Nervous System and Musculo-Skeletal Disorders
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the care required for arthritis and osteoporosis.
• Explain how to assist in the care of persons after total joint replacement surgery.
• Explain how to assist in the care of persons in casts, in traction, and with hip fractures.
• Describe the effects of amputation.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| ADL | Activities of daily living |
| ALS | Amyotrophic lateral sclerosis |
| CVA | Cerebrovascular accident |
| JRA | Juvenile rheumatoid arthritis |
| MS | Multiple sclerosis |
| RA | Rheumatoid arthritis |
| ROM | Range-of-motion |
| TBI | Traumatic brain injury |
| TIA | Transient ischemic attack |
Understanding nervous and musculo-skeletal disorders gives meaning to the required care. Refer to Chapter 10 while you study this chapter.
Nervous System Disorders
Nervous system disorders can affect mental and physical function. They can affect the ability to speak, understand, feel, see, hear, touch, think, control bowels and bladder, and move.
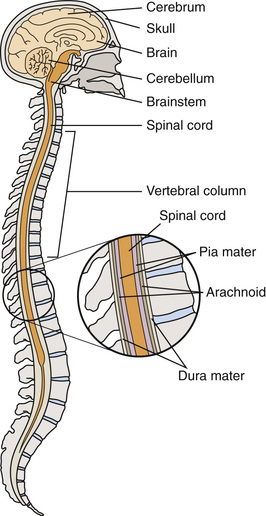
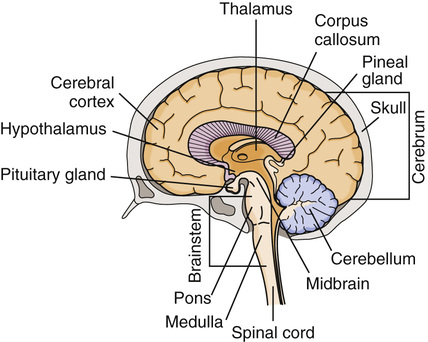
See Body Structure and Function Review: The Nervous System, p. 706.
Stroke
Stroke (brain attack or cerebrovascular accident [CVA]) occurs when 1 of these happens.
• A blood vessel in the brain bursts and bleeds into the brain (cerebral hemorrhage).
• A blood clot blocks a blood vessel in the brain. Blood flow stops.
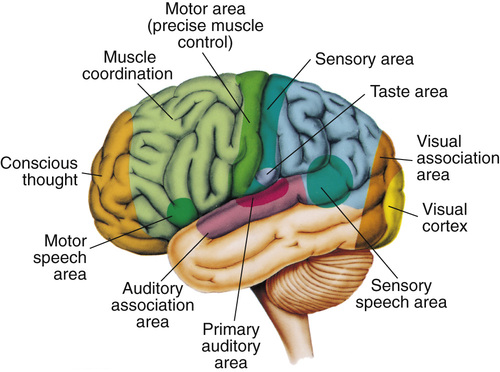
Brain cells in the affected area do not get enough oxygen and nutrients. Brain damage occurs. Functions controlled by that part of the brain are lost (Fig. 44-3).
Stroke is a leading cause of death in the United States. It is a leading cause of disability in adults. See Box 44-1 for warning signs. The person needs emergency care. Blood flow to the brain must be restored as soon as possible.
Warning signs may last a few minutes. This is called a transient ischemic attack ( TIA). (Transient means temporary or short term. Ischemic means to hold back [ischein] blood [hemic].) Blood supply to the brain is interrupted for a short time. A TIA may occur before a stroke. All stroke-like symptoms signal the need for emergency care.
Risk Factors.
Risk factors include:
Signs and Symptoms.
Stroke can occur suddenly. The person may have warning signs (see Box 44-1). The person also may have nausea, vomiting, and memory loss. Unconsciousness, noisy breathing, high blood pressure, slow pulse, redness of the face, and seizures may occur. So can hemiplegia—paralysis (plegia) on 1 side (hemi) of the body. The person may lose bowel and bladder control and the ability to speak. (See “Aphasia” in Chapter 42.)
Effects on the Person.
If the person survives, some brain damage is likely. The entire body may be affected. Functions lost depend on the area of brain damage (see Figure 44-3). They include:
• Loss of face, hand, arm, leg, or body control
• Changing emotions (crying easily or mood swings sometimes for no reason)
• Difficulty swallowing (dysphagia)
• Aphasia or slowed or slurred speech (Chapter 42)
• Changes in sight, touch, movement, and thought
• Urinary frequency, urgency, or incontinence
• Loss of bowel control or constipation
The person may forget about or ignore the weaker side. This is called neglect. It is from the loss of vision or movement and feeling on that side. Sometimes thinking is affected. The person may not recognize or know how to use common items. Activities of daily living (ADL) and other tasks are hard to do. The person may forget what to do and how to do it. If the person does know, the body may not respond.
Rehabilitation starts at once. The goal is to regain the highest possible level of function (Box 44-2, p. 708).
See Focus on Long-Term Care and Home Care: Effects on the Person (Stroke), p. 708.
