Uniqueness Of NSTEMI
The diagnosis of NSTEMI is based on a history of acute cardiac ischaemia in the absence of ST segment elevation. In NSTEMI it is common for the ruptured atherosclerotic plaque to have caused incomplete coronary artery occlusion. Alternatively, the myocardium may have been protected by good collateral flow or may have a relatively low oxygen demand. This different underlying situation is the basis for the different effectiveness of and approaches to treatment from those used in STEMI (see Chapter 7).
The signs and symptoms of NSTEMI include:
- chest pain (Figure 6.2):
- characteristic, excruciating, “crushing”, “throbbing”, type of pain, retrosternal, radiates to the left shoulder, left ulnar part of arm, lower jaw, neck, abdomen to the umbilicus
- lasts for longer time than anginal pain – usually >30 minutes
- may have onset at rest – unlike stable angina
- not relieved by rest or nitro-glycerine
- 15–20% of infarcts are painless – especially in patients with diabetes and in the elderly – in these cases it may present as acute onset of breathlessness and signs of pulmonary oedema (see Chapter 7)
- characteristic, excruciating, “crushing”, “throbbing”, type of pain, retrosternal, radiates to the left shoulder, left ulnar part of arm, lower jaw, neck, abdomen to the umbilicus
- shortness of breath
- nausea
- vomiting
- diaphoresis (sweating)
- palpitations
- anxiety or sense of impending doom
- a feeling of being acutely ill
- non-specific ECG changes – ST segment depression/T wave inversion (see Figures 6.3 and 6.4)
- raised troponin levels (amount released reflects extent of myocardial damage).
Figure 6.2 Typical chest pain distribution in ACS – front and back.
From Jevon P, Humphreys M and Ewens B (2009) Nursing Medical Emergency Patients. Reproduced with permission from John Wiley & Sons.
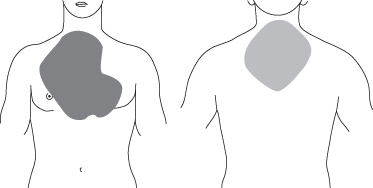
Figure 6.4 12-lead ECG demonstrating ST segment depression in leads I, II, III, aVF, V4–V6.
From Jevon P, Humphreys M and Ewens B (2009) Nursing Medical Emergency Patients. Reproduced with permission from John Wiley & Sons.
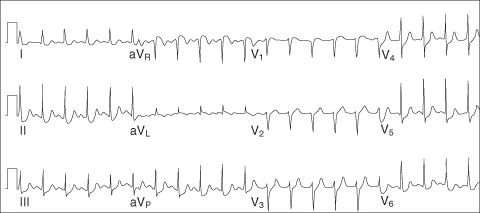
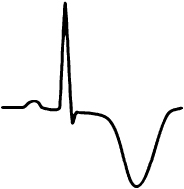
Myocardial ischaemia may give rise to T wave inversion, but it should be remembered that inverted T waves are normal in leads III, aVR and V1 in association with a predominantly negative QRS complex. T waves that are deep and symmetrically inverted (arrowhead) strongly suggest myocardial ischaemia.
The treatment of NSTEMI differs in some respect from the treatment of STEMI as the focus here is dictated largely by assessment of risk.
Diagnosis
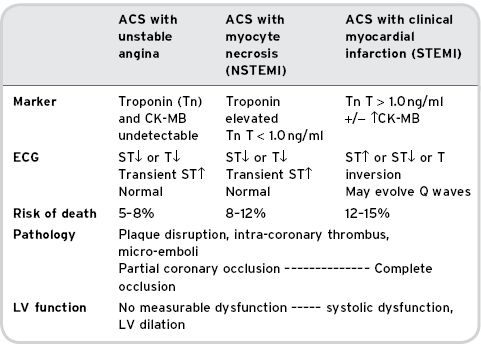
NSTEMI is only one of the many potential causes of chest pain; however, it is safer to treat the patient as if it is cardiac in origin until proven otherwise (Table 6.1 ).
Table 6.1 Spectrum of acute coronary syndrome
Adapted from the British Cardiac Society (2004).
Initial examination will include (see Chapters 3 and 4 for a fuller description) the following.
- Reported history of acute cardiac ischaemia:
- abrupt new onset of severe ischaemic chest pain, deterioration of previously stable angina or crescendo anginal symptoms in frequency and severity.
- 12-lead ECG.
- Blood tests (in particular serum cardiac markers such as troponin I/T and/or CK-MB, but also including urea and electrolytes, random glucose, random cholesterol and full blood count).
- Chest X-ray (portable – only if the cause is not thought to be cardiac; it is not appropriate to send the patient to the X-ray department in the acute situation).
These will be evaluated in conjunction with a rapid history and examination focusing primarily on the cardiovascular system (Connaughton, 2001) and a diagnosis made.
Cardiac Enzymes
NSTEMI belongs to the single clinical entity pathway that represents the entire clinical spectrum for ACS; the clinical approach focuses on risk stratification, in which cardiac markers have assumed a central role (American College of Cardiology [ACC; Braunwald et al., 2000], European Society of Cardiology [ESC; 2000] and British Cardiac Society [Fox et al., 2004]) (see Table 6.2).
Table 6.2 Table of cardiac markers in response to myocardial injury
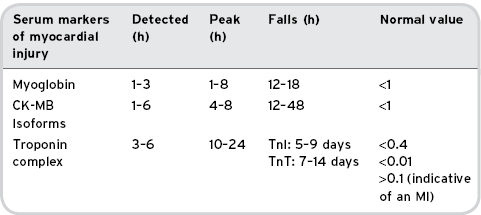
The best cardiac marker for each case depends on the time from onset of symptoms; the earliest markers are myoglobin and CK-MB isoforms (1–4 h). CK-MB and troponins are ideal in the intermediate period of 6–24 h. The troponins are recommended for elevation in patients who present more than 24 hours after symptom onset (discussed more fully in Chapter 4).
There are other non-cardiac conditions that troponins may be raised (i.e. renal failure, heart failure, etc.); therefore, the clinical context is very important.
Treatment Of NSTEMI
If the ECG does not show ST segment elevation, the term NSTEMI is applied. The accepted management of NSTEMI is empirical and initial treatment is guided by risk assessment (Gibler et al., 2005). Patients are stratified by haemodynamic, biochemical and medical factors, into high, intermediate and low risk groups (European Society of Cardiology, 2002), it is risk status which drives pharmacological treatments and the timing of further interventional procedures (Antman et al., 2000; see Box 6.1).
Box 6.1 TIMI (thrombolysis in myocardial infarction) risk score for unstable angina/non-ST-segment elevation myocardial infarction
If present, each of the following contributes +1 to the overall score.
- Score >4 indicates high-risk non-ST-segment elevation ACS.
- Age ≥65 years.
- At least three risk factors for coronary artery disease: male sex, hyperlipidaemia, hypertension, smoking, diabetes mellitus, family history of premature coronary disease.
- Previous coronary stenosis ≥50 per cent.
- ST-segment elevation or depression at presentation.
- Two or more anginal events in the past 24 hours.
- Aspirin use in the past 7 days.
- Elevated serum cardiac biomarkers.
(Antman et al., 2000)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree