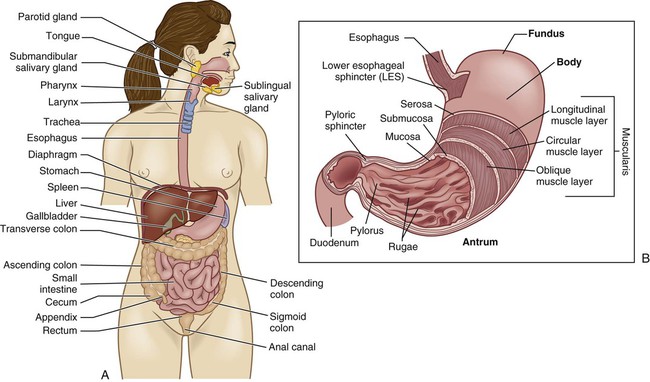
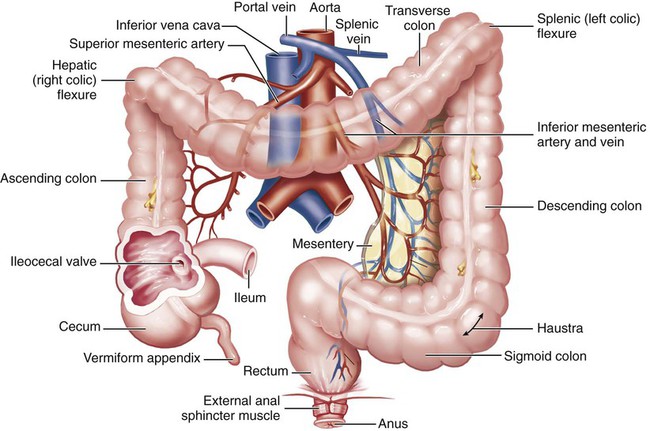
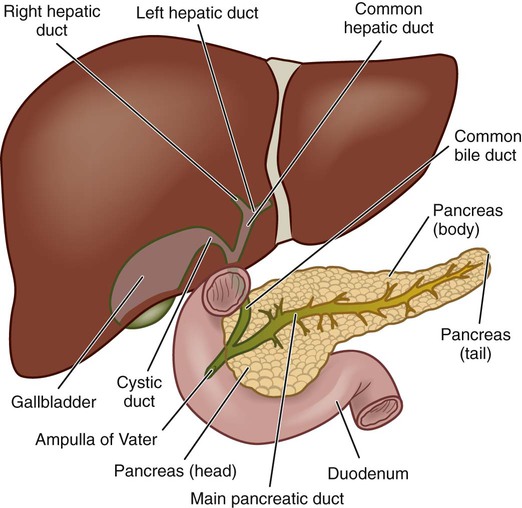
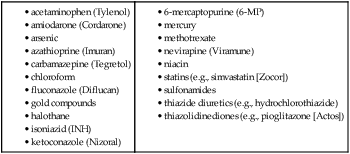
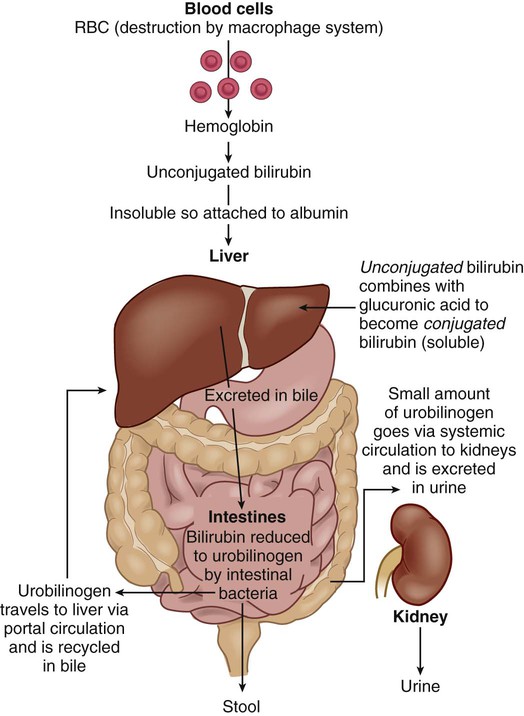
Chapter 39 1. Describe the structures and functions of the organs of the gastrointestinal tract. 2. Describe the structures and functions of the liver, gallbladder, biliary tract, and pancreas. 3. Differentiate the processes of ingestion, digestion, absorption, and elimination. 4. Explain the processes of biliary metabolism, bile production, and bile excretion. 5. Link the age-related changes of the gastrointestinal system to the differences in assessment findings. 6. Select significant subjective and objective assessment data related to the gastrointestinal system that should be obtained from a patient. 7. Identify the appropriate techniques used in the physical assessment of the gastrointestinal system. 8. Differentiate normal from abnormal findings of a physical assessment of the gastrointestinal system. 9. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the gastrointestinal system. The gastrointestinal (GI) system (also called the digestive system) consists of the GI tract and its associated organs and glands. Included in the GI tract are the mouth, esophagus, stomach, small intestine, large intestine, rectum, and anus. The associated organs are the liver, pancreas, and gallbladder (Fig. 39-1). The GI tract extends approximately 30 ft (9 m) from the mouth to the anus. It is composed of four common layers. From the inside to the outside, these layers are (1) mucosa, (2) submucosa, (3) muscle, and (4) serosa (see Fig. 39-1). The muscular coat consists of two layers: the circular (inner) layer and the longitudinal (outer) layer. Ingestion is the intake of food. A person’s appetite or desire to ingest food influences how much food is eaten. An appetite center is located in the hypothalamus. It is directly or indirectly stimulated by hypoglycemia, an empty stomach, decrease in body temperature, and input from higher brain centers. The hormone ghrelin released from the stomach mucosa plays a role in appetite stimulation. Another hormone, leptin, is involved in appetite suppression. (Ghrelin and leptin are discussed in Chapter 41.) The sight, smell, and taste of food frequently stimulate appetite. Appetite may be inhibited by stomach distention, illness (especially accompanied by fever), hyperglycemia, nausea and vomiting, and certain drugs (e.g., amphetamines). The stomach is usually J shaped and lies obliquely in the epigastric, umbilical, and left hypochondriac regions of the abdomen (see Fig. 39-5 later in the chapter). It always contains gastric fluid and mucus. The three main parts of the stomach are the fundus (cardia), body, and antrum (see Fig. 39-1). The pylorus is a small portion of the antrum proximal to the pyloric sphincter. Sphincter muscles (the LES and the pyloric sphincter) guard the entrance to and exit from the stomach. The digestive enzymes on the brush border of the