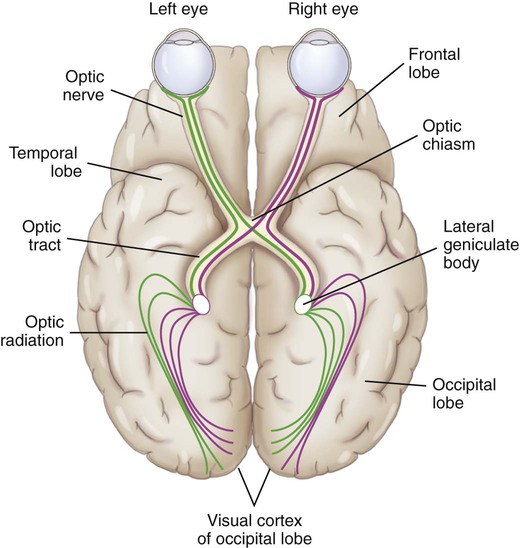
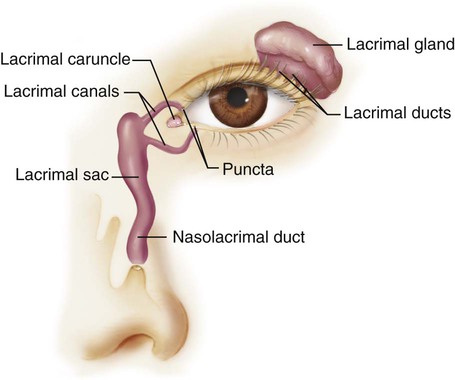
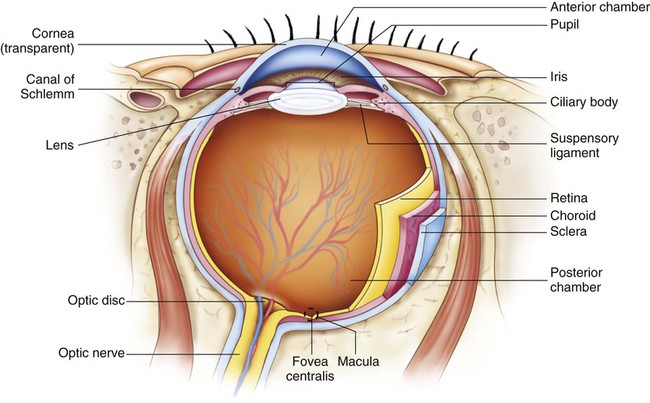
Chapter 21 1. Describe the structures and functions of the visual and auditory systems. 2. Explain the physiologic processes involved in normal vision and hearing. 3. Evaluate the significant subjective and objective assessment data related to the visual and auditory systems that should be obtained from a patient. 4. Select the appropriate techniques to use in the physical assessment of the visual and auditory systems. 5. Differentiate normal from common abnormal findings of a physical assessment of the visual and auditory systems. 6. Link the age-related changes in the visual and auditory systems to differences in assessment findings. 7. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the visual and auditory systems. eTABLE 21-1 DIAGNOSTIC TUNING FORK TESTS: AUDITORY SYSTEM The eyeball, or globe, is composed of three layers (Fig. 21-1). The tough outer layer is composed of the sclera and the transparent cornea. The middle layer consists of the uveal tract (iris, choroid, and ciliary body), and the innermost layer is the retina. The anterior cavity is divided into the anterior and posterior chambers. The anterior chamber lies between the iris and the posterior surface of the cornea, and the posterior chamber lies between the anterior surface of the lens and the posterior surface of the iris. The posterior cavity lies in the large space behind the lens and in front of the retina. Vitreous humor is a transparent gel-like substance that fills the posterior chamber (see Fig. 21-1). Light passing through the vitreous may be blocked by any nontransparent substance within the vitreous. The effect on vision varies, depending on the amount, type, and location of the substance blocking the light. Once the image travels through the refractive media, it is focused on the retina (Fig. 21-2). From the retina, the impulses travel through the optic nerve to the optic chiasm where the nasal fibers of each eye cross over to the other side. Fibers from the left field of both eyes form the left optic tract and travel to the left occipital cortex. The fibers from the right field of both eyes form the right optic tract and travel to the right occipital cortex. This arrangement of the nerve fibers in the visual pathways allows determination of the anatomic location of abnormalities. The eyebrows, eyelids, and eyelashes serve an important role in protecting the eye. They provide a physical barrier to dust and foreign particles (Fig. 21-3). The eye is further protected by the surrounding bony orbit and by fat pads located below and behind the globe, or eyeball. The transparent and avascular cornea allows light to enter the eye (see Fig. 21-1). The curved cornea refracts (bends) incoming light rays to help focus them on the retina. The cornea consists of five layers: the epithelium, Bowman’s layer, the stroma, Descemet’s membrane, and the endothelium. The lacrimal system consists of the lacrimal gland and ducts, lacrimal canals and puncta, lacrimal sac, and nasolacrimal duct (see Fig. 21-3). In addition to the lacrimal gland, other glands provide secretions to make up the mucous, aqueous, and lipid layers of the tear film. The tear film moistens the eye and provides oxygen to the cornea. The lens is a biconvex, avascular, transparent structure located behind the iris. The primary function of the lens is to bend light rays so that they fall onto the retina. Accommodation occurs when the eye focuses on a near object and is facilitated by contraction of the ciliary body, which changes the shape of the lens. The ciliary body consists of the ciliary muscles, which surround the lens and lie parallel to the sclera. The ciliary processes lie behind the peripheral part of the iris and secrete aqueous humor. The choroid is a highly vascular structure that nourishes the ciliary