh, Muslim, Nepalese, Fijian, Pakistani | |
| Assumes passive role and follows directions of trained professionals May keep head covered during labor Prenatal care started on 120th day of gestation Should not reveal sex of newborn until after placenta is delivered (to avoid upsetting the mother if the sex is not of her preference) Takes sponge baths postpartum Remains in seclusion 40 days postpartum | Female coach is preferred, although father waits near labor room for consultation. Husband must be present if male physician examines woman. Ceremony of A quqah involves father shaving head of newborn and whispering praises into ear of newborn. Coach may chant scriptures during birth. |
| Hmong (Laos, Myanmar [Burma], Thailand) | |
| Is usually quiet and passive Avoids multiple caregivers Avoids internal examinations Views full genital exposure as unacceptable Prefers squat position Do not remove amulets on wrists and ankles Do not use first name initially Prefers chicken, white rice, and warm fluids postpartum Bottle feeding popular | Husband is usually present and makes all decisions. |
| Israeli (Orthodox Jewish) | |
| Prefers nurse-midwife Maintains modesty Must not be intimate with husband until 7 days after lochia stops Males circumcised on the eighth day Females named on first Saturday after birth | Husband may not participate in prenatal classes. Husband may not touch wife during labor, view perineum, or view baby being born. Husband may participate from afar with verbal encouragement during labor. Woman’s mother participates in birth process. |
| Japanese | |
| Prefers north part of room May cut hair and take special vows Is assertive during labor but may not ask for pain relief Values modesty Will bathe and shower postpartum May expose infant to loud noises and music twice a day for a week to ward off evil spirits | Husband chants and throws rice to ward off evil spirits. Modern-day husbands are present and participate during labor and delivery. In modern Japan, husbands are compliant with health education. |
| Korean | |
| Is compliant with health care provider Avoids ice water Is an active participant in labor Do not address by first name initially Prefers sponge bath postpartum May not wish to ambulate early | Husband participates in labor and delivery. Husband prefers not to be told in advance of fetal prognosis. Family makes medical decisions. |
