Chapter 7 Multi-infarct Dementia (MID); Dementia of the Alzheimer Type (DAT) Lou Gehrig’s Disease; Motor Neuron Disease; Progressive Bulbar Palsy; Progressive Muscular Atrophy
Neurological Care Plans
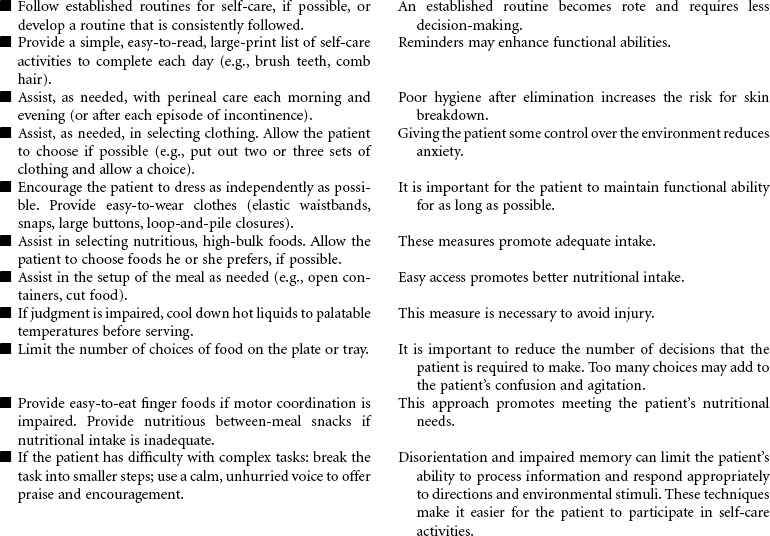
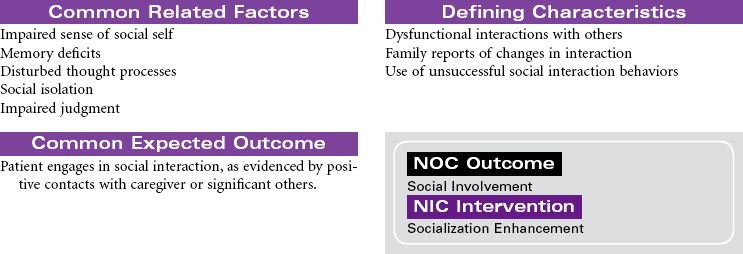
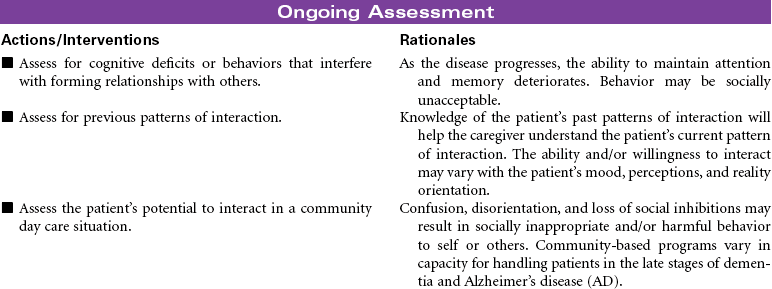
