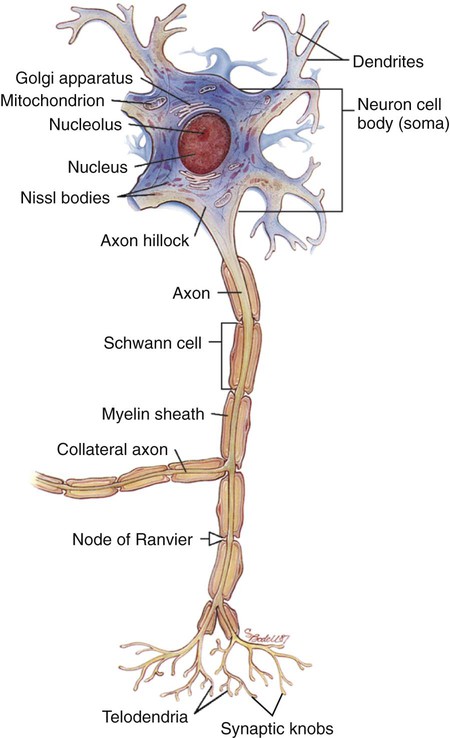
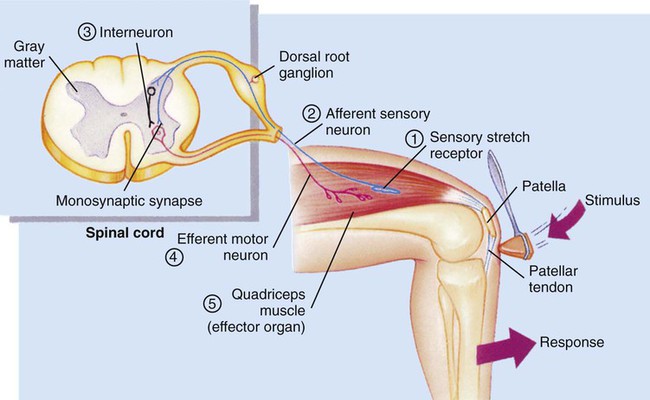
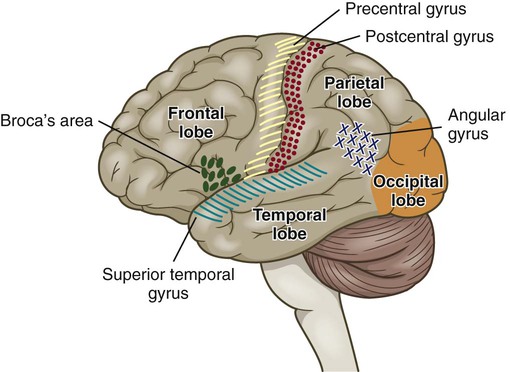
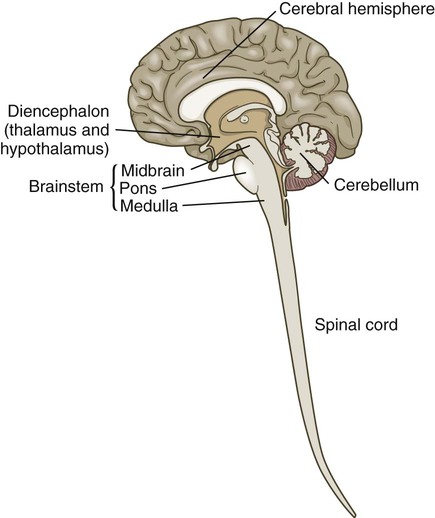
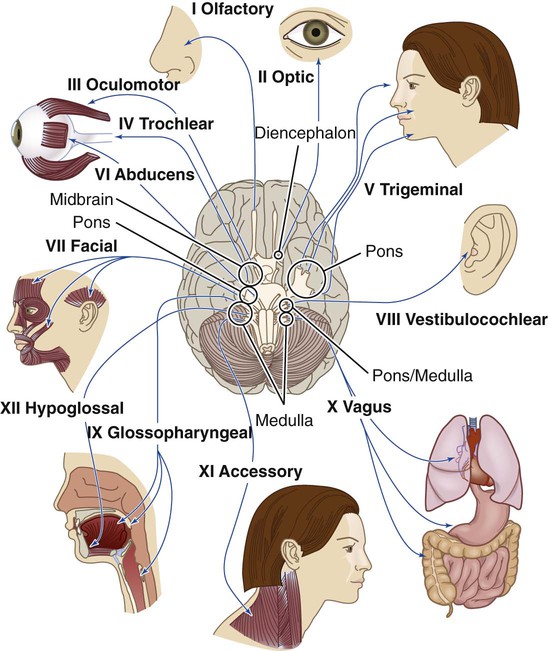
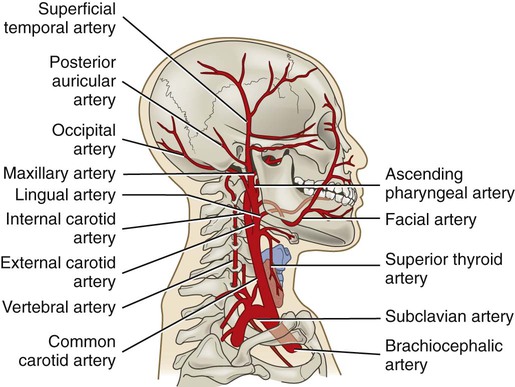
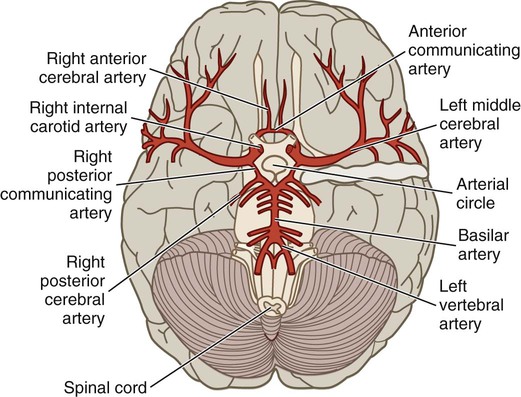
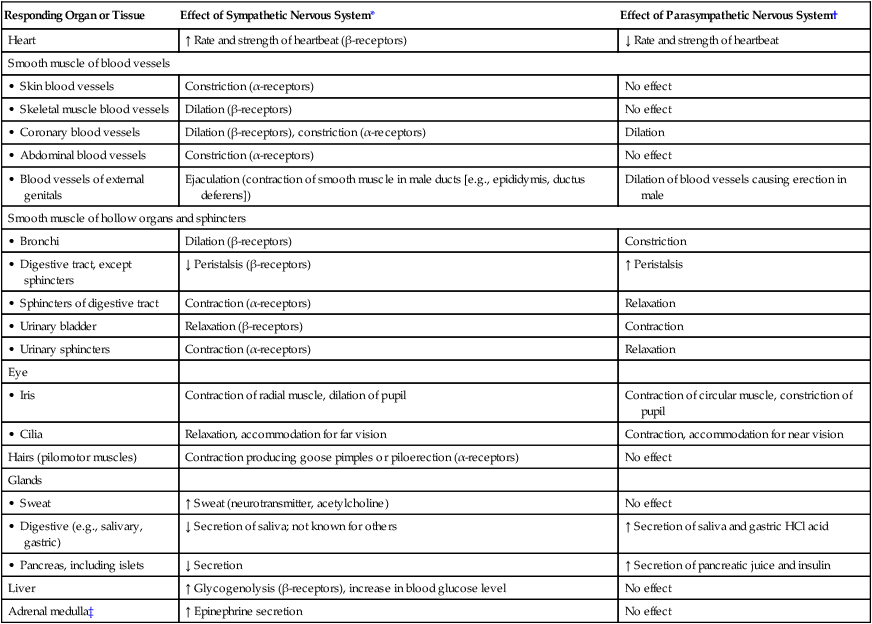
Chapter 56 1. Differentiate between the functions of neurons and glial cells. 2. Explain the anatomic location and functions of the cerebrum, brainstem, cerebellum, spinal cord, peripheral nerves, and cerebrospinal fluid. 3. Identify the major arteries supplying the brain. 4. Describe the functions of the 12 cranial nerves. 5. Compare the functions of the two divisions of the autonomic nervous system. 6. Link the age-related changes in the neurologic system to the differences in assessment findings. 7. Select significant subjective and objective data related to the nervous system that should be obtained from a patient. 8. Select appropriate techniques to use in the physical assessment of the nervous system. 9. Differentiate normal from abnormal findings of a physical assessment of the nervous system. 10. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the nervous system. eTABLE 56-1 EFFECT OF SYMPATHETIC AND PARASYMPATHETIC NERVOUS SYSTEMS *Neurotransmitter is norepinephrine unless otherwise stated. †Neurotransmitter is acetylcholine unless otherwise stated. ‡Sympathetic preganglionic axons terminate in contact with secreting cells of the adrenal medulla. Thus the adrenal medulla functions as a “giant sympathetic postganglionic neuron.” Modified from Thibodeau GA, Patton KT: Anatomy and physiology, ed 6, St Louis, 2006, Mosby. The nervous system is made up of two types of cells: neurons and glial cells. A typical neuron consists of a cell body, multiple dendrites, and an axon (Fig. 56-1). The cell body containing the nucleus and cytoplasm is the metabolic center of the neuron. Dendrites are short processes extending from the cell body that receive impulses from the axons of other neurons and conduct impulses toward the cell body. The axon projects varying distances from the cell body, ranging from several micrometers to more than a meter. The axon carries nerve impulses to other neurons or to end organs. The end organs are smooth and striated muscles and glands. Neurons have long been thought to be nonmitotic. That is, after being damaged neurons could not be replaced. The discovery of neuronal stem cells now demonstrates that