body, the iris, and the outer portion of the retina. It lies inside and parallel to the sclera (see Fig. 21-1). The retina is the innermost layer of the eye that extends and forms the optic nerve. Neurons make up the major portion of the retina. Therefore retinal cells are unable to regenerate if destroyed. The retina lines the inside of the eyeball, extending from the area of the optic nerve to the ciliary body (see Fig. 21-1). It is responsible for converting images into a form that the brain can understand and process as vision. The retina is composed of two types of photoreceptor cells: rods and cones. Rods are stimulated in dim or darkened environments, and cones are receptive to colors in bright environments. The center of the retina is the fovea centralis, a pinpoint depression composed only of densely packed cones.1 This area of the retina provides the sharpest visual acuity. Surrounding the fovea is the macula, an area less than 1 mm2, which has a high concentration of cones and is relatively free of blood vessels. Every structure of the visual system is subject to changes as the individual ages. Whereas many of these changes are relatively benign, others may result in severely compromised visual acuity in the older adult. The psychosocial impact of poor vision or blindness can be highly significant. Age-related changes in the visual system and differences in assessment findings are presented in Table 21-1. TABLE 21-1 GERONTOLOGIC ASSESSMENT DIFFERENCES Obtain information about the patient’s past health history, including both the ocular and nonocular history. Question the patient specifically about systemic diseases, such as diabetes, hypertension, cancer, rheumatoid arthritis, syphilis and other sexually transmitted infections (STIs), acquired immunodeficiency syndrome (AIDS), muscular dystrophy, myasthenia gravis, multiple sclerosis, inflammatory bowel disease, and hypothyroidism or hyperthyroidism; many of these diseases have ocular manifestations. It is particularly important to determine whether the patient has any history of cardiac or pulmonary disease because β-adrenergic blockers are often used to treat glaucoma. These medications can slow heart rate, decrease blood pressure, and exacerbate asthma or chronic obstructive pulmonary disease (COPD).2 Ocular problems do not always affect the patient’s visual acuity. For example, patients with blepharitis or diabetic retinopathy may not have noticeable visual deficits. The focus of the functional health pattern assessment depends on the presence or absence of vision loss and whether the loss is permanent or temporary. Table 21-2 lists suggested health history questions related to the functional health patterns. TABLE 21-2 • Describe the change in your vision. Describe how this affects your daily life. • Do you wear protective eyewear (sunglasses, safety goggles, hats)?* • Do you wear contact lenses? If so, how do you take care of them? • If you use eyedrops, how do you instill them? • Do you have any allergies that cause eye symptoms?* • Do you have a family history of cataracts, glaucoma, or macular degeneration?* • Does your eye problem affect your ability to read?* • Do you have any eye pain?* Do you have any eye itching, burning, or foreign body sensation?* Patient characteristics such as gender, ethnicity, and age are important in assessing ophthalmic conditions. Men are more likely than women to have color blindness. The leading cause of blindness among African Americans is glaucoma.3 Older individuals are also at greater risk for glaucoma. The patient’s visual health can affect activities at home or at work. It is important to know how the patient perceives the current health problem. As outlined in Table 21-2, guide the patient in describing the current problem. Assess the patient’s ability to accomplish necessary self-care, especially any eye care related to the patient’s ophthalmic problem.