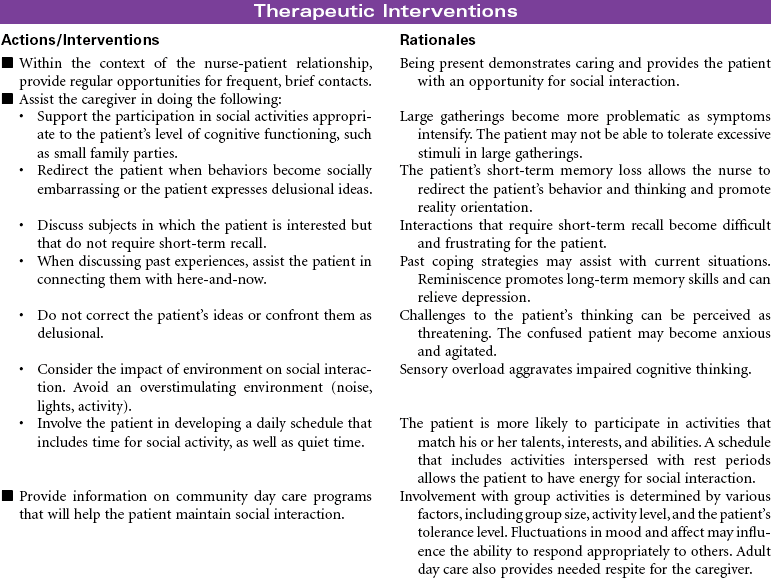
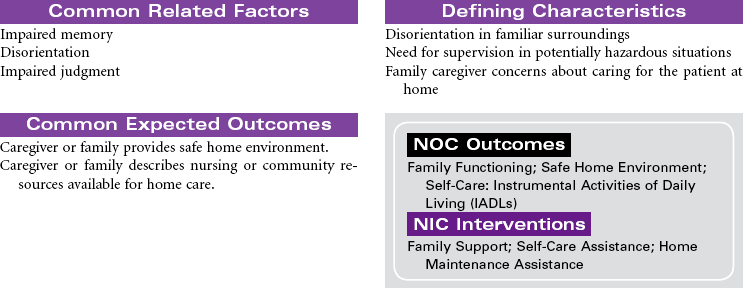
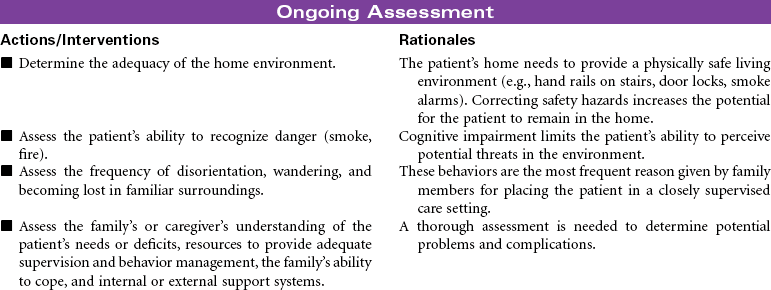
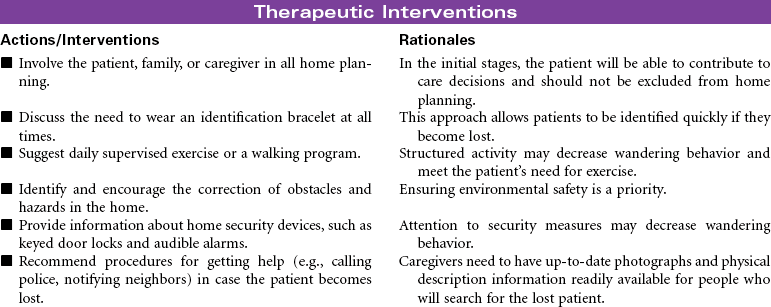
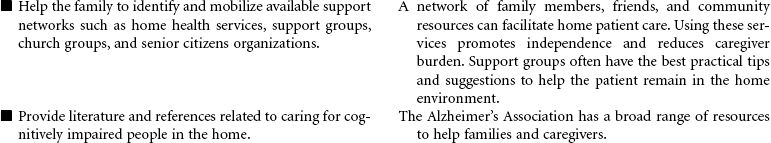
Alzheimer’s Disease/Dementia
![]() For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
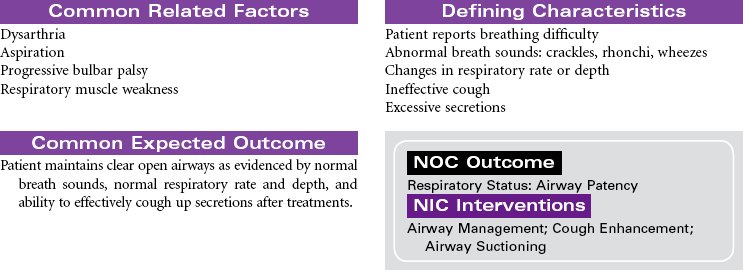