microvilli chemically break down nutrients for absorption. The villi are surrounded by the crypts of Lieberkühn, which contain the multipotent stem cells for the other epithelial cell types. (Stem cells are discussed in Chapter 13.) Brunner’s glands in the submucosa of the duodenum secrete an alkaline fluid containing bicarbonate. Intestinal goblet cells secrete mucus that protects the mucosa. Digestion is the physical and chemical breakdown of food into absorbable substances. Digestion in the GI tract is facilitated by the timely movement of food through the GI tract and the secretion of specific enzymes. These enzymes break down foodstuffs to particles of appropriate size for absorption (Table 39-1). TABLE 39-1 In the stomach the digestion of proteins begins with the release of pepsinogen from chief cells. The stomach’s acidic environment results in the conversion of pepsinogen to its active form, pepsin. Pepsin begins the breakdown of proteins. There is minimal digestion of starches and fats. The food is mixed with gastric secretions, which are under neural and hormonal control (Tables 39-2 and 39-3). The stomach also serves as a reservoir for food, which is slowly released into the small intestine. The length of time that food remains in the stomach depends on the composition of the food, but average meals remain from 3 to 4 hours. TABLE 39-2 TABLE 39-3 HORMONES CONTROLLING GI SECRETION AND MOTILITY In the small intestine, carbohydrates are broken down to monosaccharides, fats to glycerol and fatty acids, and proteins to amino acids. The physical presence and chemical nature of chyme (food mixed with gastric secretions) stimulate motility and secretion. Secretions involved in digestion include enzymes from the pancreas, bile from the liver (see Table 39-1), and enzymes from the small intestine. Enzymes on the brush border of the microvilli complete the digestion process. These enzymes break down disaccharides to monosaccharides and peptides to amino acids for absorption. Both secretion and motility are under neural and hormonal control. When food enters the stomach and small intestine, hormones are released into the bloodstream (see Table 39-3). These hormones play important roles in the control of HCl acid secretion, production and release of digestive enzymes, and motility. The liver is the largest internal organ in the body, weighing approximately 3 lb (1.36 kg). It lies in the right epigastric region (see Fig. 39-5 later in the chapter). Most of the liver is enclosed in peritoneum. It has a fibrous capsule that divides it into right and left lobes (Fig. 39-3). The liver is essential for life. It functions in the manufacture, storage, transformation, and excretion of a number of substances involved in metabolism. The liver’s functions are numerous and can be classified into four main areas (Table 39-4). TABLE 39-4 Bile is produced by the hepatic cells and secreted into the biliary canaliculi of the lobules. Bile then drains into the interlobular bile ducts, which unite into the two main left