neurogenesis occurs in adult brains after cerebral injury.1 Different types of macroglial cells include the astrocytes (most abundant), oligodendrocytes, and ependymal cells.2 Astrocytes are found primarily in gray matter and provide structural support to neurons. Their delicate processes form the blood-brain barrier with the endothelium of the blood vessels. They also play a role in synaptic transmission (conduction of impulses between neurons). When the brain is injured, astrocytes act as phagocytes for neuronal debris. They help restore the neurochemical milieu and provide support for repair. Proliferation of astrocytes contributes to the formation of scar tissue (gliosis) in the CNS. If the axon of the nerve cell is damaged, the cell attempts to repair itself. Damaged nerve cells attempt to grow back to their original destinations by sprouting many branches from the damaged ends of their axons. Axons in the CNS are generally less successful than peripheral axons in regeneration.3 Neurotransmitters are chemicals that affect the transmission of impulses across the synaptic cleft. (Examples of neurotransmitters are presented in Table 56-1.) Excitatory neurotransmitters activate postsynaptic receptors that increase the likelihood that an action potential will be generated. Inhibitory neurotransmitters activate postsynaptic receptors that inhibit the likelihood that an action potential will be generated. TABLE 56-1 CNS, Central nervous system; SNS, sympathetic nervous system. *These are examples only. Most of the neurotransmitters are also found in other locations and may have additional functions. Neurotransmitters can be affected by drugs and toxins, which can modify their function or block their attachment to receptor sites on the postsynaptic membrane. When many presynaptic cells release excitatory neurotransmitters on a single neuron, the sum of their input is enough to generate an action potential. Neurotransmitters continue to combine with the receptor sites at the postsynaptic membrane until they are inactivated by enzymes, are taken up by the presynaptic endings, or diffuse away from the synaptic region. With the use of cerebral microdialysis (minimally invasive sampling technique), neurotransmitter levels can now be measured in the cerebral cortex.4 A reflex is an involuntary response to stimuli. In the spinal cord, reflex arcs play an important role in maintaining muscle tone, which is essential for body posture. The components of a