Nursing Assessment
Visual and Auditory Systems
Visual System
Structures and Functions of Visual System
Study
Description
Weber Test
The examiner places an activated tuning fork on the midline of the skull or the forehead. Ask the patient to indicate where the sound is heard best. In normal auditory function, the patient perceives a midline tone and the sound is heard equally in both ears. If a patient has conductive hearing loss in one ear, the sound will be heard louder (lateralizes) in that ear. If sensorineural loss is present, the sound is louder (lateralizes) in the unaffected ear.
Normal results: no lateralization
Rinne Test
The examiner holds the base of a tuning fork against the mastoid bone (BC—bone conduction of sound) and notes the time. When the sound is no longer perceived behind the ear (BC), the time is noted once again and the still vibrating fork is moved 0.5 to 2 inches in front of the ear canal (AC—air conduction of sound). Have the patient report when the sound next to the ear canal (AC) is no longer heard and note the time. Normally, the sound is heard twice as long in front of the ear as it is on the bone. The Rinne test is positive when the patient reports that air conduction (AC) is heard longer than bone conduction (BC). This can indicate a sensorineural hearing loss. If the patient hears the tuning fork better by bone conduction, the Rinne test is negative, which suggests a conductive hearing loss.
Normal results: AC>BC
Structures and Functions of Vision
Eyeball.
Refractive Media.
Visual Pathways.
External Structures and Functions
Internal Structures and Functions
Gerontologic Considerations
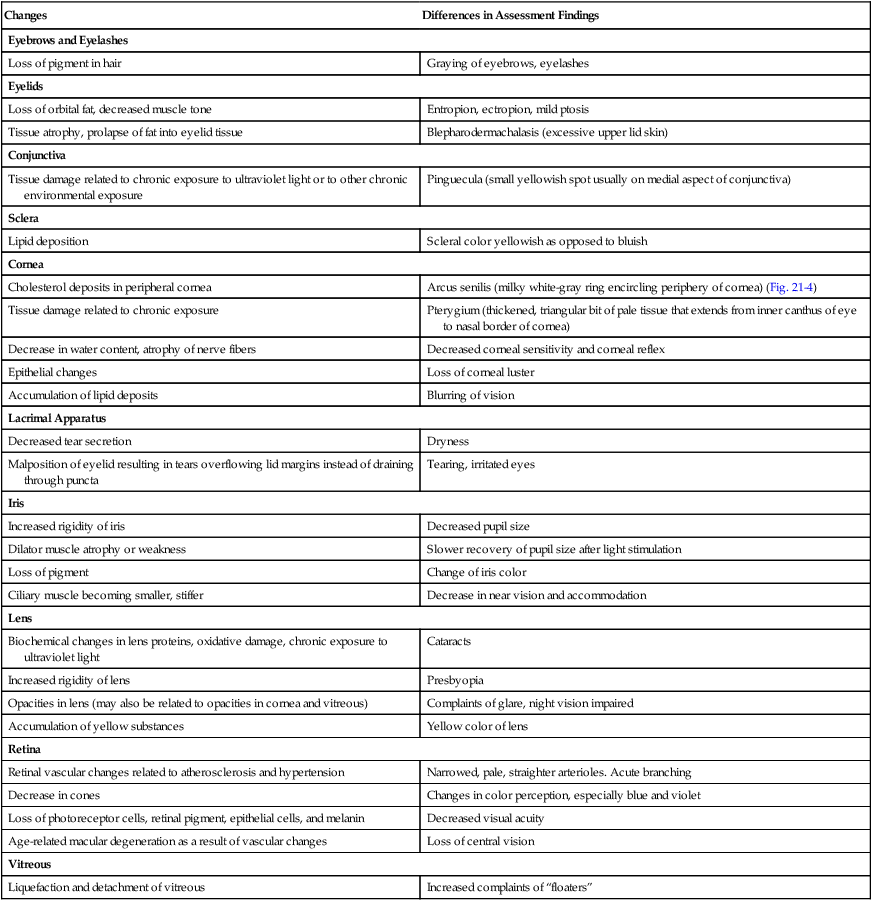
Effects of Aging on Visual System
Visual System
Changes
Differences in Assessment Findings
Eyebrows and Eyelashes
Loss of pigment in hair
Graying of eyebrows, eyelashes
Eyelids
Loss of orbital fat, decreased muscle tone
Entropion, ectropion, mild ptosis
Tissue atrophy, prolapse of fat into eyelid tissue
Blepharodermachalasis (excessive upper lid skin)
Conjunctiva
Tissue damage related to chronic exposure to ultraviolet light or to other chronic environmental exposure
Pinguecula (small yellowish spot usually on medial aspect of conjunctiva)
Sclera