| Mexican American | |
| Believes supine position is best for fetus Selects her preferred coach Prefers privacy Accepts pain but is active in labor Will not shower postpartum and walks to bathroom only Avoids beans postpartum Uses alternative therapies for mother and newborn (see Chapter 21) | Husband is in control of decisions but is not present during labor. Female relatives provide support. Husband prefers not to be told in advance of serious fetal prognosis. |
| Puerto Rican | |
| Is active in labor Prefers hospital care Keeps body covered Does not eat beans, starch, or eggs if breastfeeding Will not wash hair for 40 days postpartum Prefers sponge bath and lotions | Husband assumes supportive role during labor and delivery. If not present during delivery, husband expects to be kept informed. |
| Vietnamese | |
| Woman expected to “suffer in silence” Needs to be offered options for pain relief Prefers upright position for labor and delivery Prefers warm fluids to drink Sponge bathes only for 2 weeks postpartum Newborn not praised to protect from jealousy | Female family member is preferred. Husband is expected to remain nearby. Sexual intercourse is prohibited during pregnancy and puerperium. |
| West Indian (Trinidad and Tobago, Jamaica, Barbados) | |
| Prefers midwife Maintains passive role and follows instructions Prefers bed rest for 1 week postpartum Do not address by first name initially | Female relative or friend as coach is preferred. Husband is not present in area. |
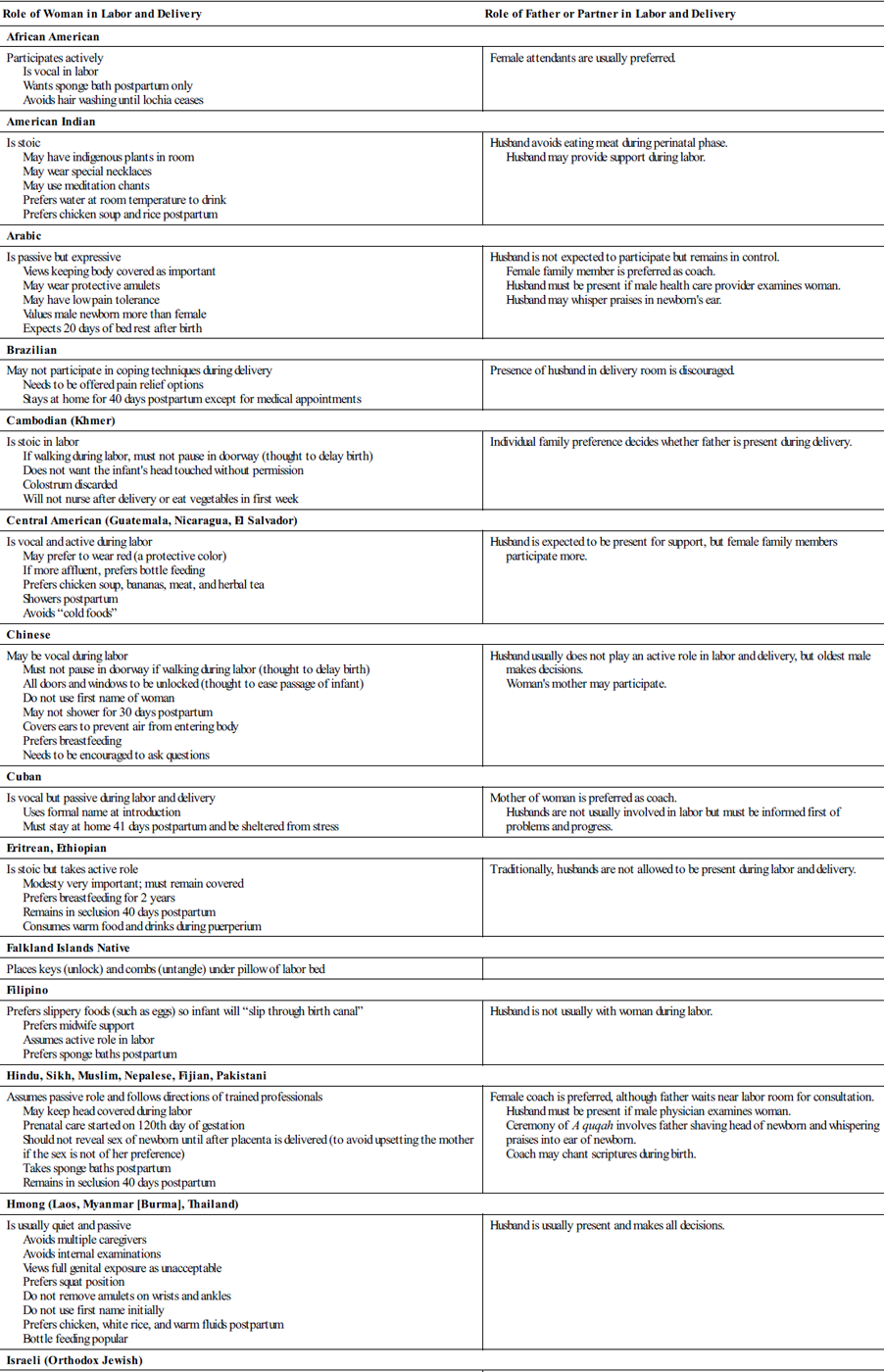
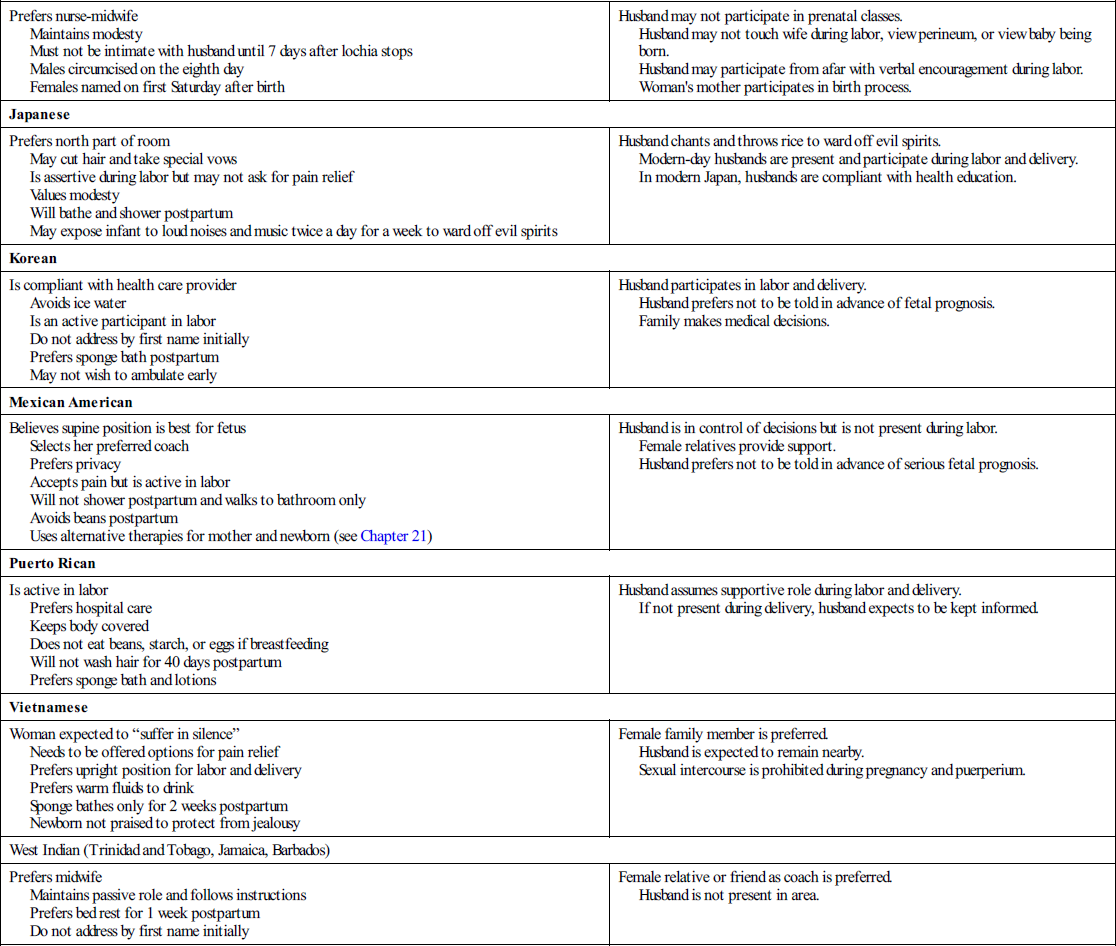
Data from Leifer, G. (2010). Introduction to maternity and pediatric nursing (6th ed.). Philadelphia: Saunders; Lowdermilk, D. I., Perry, S., & Hockenberry, D. (2010). Maternal child nursing care, St. Louis: Mosby; Wong, D.I., Perry, S.E., & Hockenberry-Eaton, M. (2009). Maternal and child nursing care. (2nd ed.). St. Louis: Mosby; Nichols, F. H., & Zwelling, E. (1997). Maternal-newborn nursing: Theory and practice. Philadelphia: Saunders; Minark, P. A., Lipson, J. G., & Dibble, S. I. (1996). Culture and nursing care. San Francisco: University of California; Lipson, J.F., & Steiger, N.J. (1996). Self-care nursing in a multicultural context. Thousand Oaks, CA: Sage publications; Murasaki, S. (1996). Diary of Lady Murasaki. New York: Penguin Books.