monosynaptic reflex arc (Fig. 56-2) are a receptor organ, an afferent neuron, an effector neuron, and an effector organ (e.g., skeletal muscle). The afferent neuron synapses with the efferent neuron in the gray matter of the spinal cord. More complex reflex arcs have other neurons (interneurons) in addition to the afferent neuron influencing the effector neuron. The cerebrum is composed of the right and left cerebral hemispheres and divided into four lobes: frontal, temporal, parietal, and occipital (Fig. 56-3). The functions of the cerebrum are multiple and complex (Table 56-2). The frontal lobe controls higher cognitive function, memory retention, voluntary eye movements, voluntary motor movement, and speech in Broca’s area. The temporal lobe integrates somatic, visual, and auditory data and contains Wernicke’s speech area. The parietal lobe interprets spatial information and contains the sensory cortex. Processing of sight takes place in the occipital lobe. TABLE 56-2 The thalamus (part of the diencephalon) lies directly above the brainstem (Fig. 56-4) and is the major relay center for afferent inputs to the cerebral cortex. The hypothalamus is located just inferior to the thalamus and slightly in front of the midbrain. It regulates the ANS and the endocrine system. The limbic system is located near the inner surfaces of the cerebral hemispheres and is concerned with emotion, aggression, feeding behavior, and sexual response. The brainstem includes the midbrain, pons, and medulla (see Fig. 56-4). Ascending and descending fibers to and from the cerebrum and cerebellum pass through the brainstem. The nuclei of cranial nerves III through XII are in the brainstem. The vital centers concerned with respiratory, vasomotor, and cardiac function are located in the medulla. The analysis of CSF composition provides useful diagnostic information related to certain nervous system diseases. CSF pressure is often measured in patients with actual or suspected intracranial injury. Increased intracranial pressure, indicated by increased CSF pressure, can force downward (central) herniation of the brain and brainstem. The signs marking this event are part of the herniation syndrome (see Chapter 57). The spinal cord can be seen as a series of spinal segments, one on top of another. In addition to the cell bodies, each segment contains a pair of dorsal (afferent) sensory nerve fibers or roots and ventral (efferent) motor fibers or roots, which innervate a specific region of