Lipid deposition
Scleral color yellowish as opposed to bluish
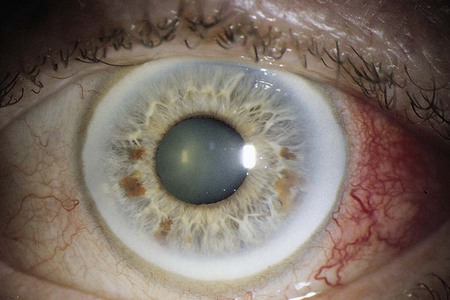
Cornea
Cholesterol deposits in peripheral cornea
Arcus senilis (milky white-gray ring encircling periphery of cornea) (Fig. 21-4)
Tissue damage related to chronic exposure
Pterygium (thickened, triangular bit of pale tissue that extends from inner canthus of eye to nasal border of cornea)
Decrease in water content, atrophy of nerve fibers
Decreased corneal sensitivity and corneal reflex
Epithelial changes
Loss of corneal luster
Accumulation of lipid deposits
Blurring of vision
Lacrimal Apparatus
Decreased tear secretion
Dryness
Malposition of eyelid resulting in tears overflowing lid margins instead of draining through puncta
Tearing, irritated eyes
Iris
Increased rigidity of iris
Decreased pupil size
Dilator muscle atrophy or weakness
Slower recovery of pupil size after light stimulation
Loss of pigment
Change of iris color
Ciliary muscle becoming smaller, stiffer
Decrease in near vision and accommodation
Lens
Biochemical changes in lens proteins, oxidative damage, chronic exposure to ultraviolet light
Cataracts
Increased rigidity of lens
Presbyopia
Opacities in lens (may also be related to opacities in cornea and vitreous)
Complaints of glare, night vision impaired
Accumulation of yellow substances
Yellow color of lens
Retina
Retinal vascular changes related to atherosclerosis and hypertension
Narrowed, pale, straighter arterioles. Acute branching
Decrease in cones
Changes in color perception, especially blue and violet
Loss of photoreceptor cells, retinal pigment, epithelial cells, and melanin
Decreased visual acuity
Age-related macular degeneration as a result of vascular changes
Loss of central vision
Vitreous
Liquefaction and detachment of vitreous
Increased complaints of “floaters”
Assessment of Visual System
Subjective Data
Important Health Information
Past Health History.
Functional Health Patterns.
Health Perception–Health Management
Nutritional-Metabolic
Elimination
Activity-Exercise
Sleep-Rest
Cognitive-Perceptual
Self-Perception–Self-Concept
Role-Relationship
Sexuality-Reproductive
Coping–Stress Tolerance
Value-Belief
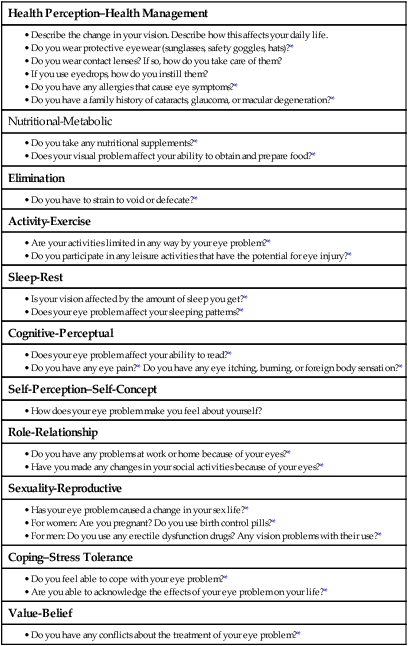
Health Perception–Health Management Pattern.