Pain expression varies with the cultural background. In some cultures, it is important for individuals to act in a manner that will not bring shame on the family; women, therefore, may not express pain outwardly. In other cultures, women may be vocally expressive during labor and cry out or moan with contractions and request pain relief.
Position preference varies with cultures, and there are differences within cultures. In many non-European societies uninfluenced by westernization, women assume an upright position in childbirth. In some cultures, kneeling or squatting during childbirth is common.
A female care provider is preferred in some cultures. Regardless of cultural background, the woman feels more comfortable and less stressed when her wishes are respected.
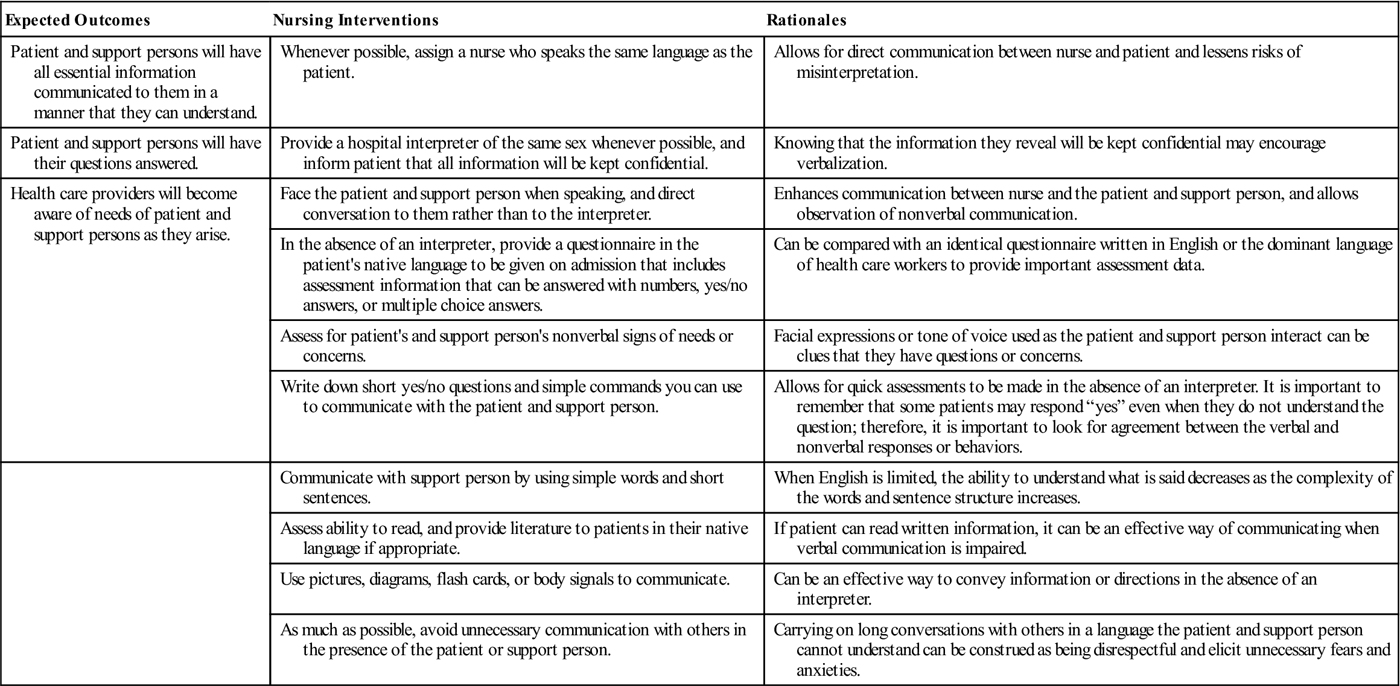
The support person with whom the woman feels comfortable varies according to her beliefs and customs. The woman’s mother or a female relative (rather than her husband or male partner) may give support during labor. Women from a strong matriarchal family structure may prefer their mothers or female extended family members to be with them during the labor process. Cultural sensitivity will assist nurses in being nonjudgmental, and they will be less likely to impose their own values and beliefs on women they care for (Nursing Care Plan 7-1).
Care Management
When to Go to the Hospital or Birth Center
During late pregnancy, the woman should be instructed about when to go to the hospital or birth center. This is not an exact time, but the general guidelines are:
The woman’s knowledge of her own body complements professional knowledge. Thus, when the woman feels “something is different,” she should be given positive encouragement for her self-monitoring of symptoms rather than her focusing on the exact symptoms of true or false labor (Palmer & Carty, 2006).
Data collection begins at the first contact with the woman, whether by telephone or in person. Women are encouraged to call the hospital labor and delivery unit or birthing center if they have questions about when to come to the hospital to be evaluated. The manner and expression or tone of voice in which the nurse communicates with the woman during their first contact can influence how the woman will feel about her birth experience.