the body. This combined motor-sensory nerve is called a spinal nerve (Fig. 56-5). The cell bodies of the voluntary motor system are located in the anterior horn of the spinal cord gray matter. The cell bodies of the autonomic (involuntary) motor system are located in the anterolateral portion of the spinal cord gray matter. The cell bodies of sensory fibers are located in the dorsal root ganglia just outside the spinal cord. On exiting the spinal column, each spinal nerve divides into ventral and dorsal rami, a collection of motor and sensory fibers that eventually goes to peripheral structures (e.g., skin, muscles, viscera). A dermatome is the area of skin innervated by the sensory fibers of a single dorsal root of a spinal nerve (Fig. 56-6). The dermatomes give a general picture of somatic sensory innervation by spinal segments. A myotome is a muscle group innervated by the primary motor neurons of a single ventral root. The dermatomes and myotomes of a given spinal segment overlap with those of adjacent segments because of the development of ascending and descending collateral branches of nerve fibers. Table 56-3 summarizes the motor and sensory components of the CNs. Fig. 56-7 shows the position of the CNs in relation to the brain and spinal cord. Just as the cell bodies of the spinal nerves are located in specific segments of the spinal cord, so are the cell bodies (nuclei) of the CNs located in specific segments of the brain. Exceptions are the nuclei of the olfactory and optic nerves. The primary cell bodies of the olfactory nerve are located in the nasal epithelium, and those of the optic nerve are in the retina. TABLE 56-3 Knowledge of the distribution of the brain’s major arteries is essential for understanding and evaluating the signs and symptoms of cerebrovascular disease and trauma. The brain’s blood supply arises from the internal carotid arteries (anterior circulation) and the vertebral arteries (posterior circulation), which are shown in Fig. 56-8. The internal carotid arteries provide blood flow to the anterior and middle portions of the cerebrum. The vertebral arteries join to form the basilar artery and provide blood flow to the brainstem, cerebellum, and posterior cerebrum. The circle of Willis is formed by communicating arteries that join the basilar and internal carotid arteries (Fig. 56-9). The circle of Willis is a safety valve for regulating cerebral blood flow when differential pressures or vascular occlusions are present.