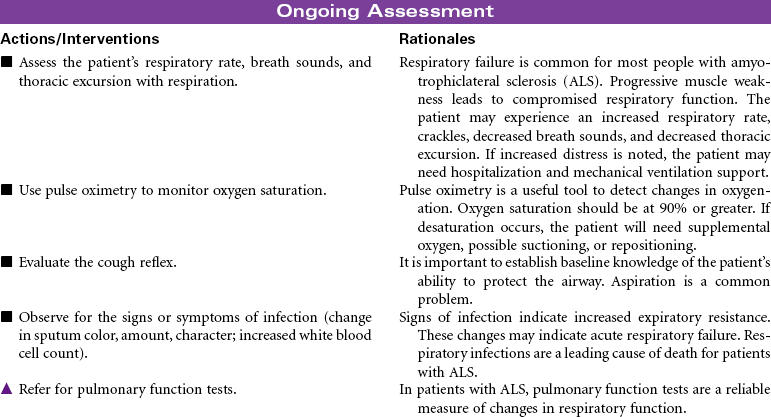
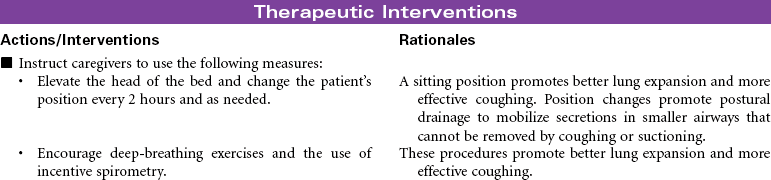
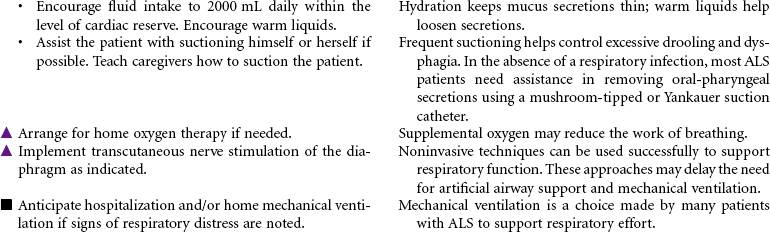
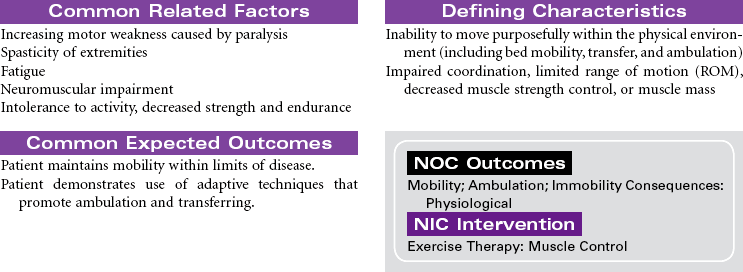
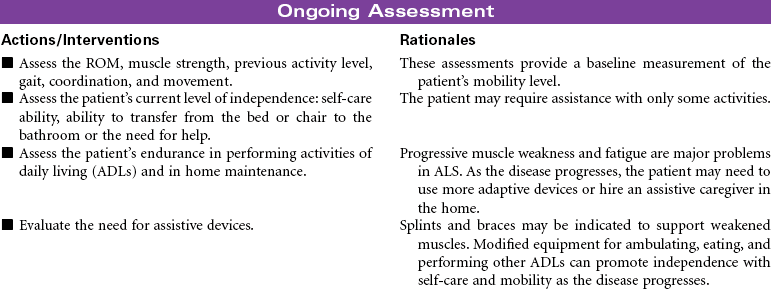
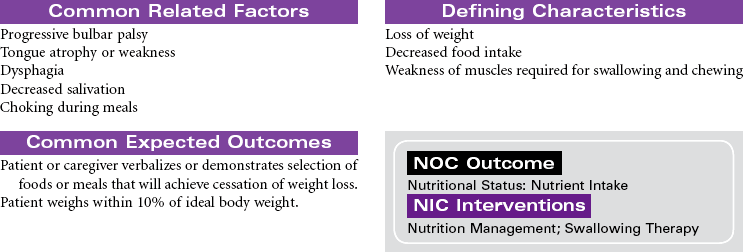
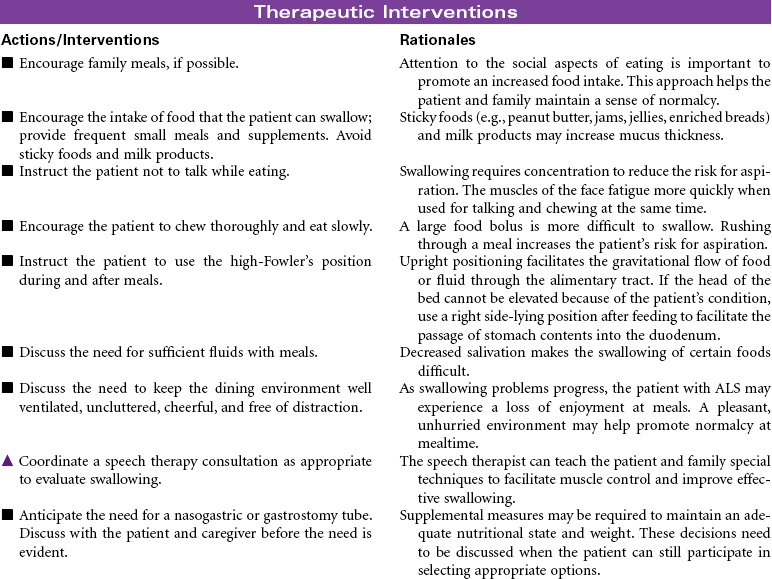
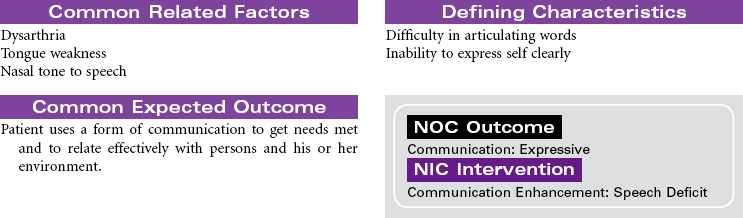
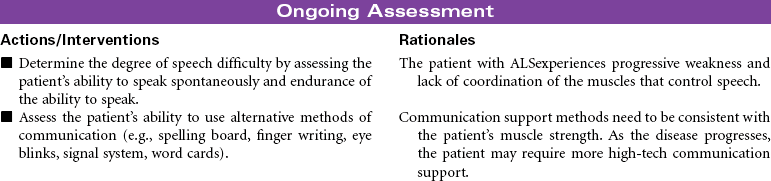