Parkinson’s Disease
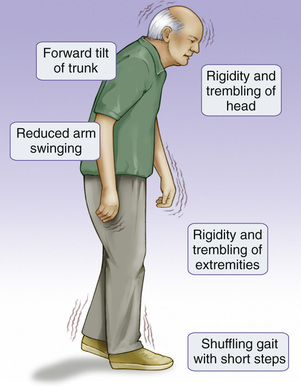
Parkinson’s disease is a progressive disorder affecting movement. Persons over the age of 50 are at risk. One or both sides of the body are affected. Signs and symptoms are mild at first (Fig. 44-4). They include:
• Rigid, stiff muscles—in the arms, legs, neck, and trunk.
• Stooped posture and impaired balance—it is hard to walk. Falls are a risk.
• Mask-like expression—the person cannot blink and smile. A fixed stare is common.
Other signs and symptoms develop over time. They include swallowing and chewing problems, constipation, sleep problems, depression, and emotional changes (fear, insecurity). Memory loss and slow thinking can occur. The person may have slow, monotone, and soft speech.
With no cure, drugs are ordered to control the disease. Exercise and physical therapy help improve strength, posture, balance, and mobility. Therapy is needed for speech and swallowing problems. The person may need help with eating and self-care. Normal elimination is a goal. Safety measures are needed to prevent falls and injuries.
Multiple Sclerosis
Multiple sclerosis (MS) is a central nervous system disease. Multiple means many. Sclerosis means hardening or scarring. The myelin (which covers nerve fibers) in the brain and spinal cord is destroyed. Nerve impulses are not sent to and from the brain in a normal way. Functions are impaired or lost.
Symptoms usually start between the ages of 20 and 40. Women and whites are at greater risk than other groups. The risk increases if a family member has MS. Signs and symptoms may include:
• Blurred or double vision; blindness in 1 eye
• Muscle weakness in the arms and legs
• Balance and coordination problems
• Tingling, prickling, or numb sensations
• Partial or complete paralysis
• Pain
• Tremors
• Concentration, attention, memory, and judgment problems
• Problems with sexual function
• Fatigue
MS can present in many ways. For example:
MS has no cure. Some drugs can slow the disease. Persons with MS are kept as active and as independent as possible. The care plan reflects changing needs. Skin care, hygiene, and ROM exercises are important. So are turning, positioning, and deep breathing and coughing. Elimination needs are met. Injuries and complications from bedrest are prevented.
See Focus on Long-Term Care and Home Care: Multiple Sclerosis.
Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) attacks the nerve cells that control voluntary muscles. Commonly called Lou Gehrig’s disease, it is rapidly progressive and fatal. (Lou Gehrig was a New York Yankees baseball player who died of the disease.)
ALS usually strikes persons between 40 and 60 years of age. Most die 2 to 5 years after onset.
The disease attacks the nerve cells responsible for voluntary muscles. Such cells are in the brain, brainstem, and spinal cord. These cells stop sending messages to the muscles. The muscles weaken, waste away (atrophy), and twitch. Over time, the brain cannot start voluntary movements or control them. The person cannot move the arms, legs, and body. Muscles for speaking, chewing and swallowing, and breathing also are affected. Eventually respiratory muscles fail. The person needs a ventilator to breathe (Chapter 40).
The disease usually does not affect the mind, intelligence, or memory. However, some persons develop dementia. Sight, smell, taste, hearing, and touch are not affected. Usually bowel and bladder functions remain intact.
ALS has no cure. Some drugs can slow the disease and improve symptoms. However, damage cannot be reversed. The person is kept active and independent to the extent possible. The care plan reflects changing needs. It may include:
• Physical, occupational, and speech-language therapies
• Mobility aides—braces, walker, wheelchair
• Comfort and pain-relief measures
• Dysphagia diet or feeding tube
• Respiratory support—suctioning, mechanical ventilation
• Safety measures to prevent falls and injuries
• Psychological and social support
Head Injuries
Head injuries result from trauma to the scalp, skull, or brain. Injuries range from a minor bump to a serious, life-threatening brain injury. Traffic accidents, falls, assaults, and gunshots are common causes. So are home, work, sports, and outdoor accidents.
Head injuries are open or closed. Bleeding may occur.
• Closed—a hard blow to the head did not break the skull.
• Open (penetrating)—an object broke the skull and entered the brain.
Symptoms may develop at the time of the injury. Or they can take several hours or days to develop. Symptoms are from bleeding or swelling inside the skull.
Most head injuries need emergency care. See Chapter 54.
Traumatic Brain Injury.
Traumatic brain injury (TBI) occurs from violent injury to the brain—bumps, blows, or jolts to the head or penetrating injuries. Common causes include:
TBI results in bruised or torn brain tissue. Bleeding is in the brain or in nearby tissues. Spinal cord injuries are likely.
Men, infants and children, young adults, and older persons are at risk for TBI. Death can occur at the time of injury or later. See Box 44-3 for the signs and symptoms of TBI.