Nursing Assessment
Nervous System
Responding Organ or Tissue
Effect of Sympathetic Nervous System*
Effect of Parasympathetic Nervous System†
Heart
↑ Rate and strength of heartbeat (β-receptors)
↓ Rate and strength of heartbeat
Smooth muscle of blood vessels
• Skin blood vessels
Constriction (α-receptors)
No effect
• Skeletal muscle blood vessels
Dilation (β-receptors)
No effect
• Coronary blood vessels
Dilation (β-receptors), constriction (α-receptors)
Dilation
• Abdominal blood vessels
Constriction (α-receptors)
No effect
• Blood vessels of external genitals
Ejaculation (contraction of smooth muscle in male ducts [e.g., epididymis, ductus deferens])
Dilation of blood vessels causing erection in male
Smooth muscle of hollow organs and sphincters
• Bronchi
Dilation (β-receptors)
Constriction
• Digestive tract, except sphincters
↓ Peristalsis (β-receptors)
↑ Peristalsis
• Sphincters of digestive tract
Contraction (α-receptors)
Relaxation
• Urinary bladder
Relaxation (β-receptors)
Contraction
• Urinary sphincters
Contraction (α-receptors)
Relaxation
Eye
• Iris
Contraction of radial muscle, dilation of pupil
Contraction of circular muscle, constriction of pupil
• Cilia
Relaxation, accommodation for far vision
Contraction, accommodation for near vision
Hairs (pilomotor muscles)
Contraction producing goose pimples or piloerection (α-receptors)
No effect
Glands
• Sweat
↑ Sweat (neurotransmitter, acetylcholine)
No effect
• Digestive (e.g., salivary, gastric)
↓ Secretion of saliva; not known for others
↑ Secretion of saliva and gastric HCl acid
• Pancreas, including islets
↓ Secretion
↑ Secretion of pancreatic juice and insulin
Liver
↑ Glycogenolysis (β-receptors), increase in blood glucose level
No effect
Adrenal medulla‡
↑ Epinephrine secretion
No effect
Structures and Functions of Nervous System
Cells of Nervous System
Neurons.
Glial Cells.
Nerve Regeneration
Nerve Impulse
Neurotransmitters.
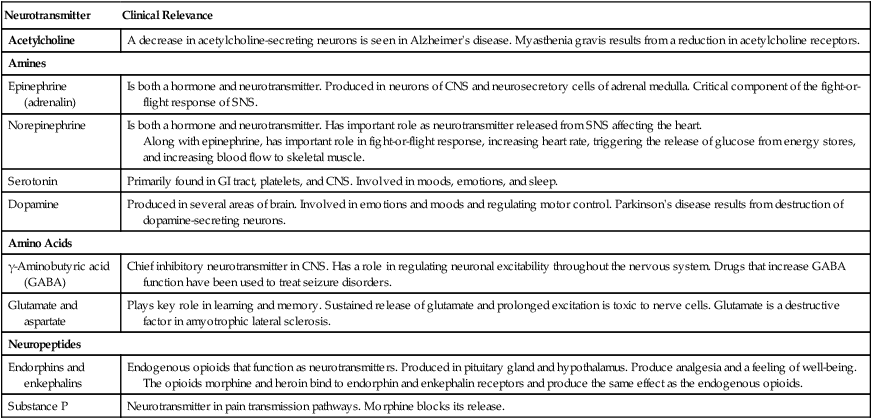
Neurotransmitter
Clinical Relevance
Acetylcholine
A decrease in acetylcholine-secreting neurons is seen in Alzheimer’s disease. Myasthenia gravis results from a reduction in acetylcholine receptors.
Amines
Epinephrine (adrenalin)
Is both a hormone and neurotransmitter. Produced in neurons of CNS and neurosecretory cells of adrenal medulla. Critical component of the fight-or-flight response of SNS.
Norepinephrine
Is both a hormone and neurotransmitter. Has important role as neurotransmitter released from SNS affecting the heart.
Along with epinephrine, has important role in fight-or-flight response, increasing heart rate, triggering the release of glucose from energy stores, and increasing blood flow to skeletal muscle.
Serotonin
Primarily found in GI tract, platelets, and CNS. Involved in moods, emotions, and sleep.
Dopamine
Produced in several areas of brain. Involved in emotions and moods and regulating motor control. Parkinson’s disease results from destruction of dopamine-secreting neurons.
Amino Acids
γ-Aminobutyric acid (GABA)
Chief inhibitory neurotransmitter in CNS. Has a role in regulating neuronal excitability throughout the nervous system. Drugs that increase GABA function have been used to treat seizure disorders.
Glutamate and aspartate
Plays key role in learning and memory. Sustained release of glutamate and prolonged excitation is toxic to nerve cells. Glutamate is a destructive factor in amyotrophic lateral sclerosis.