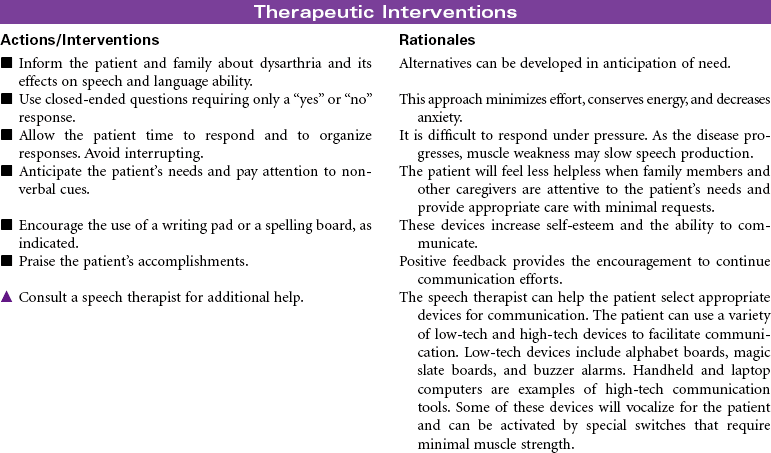
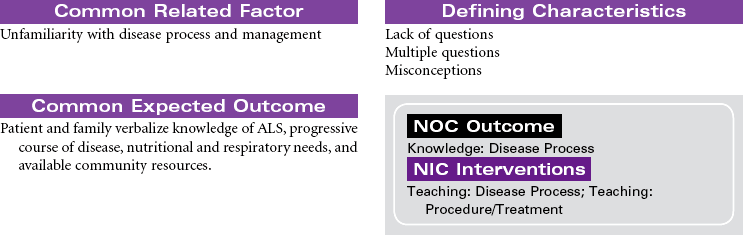
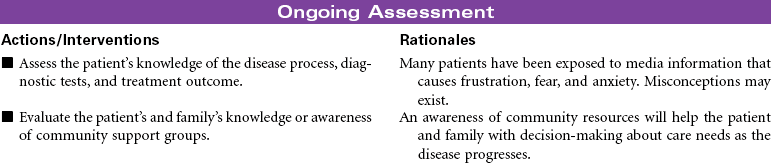
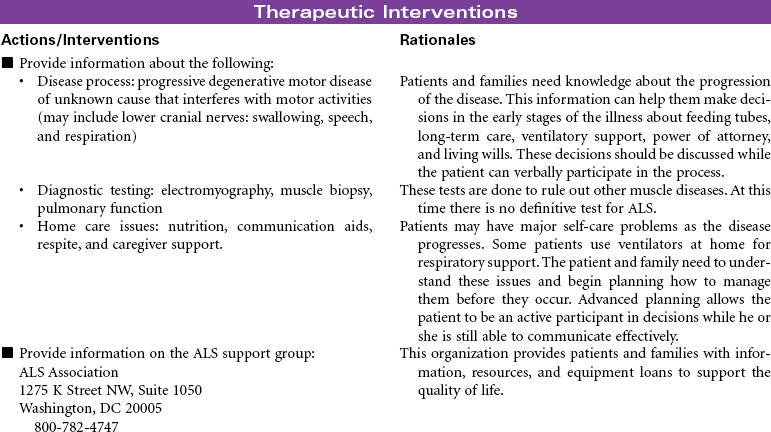
Amyotrophic Lateral Sclerosis
Neurological Care Plans
Get Clinical Tree app for offline access

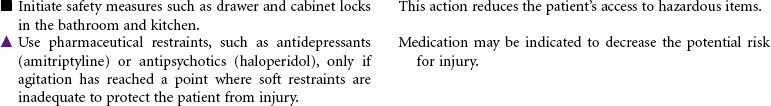
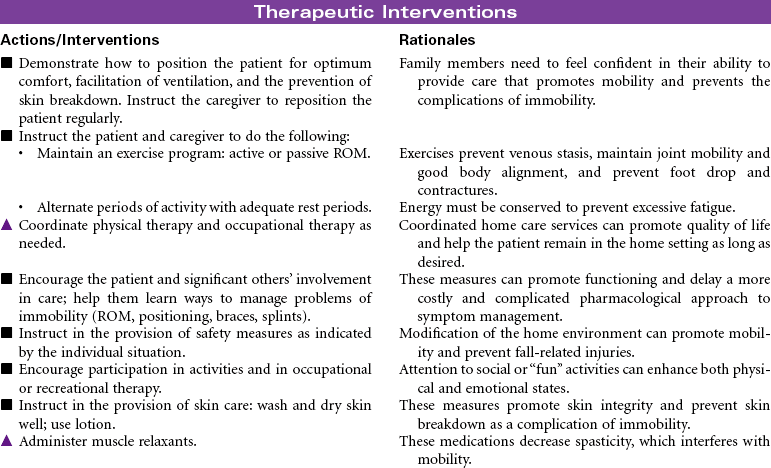