Preadmission Forms
The nurse should review the available preadmission forms because they may have been completed a few weeks before admission. The prenatal record has information, including nursing and medical parameters, laboratory results, and nutritional guidance, that has been provided. Expressed psychosocial and cultural factors, including the woman’s birth plan and her special requests or needs, may also be documented.
Care Plan
A major challenge for the nurse is the formulation of a care plan for labor and birth. An individualized plan should include the woman’s coping mechanisms and support systems (see Chapter 5). The plan also includes whether the woman will labor, give birth, and recover in the same room or be transferred to a delivery room to give birth. Also, the care plan reflects the degree to which the partner will participate in the labor process.
The teaching aspect of the plan should incorporate what the woman can expect in labor care. The nursing care plan provides an important means of communication between the woman and the nurse (Nursing Care Plan 7-2).
Data Collection and Admission Procedures
The nurse is responsible for collecting data concerning the woman being admitted. Components of the admission information can be obtained from the prenatal record and then verified or updated. Women who have not had prenatal care will need to give more information to the nurse. The nurse’s data collection during admission focuses on three priorities: to determine (1) the condition of the mother and the fetus, (2) whether birth is imminent, and (3) whether the woman’s labor appears uneventful. Most facilities have a preprinted form to guide admission data collection. Women who have had prenatal care should have a prenatal record on file for the retrieval of information. Women who have not had prenatal care will have additional laboratory tests, which may include a complete blood count,
hematocrit, drug screen, tests for sexually transmitted infections, and others as indicated. Box 7-1 outlines nursing responsibilities during patient admissions.
Nursing Care of Patient in False Labor
True labor is characterized by changes in the cervix (effacement and dilation), which is the key distinction between true and false labors. See Table 6-1 for other characteristics of true and false labors.