Neuropeptides
Endorphins and enkephalins
Endogenous opioids that function as neurotransmitters. Produced in pituitary gland and hypothalamus. Produce analgesia and a feeling of well-being.
The opioids morphine and heroin bind to endorphin and enkephalin receptors and produce the same effect as the endogenous opioids.
Substance P
Neurotransmitter in pain transmission pathways. Morphine blocks its release.
Central Nervous System
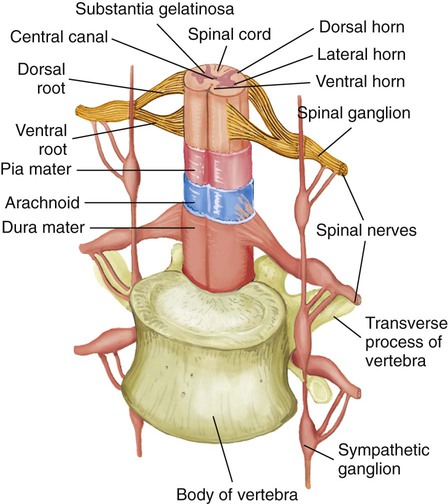
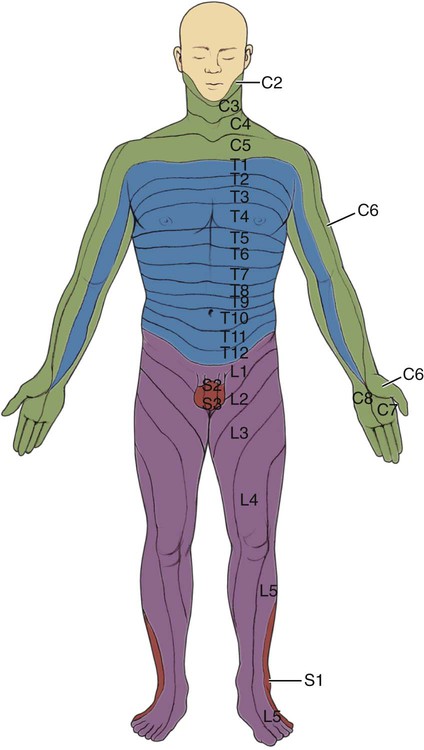
Spinal Cord.
Reflex Arc.
Brain.
Cerebrum.
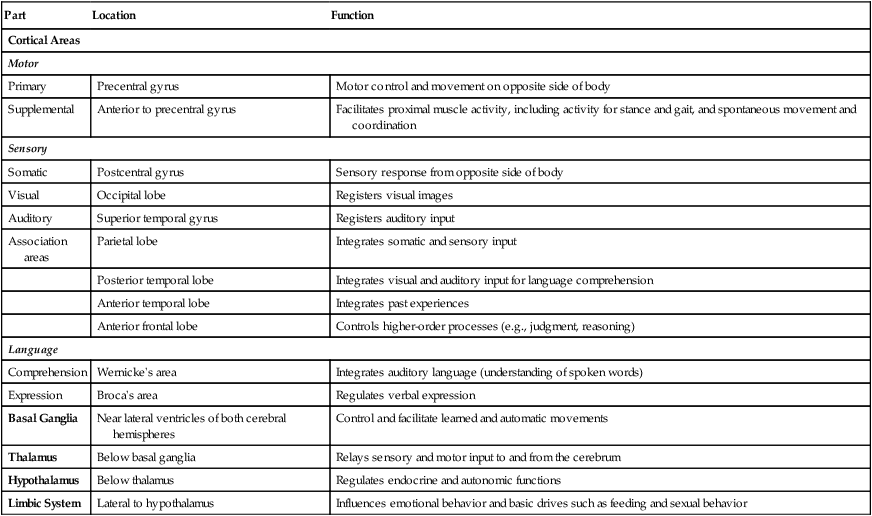
Part
Location
Function
Cortical Areas
Motor
Primary
Precentral gyrus
Motor control and movement on opposite side of body
Supplemental
Anterior to precentral gyrus
Facilitates proximal muscle activity, including activity for stance and gait, and spontaneous movement and coordination
Sensory
Somatic
Postcentral gyrus
Sensory response from opposite side of body
Visual
Occipital lobe
Registers visual images
Auditory
Superior temporal gyrus
Registers auditory input
Association areas
Parietal lobe
Integrates somatic and sensory input
Posterior temporal lobe
Integrates visual and auditory input for language comprehension
Anterior temporal lobe
Integrates past experiences
Anterior frontal lobe
Controls higher-order processes (e.g., judgment, reasoning)
Language
Comprehension
Wernicke’s area
Integrates auditory language (understanding of spoken words)
Expression
Broca’s area
Regulates verbal expression
Basal Ganglia
Near lateral ventricles of both cerebral hemispheres
Control and facilitate learned and automatic movements
Thalamus
Below basal ganglia
Relays sensory and motor input to and from the cerebrum
Hypothalamus
Below thalamus
Regulates endocrine and autonomic functions
Limbic System
Lateral to hypothalamus
Influences emotional behavior and basic drives such as feeding and sexual behavior
Brainstem.