and right hepatic ducts. The hepatic ducts merge with the cystic duct from the gallbladder to form the common bile duct (see Fig. 39-3). Most of the bile is stored and concentrated in the gallbladder. It is then released into the cystic duct and moves down the common bile duct to enter the duodenum at the ampulla of Vater. In the intestines, bilirubin is reduced to stercobilinogen and urobilinogen by bacterial action. Stercobilinogen accounts for the brown color of stool. A small amount of conjugated bilirubin is reabsorbed into the blood. Some urobilinogen is reabsorbed into the blood, returned to the liver through the portal circulation (enterohepatic), and excreted in the bile. Bilirubin, a pigment derived from the breakdown of hemoglobin, is constantly produced (Fig. 39-4). Because it is insoluble in water, it is bound to albumin for transport to the liver. This form of bilirubin is referred to as unconjugated. In the liver bilirubin is conjugated with glucuronic acid. Conjugated bilirubin is soluble and is excreted in bile. Bile also consists of water, cholesterol, bile salts, electrolytes, and phospholipids. Bile salts are needed for fat emulsification and digestion. The pancreas is a long, slender gland lying behind the stomach and in front of the first and second lumbar vertebrae. It consists of a head, body, and tail. The anterior surface of the pancreas is covered by peritoneum. The pancreas contains lobes and lobules. The pancreatic duct extends along the gland and enters the duodenum through the common bile duct (see Fig. 39-3). The pancreas has both exocrine and endocrine functions. The exocrine function contributes to digestion through the production and release of enzymes (see Table 39-1). The endocrine function occurs in the islets of Langerhans, whose β cells secrete insulin and amylin; α cells secrete glucagon; δ cells secrete somatostatin; and F cells secrete pancreatic polypeptide. The process of aging changes the functional ability of the GI system (Table 39-5). Diet, alcohol intake, and obesity affect organs of the GI system, making it a challenge to separate the sole effects of aging from lifestyle. Xerostomia (decreased saliva production), or dry mouth, affects many older adults and may be associated with difficulty swallowing (dysphagia).1 Many factors can lead to a decrease in appetite and make eating less pleasurable. These include a decrease in taste buds and salivary gland secretion, diminished sense of smell, and caries and periodontal disease leading to loss of teeth. TABLE 39-5 GERONTOLOGIC ASSESSMENT DIFFERENCES Age-related changes in the esophagus include delayed emptying resulting from smooth muscle weakness and an incompetent LES.2 Although motility of the GI system decreases with age, secretion and absorption are affected to a lesser extent. The older patient often has a decrease in HCl acid secretion (hypochlorhydria) and a subsequent reduction in the amount of intrinsic factor secreted. Although constipation is a common complaint of older adults, age-related