A better term for false labor might be prodromal labor because these contractions help prepare the woman’s body and the fetus for true labor. Many women are observed for a short while (1 to 2 hours) if their initial assessment suggests that they are not in true labor and their membranes are intact. The mother and fetus are assessed during observation as if labor were occurring. Most facilities run an external electronic fetal monitor (EFM) strip for at least 20 minutes to document fetal well-being. The woman can usually walk about when not being monitored. If she is in true labor, walking often helps intensify the contractions and causes cervical effacement and dilation.
After the observation period, the woman’s labor status is reevaluated by the health care provider, and another vaginal examination is performed. If there is no change in the cervical effacement or dilation, the woman is usually sent home to await true labor. Sometimes, if it is her first child and she lives nearby, the woman in very early labor is sent home because the latent phase of most first labors is quite long.
Each woman in false labor (or early latent-phase labor) is evaluated individually. Factors to be considered include the number and duration of previous labors, distance from the facility, and availability of transportation.
The woman in false labor is often frustrated and needs generous reassurance that her symptoms will eventually change to true labor. No one stays pregnant forever, although it sometimes feels that way to a woman who has had several false alarms and is tired of being pregnant. Guidelines for coming to the facility should be reinforced before she leaves. If her membranes are ruptured, she is usually admitted even if labor has not begun because of the risk for infection or a prolapsed umbilical cord (see Chapter 14).