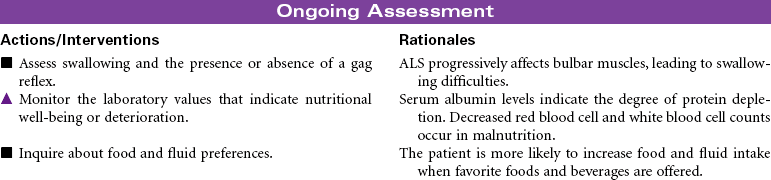
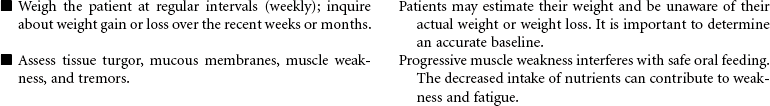
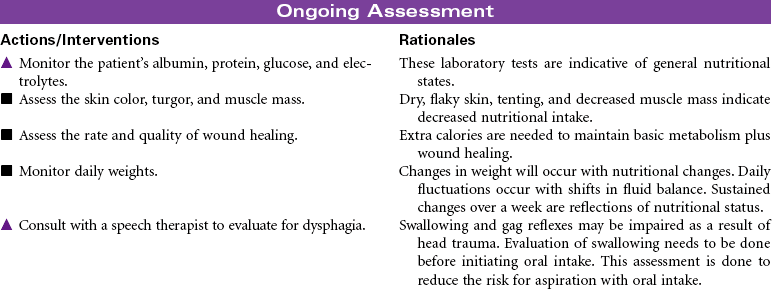
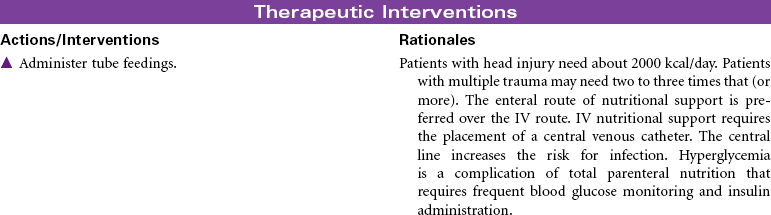
 = Independent
= Independent  = Collaborative
= Collaborative
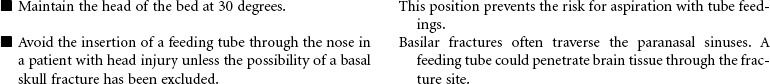
 = Independent
= Independent  = Collaborative
= Collaborative