changes in colonic secretion or motility have not been consistently shown.3 Factors that may increase the risk for constipation include slower peristalsis, inactivity, decreased dietary fiber, decreased fluid intake, constipating medications, and laxative abuse; neurologic, cognitive, and metabolic disorders may also play a role.4,5 (Constipation is discussed in Chapter 43.) The size of the pancreas is unaffected by aging, but it does undergo structural changes such as fibrosis, fatty acid deposits, and atrophy. Both obstructive and nonobstructive gallbladder diseases increase with age.6 Older adults, especially those over 85, are at risk for decreased food intake.7 The economic inability to purchase food supplies affects nutritional intake, especially in the older adult. Economic constraints may also reduce the number of fresh fruits and vegetables consumed and thus the amount of fiber. Immobility limits the ability to obtain and prepare meals. In the United States, approximately one third of people over 60 are obese.7,8 Age-related changes in the GI system and differences in assessment findings are presented in Table 39-5. The health history should include an assessment of the patient’s past and current use of medications. The names of all drugs, their frequency of use, and their duration of use are important. This is a critical aspect of history taking because many medications may not only have an effect on the GI system but also may be affected by abnormalities of the GI system. The medication assessment should include information about over-the-counter (OTC) medications, prescription drugs, herbal products, vitamins, and nutritional supplements (see the Complementary & Alternative Therapies box in Chapter 3 on p. 39). Note the use of prescription or OTC appetite suppressants. Many chemicals and drugs are potentially hepatotoxic (Table 39-6) and result in significant patient harm unless monitored closely. For example, chronic high doses of acetaminophen and nonsteroidal antiinflammatory drugs (NSAIDs) may be hepatotoxic. NSAIDs (including aspirin) may also predispose a patient to upper GI bleeding, with an increasing risk as the person ages. Other medications such as antibiotics may change the normal bacterial composition in the GI tract, resulting in diarrhea. Antacids and laxatives may affect the absorption of certain medications. Ask the patient if laxatives or antacids are taken, including the kind and frequency. Obtain information about hospitalizations for any problems related to the GI system. Also obtain data related to any abdominal or rectal surgery, including the year, reason for surgery, postoperative course, and possible blood transfusions. Terms related to surgery of the GI system are presented in Table 39-7. TABLE 39-7 SURGERIES OF THE GASTROINTESTINAL SYSTEM
Nursing Assessment
Gastrointestinal System
Structures and Functions of Gastrointestinal System
Ingestion
Digestion and Absorption
Stomach.
Small Intestine.
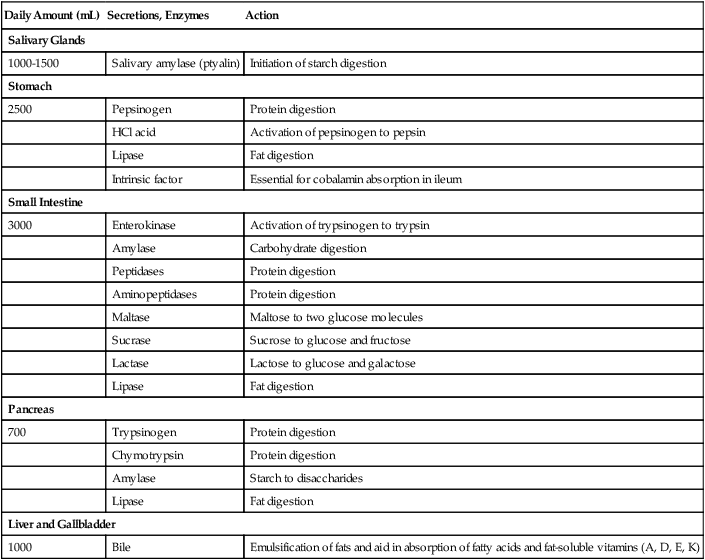
Physiology of Digestion.