Focused Data Collection for First and Second Stages of Labor
In addition to creating an environment of trust and security, meeting informational needs, promoting relaxation, and providing a support system, the nurse must address specific physical concerns throughout the labor process. These nursing assessments and interventions begin during the first stage and continue through the labor process.
Priority activities are performed to assess the condition of the mother and fetus and to determine when the birth is imminent. Several assessments relate to the safety of both the mother and the fetus and therefore need to be carried out in a consistent time frame. In addition, any departure from the normal progress of labor should be promptly documented and reported.
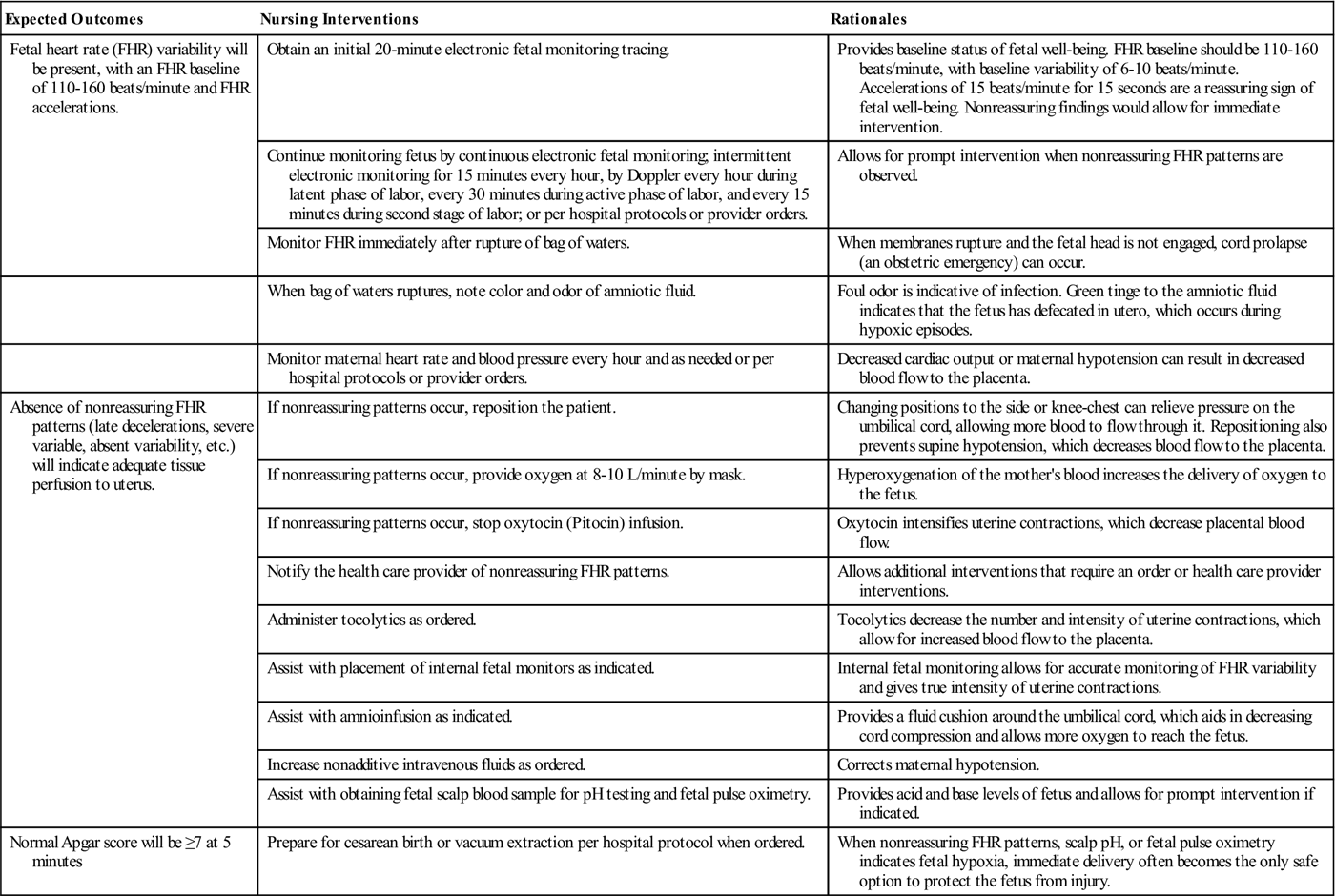
 Monitoring Fetal Heart Rate
Monitoring Fetal Heart Rate
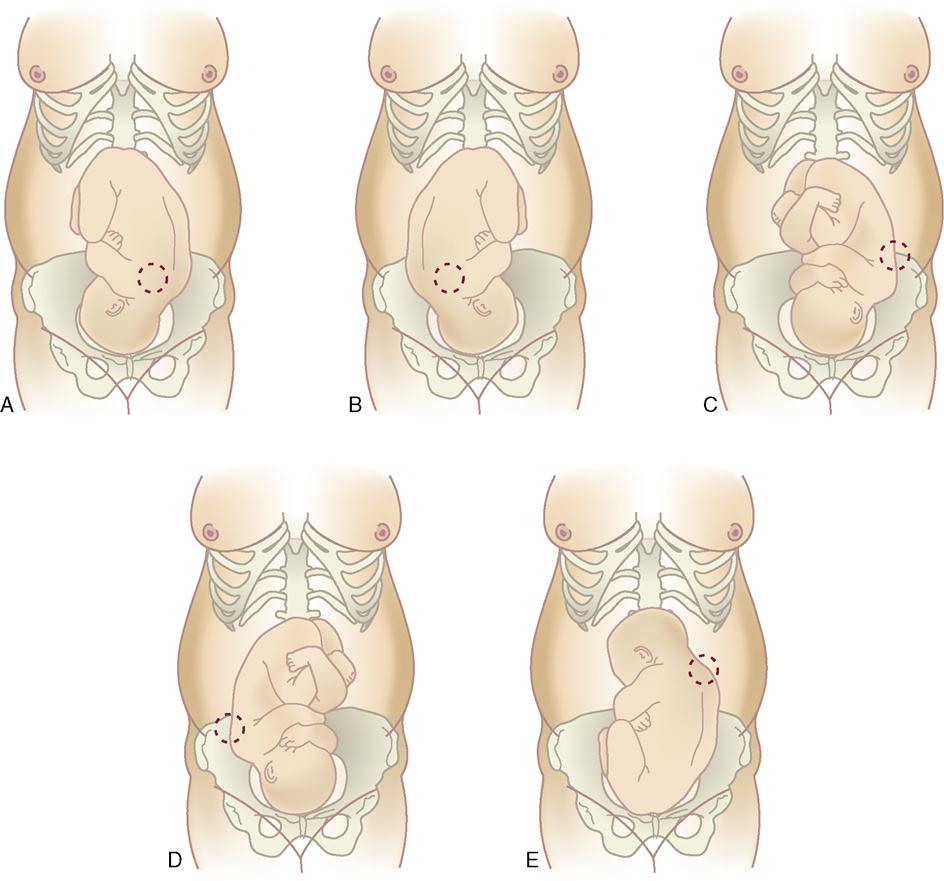
The fetal heart rate (FHR) should be assessed by auscultation with a Doppler transducer or fetoscope if the woman is not on an EFM. The location of the strongest fetal heart tone depends on the fetal position because the heart tone is best heard over the fetal back (Figure 7-2). If the woman and fetus are determined to be at low risk, the FHR is monitored and documented per routine (Skill 7-1). A sudden change in FHR or a measurement outside of the range of 110 to 160 beats/minute should be immediately reported. FHR should be taken immediately after the rupture of membranes because any prolapse of the umbilical cord is most likely to occur at this time. In addition, the FHR should be taken after a vaginal examination, administration of medications, and notation of abnormal fetal activity.