Ventricles and Cerebrospinal Fluid.
Peripheral Nervous System
Spinal Nerves.
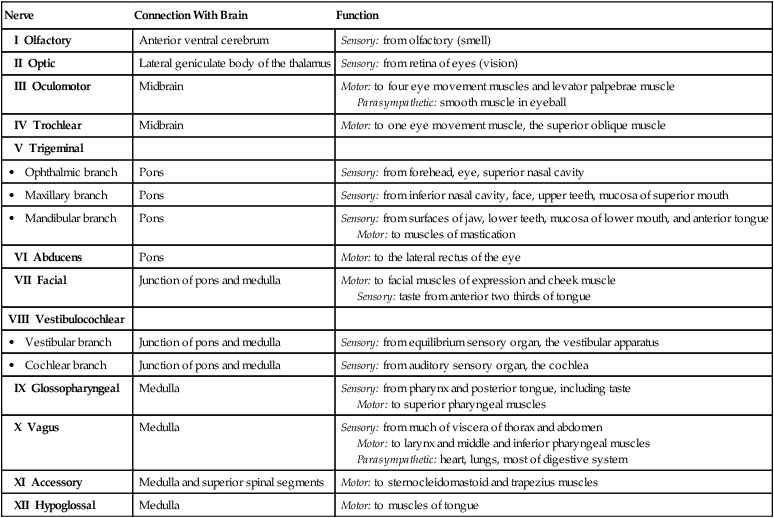
Cranial Nerves.
Nerve
Connection With Brain
Function
I Olfactory
Anterior ventral cerebrum
Sensory: from olfactory (smell)
II Optic
Lateral geniculate body of the thalamus
Sensory: from retina of eyes (vision)
III Oculomotor
Midbrain
Motor: to four eye movement muscles and levator palpebrae muscle
Parasympathetic: smooth muscle in eyeball
IV Trochlear
Midbrain
Motor: to one eye movement muscle, the superior oblique muscle
V Trigeminal
• Ophthalmic branch
Pons
Sensory: from forehead, eye, superior nasal cavity
• Maxillary branch
Pons
Sensory: from inferior nasal cavity, face, upper teeth, mucosa of superior mouth
• Mandibular branch
Pons
Sensory: from surfaces of jaw, lower teeth, mucosa of lower mouth, and anterior tongue
Motor: to muscles of mastication
VI Abducens
Pons
Motor: to the lateral rectus of the eye
VII Facial
Junction of pons and medulla
Motor: to facial muscles of expression and cheek muscle
Sensory: taste from anterior two thirds of tongue
VIII Vestibulocochlear
• Vestibular branch
Junction of pons and medulla
Sensory: from equilibrium sensory organ, the vestibular apparatus
• Cochlear branch
Junction of pons and medulla
Sensory: from auditory sensory organ, the cochlea
IX Glossopharyngeal
Medulla
Sensory: from pharynx and posterior tongue, including taste
Motor: to superior pharyngeal muscles
X Vagus
Medulla
Sensory: from much of viscera of thorax and abdomen
Motor: to larynx and middle and inferior pharyngeal muscles
Parasympathetic: heart, lungs, most of digestive system
XI Accessory
Medulla and superior spinal segments
Motor: to sternocleidomastoid and trapezius muscles
XII Hypoglossal
Medulla
Motor: to muscles of tongue
Cerebral Circulation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Assessment: Nervous System
Get Clinical Tree app for offline access