Daily Amount (mL)
Secretions, Enzymes
Action
Salivary Glands
1000-1500
Salivary amylase (ptyalin)
Initiation of starch digestion
Stomach
2500
Pepsinogen
Protein digestion
HCl acid
Activation of pepsinogen to pepsin
Lipase
Fat digestion
Intrinsic factor
Essential for cobalamin absorption in ileum
Small Intestine
3000
Enterokinase
Activation of trypsinogen to trypsin
Amylase
Carbohydrate digestion
Peptidases
Protein digestion
Aminopeptidases
Protein digestion
Maltase
Maltose to two glucose molecules
Sucrase
Sucrose to glucose and fructose
Lactase
Lactose to glucose and galactose
Lipase
Fat digestion
Pancreas
700
Trypsinogen
Protein digestion
Chymotrypsin
Protein digestion
Amylase
Starch to disaccharides
Lipase
Fat digestion
Liver and Gallbladder
1000
Bile
Emulsification of fats and aid in absorption of fatty acids and fat-soluble vitamins (A, D, E, K)
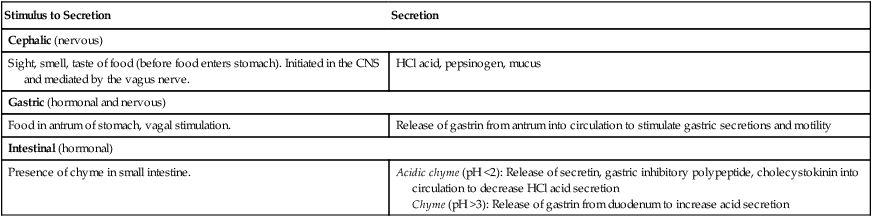
Stimulus to Secretion
Secretion
Cephalic (nervous)
Sight, smell, taste of food (before food enters stomach). Initiated in the CNS and mediated by the vagus nerve.
HCl acid, pepsinogen, mucus
Gastric (hormonal and nervous)
Food in antrum of stomach, vagal stimulation.
Release of gastrin from antrum into circulation to stimulate gastric secretions and motility
Intestinal (hormonal)
Presence of chyme in small intestine.
Acidic chyme (pH <2): Release of secretin, gastric inhibitory polypeptide, cholecystokinin into circulation to decrease HCl acid secretion
Chyme (pH >3): Release of gastrin from duodenum to increase acid secretion
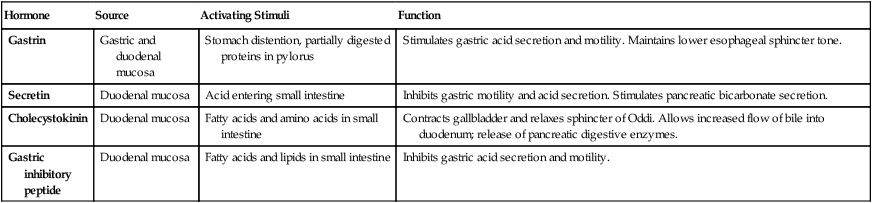
Hormone
Source
Activating Stimuli
Function
Gastrin
Gastric and duodenal mucosa
Stomach distention, partially digested proteins in pylorus
Stimulates gastric acid secretion and motility. Maintains lower esophageal sphincter tone.
Secretin
Duodenal mucosa
Acid entering small intestine
Inhibits gastric motility and acid secretion. Stimulates pancreatic bicarbonate secretion.