A Doppler transducer or a fetoscope is used to auscultate the FHR between, during, and immediately after uterine contractions. Advantages of continuously monitoring FHR with an EFM include the ability to evaluate FHR variability and to identify abnormalities in FHR patterns.
When a woman is on an EFM, the nurse should closely observe the FHR tracing. The nurse should report signs of fetal distress to the physician or nurse-midwife immediately. These signs include (1) a loss of baseline variability, (2) variable or late decelerations that persist after maternal position change, and (3) persistent fetal tachycardia. Meconium in the amniotic fluid when the fetus is in a vertex position, a sign of fetal distress, should also be reported.
Intermittent Fetal Heart Monitoring During Labor
Fetal monitoring during labor is an integral part of nursing care. Intrapartum fetal monitoring is surveillance used to identify the healthy fetus or the


 Ruptured membranes: The woman should go to the birth facility if her membranes rupture or if she thinks they may have ruptured.
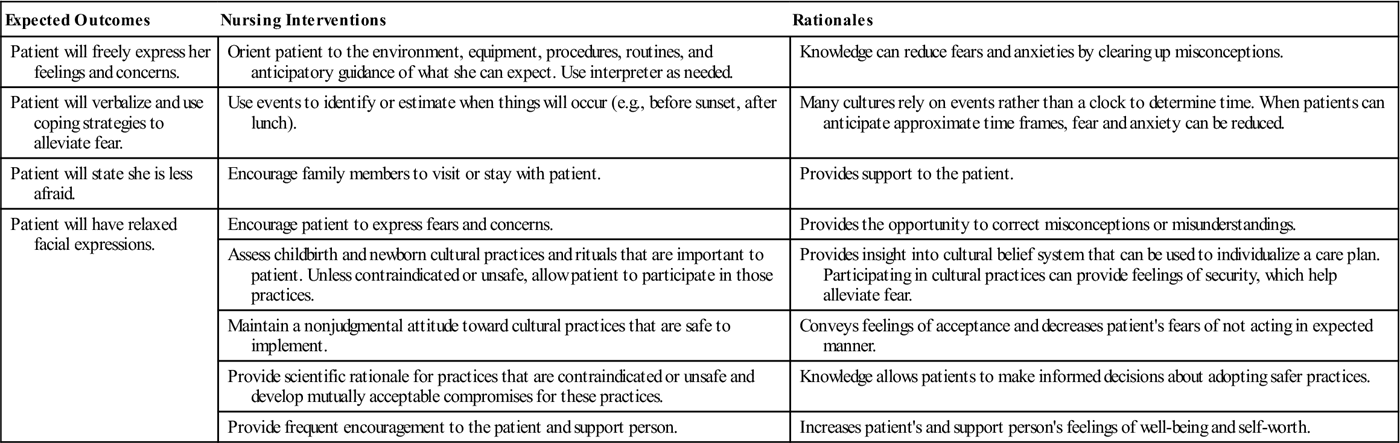
Ruptured membranes: The woman should go to the birth facility if her membranes rupture or if she thinks they may have ruptured. Nursing Care Plan 7-1
Nursing Care Plan 7-1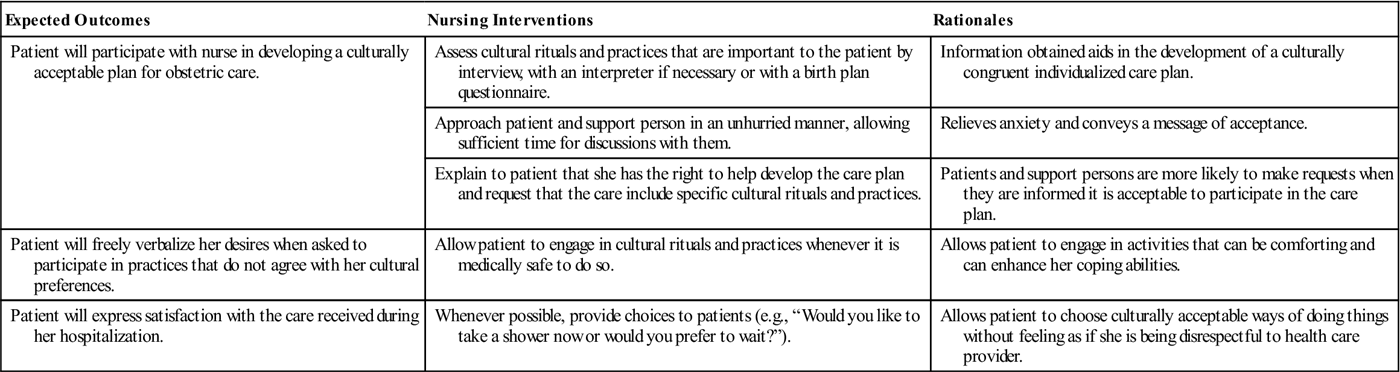
 Nursing Care Plan 7-2
Nursing Care Plan 7-2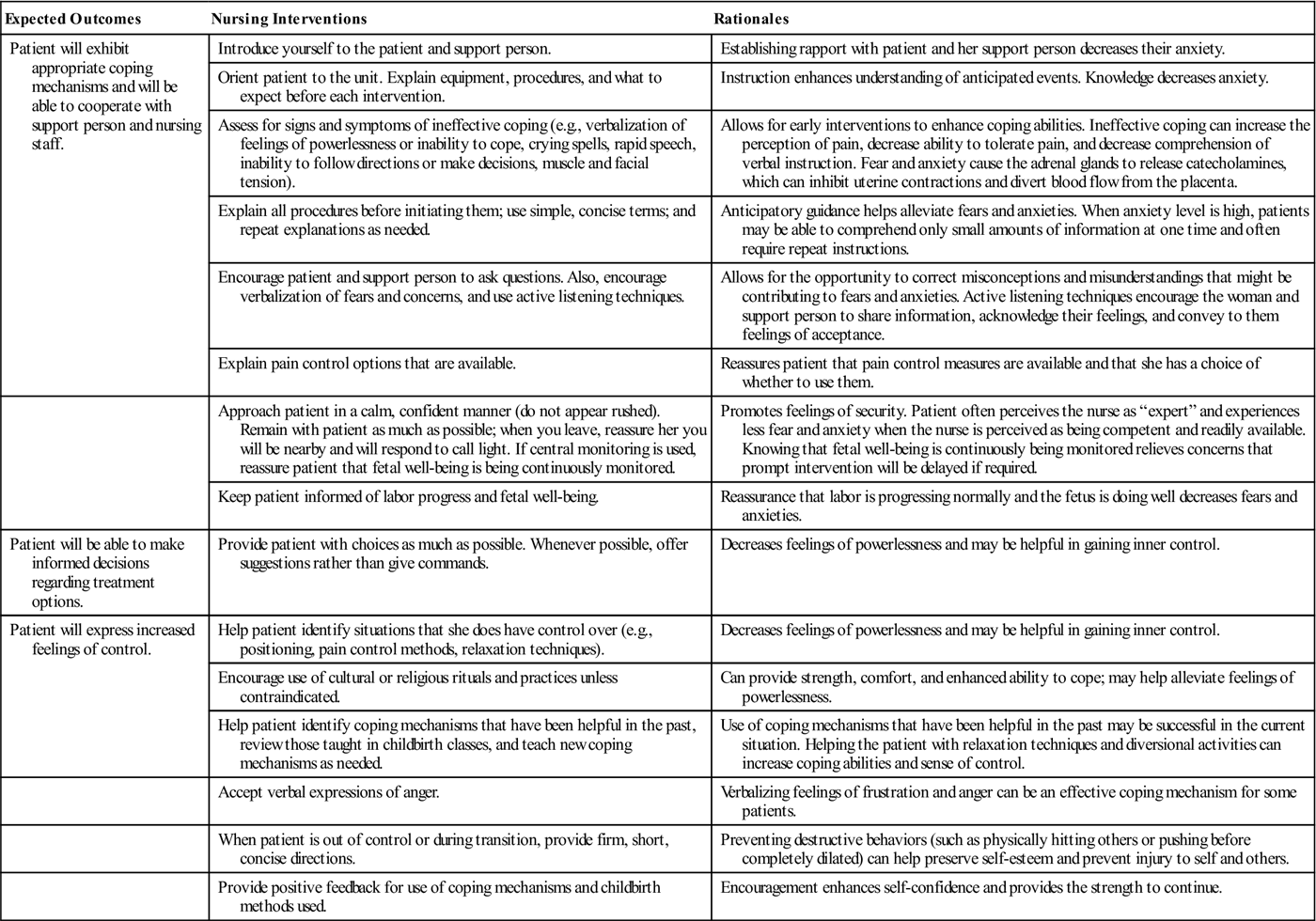


 Skill 7-1
Skill 7-1