Cholecystokinin
Duodenal mucosa
Fatty acids and amino acids in small intestine
Contracts gallbladder and relaxes sphincter of Oddi. Allows increased flow of bile into duodenum; release of pancreatic digestive enzymes.
Gastric inhibitory peptide
Duodenal mucosa
Fatty acids and lipids in small intestine
Inhibits gastric acid secretion and motility.
Liver, Biliary Tract, and Pancreas
Liver.
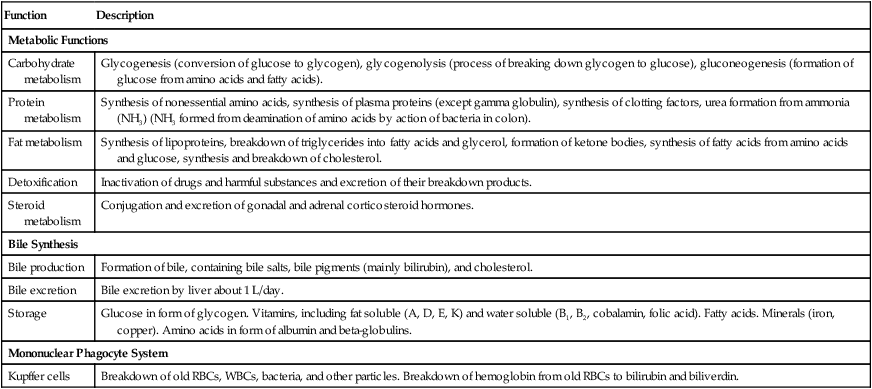
Function
Description
Metabolic Functions
Carbohydrate metabolism
Glycogenesis (conversion of glucose to glycogen), glycogenolysis (process of breaking down glycogen to glucose), gluconeogenesis (formation of glucose from amino acids and fatty acids).
Protein metabolism
Synthesis of nonessential amino acids, synthesis of plasma proteins (except gamma globulin), synthesis of clotting factors, urea formation from ammonia (NH3) (NH3 formed from deamination of amino acids by action of bacteria in colon).
Fat metabolism
Synthesis of lipoproteins, breakdown of triglycerides into fatty acids and glycerol, formation of ketone bodies, synthesis of fatty acids from amino acids and glucose, synthesis and breakdown of cholesterol.
Detoxification
Inactivation of drugs and harmful substances and excretion of their breakdown products.
Steroid metabolism
Conjugation and excretion of gonadal and adrenal corticosteroid hormones.
Bile Synthesis
Bile production
Formation of bile, containing bile salts, bile pigments (mainly bilirubin), and cholesterol.
Bile excretion
Bile excretion by liver about 1 L/day.
Storage
Glucose in form of glycogen. Vitamins, including fat soluble (A, D, E, K) and water soluble (B1, B2, cobalamin, folic acid). Fatty acids. Minerals (iron, copper). Amino acids in form of albumin and beta-globulins.
Mononuclear Phagocyte System
Kupffer cells
Breakdown of old RBCs, WBCs, bacteria, and other particles. Breakdown of hemoglobin from old RBCs to bilirubin and biliverdin.
Biliary Tract.
Bilirubin Metabolism.
Pancreas.
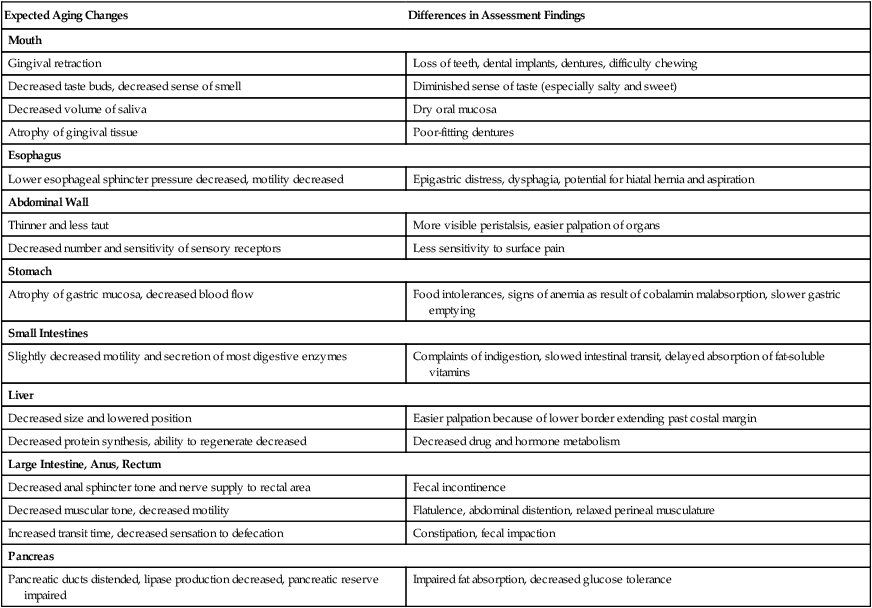
Gerontologic Considerations
Effects of Aging on Gastrointestinal System
Gastrointestinal System
Expected Aging Changes
Differences in Assessment Findings
Mouth
Gingival retraction
Loss of teeth, dental implants, dentures, difficulty chewing
Decreased taste buds, decreased sense of smell
Diminished sense of taste (especially salty and sweet)
Decreased volume of saliva
Dry oral mucosa
Atrophy of gingival tissue
Poor-fitting dentures
Esophagus
Lower esophageal sphincter pressure decreased, motility decreased
Epigastric distress, dysphagia, potential for hiatal hernia and aspiration
Abdominal Wall
Thinner and less taut
More visible peristalsis, easier palpation of organs
Decreased number and sensitivity of sensory receptors
Less sensitivity to surface pain
Stomach
Atrophy of gastric mucosa, decreased blood flow
Food intolerances, signs of anemia as result of cobalamin malabsorption, slower gastric emptying
Small Intestines
Slightly decreased motility and secretion of most digestive enzymes
Complaints of indigestion, slowed intestinal transit, delayed absorption of fat-soluble vitamins
Liver
Decreased size and lowered position
Easier palpation because of lower border extending past costal margin
Decreased protein synthesis, ability to regenerate decreased
Decreased drug and hormone metabolism
Large Intestine, Anus, Rectum
Decreased anal sphincter tone and nerve supply to rectal area
Fecal incontinence
Decreased muscular tone, decreased motility
Flatulence, abdominal distention, relaxed perineal musculature
Increased transit time, decreased sensation to defecation
Constipation, fecal impaction
Pancreas
Pancreatic ducts distended, lipase production decreased, pancreatic reserve impaired
Impaired fat absorption, decreased glucose tolerance
Assessment of Gastrointestinal System
Subjective Data
Important Health Information
Medications.
Surgery or Other Treatments.
Procedure
Description
Appendectomy
Removal of appendix
Cholecystectomy
Removal of gallbladder
Choledochojejunostomy
Opening between common bile duct and jejunum
Choledocholithotomy
Opening into common bile duct for removal of stones
Colectomy
Removal of colon
Colostomy
Opening into colon
Esophagoenterostomy
Removal of portion of esophagus with segment of colon attached to remaining portion
Esophagogastrostomy
Removal of esophagus and anastomosis of remaining portion to stomach
Gastrectomy
Removal of stomach
Gastrostomy
Opening into stomach
Glossectomy
Removal of tongue
Hemiglossectomy
Removal of half of tongue
Herniorrhaphy
Removal of a hernia
lleostomy
Opening into ileum
Mandibulectomy
Removal of mandible
Pyloroplasty
Enlargement and repair of pyloric sphincter area
Vagotomy
Resection of branch of vagus nerve ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree