Medication Administration
Objectives
• Differentiate routes of administration.
• Compare and contrast the various sites for parenteral therapy.
• Explain the equipment and technique used in parenteral therapy.
• Explain documenting medication administration.
• Analyze the nursing interventions related to administration of medications by various routes.
• Apply the nursing process to the administration of medication.
Key Terms
buccal, p. 134
inhalation, p. 134
instillations, p. 135
intradermal, p. 138
intramuscular, p. 138
intraosseous, p. 138
intravenous, p. 138
meniscus, p. 134
metered-dose inhaler, p. 136
parenteral, p. 134
spacers, p. 137
subcutaneous, p. 138
sublingual, p. 134
suppository, p. 134
topical, p. 135
transdermal, p. 135
Z-track technique, p. 138
Administration of medications is a basic activity in nursing practice. As a result of the transition from hospitals and institutions to community-based services, an increasing number of nurses are practicing in a variety of settings. Nurses therefore must be knowledgeable about specific drugs and their administration, patient response, drug interactions, patient allergies, and related resources. Safety and prevention of medication errors are essential (see Chapter 12).
Self-Administration of Medication
Self-administration of medication (SAM) is common in the home and in many community-based settings like the workplace. However, SAM is relatively new to patients and staff in institutional settings. In practical terms, SAM means that the nurse gives the patient the appropriate medications and instructions that are kept at the bedside and then go home with the patient on discharge. Patients are responsible for taking their medication according to the instructions. Patients play a key role in and exercise control associated with taking selected medications. SAM allows patients to manage their medications during the hospital admission and prepares them to manage their medications at home for optimal benefits. Refer to Chapters 53 and 54 for a description of SAM for maternity patients and Chapter 12 for the “five-plus-five rights,” the “do’s and don’ts” of medication administration, factors that alter drug responses, high-alert medications, and pregnancy categories.
Forms and Routes for Drug Administration
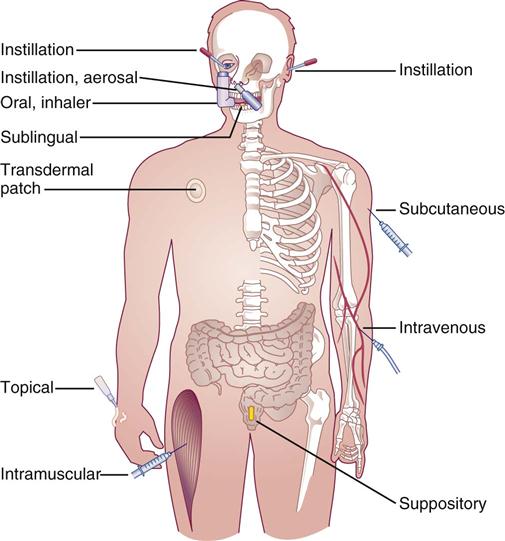
A variety of forms and routes are used for the administration of medications, including sublingual, buccal, oral (tablets, capsules, liquids, suspensions, elixirs), transdermal, topical, instillation (drops and sprays), inhalation, nasogastric and gastrostomy tubes, suppositories, and parenteral (Figure 13-1).
Tablets and Capsules
Liquids
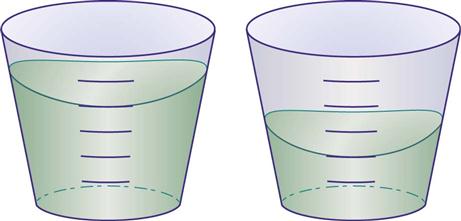
• The meniscus is the slightly concave curved line of a dose of liquid. The bottom of the meniscus should be used to measure the desired dose of medication (Figure 13-2).
Transdermal
Topical
Instillations
Instillations are liquid medications usually administered as drops, ointment, or sprays in the following forms:
• Eyedrops (Box 13-1 and Figure 13-3)
• Eye ointment (Box 13-2 and Figure 13-4)
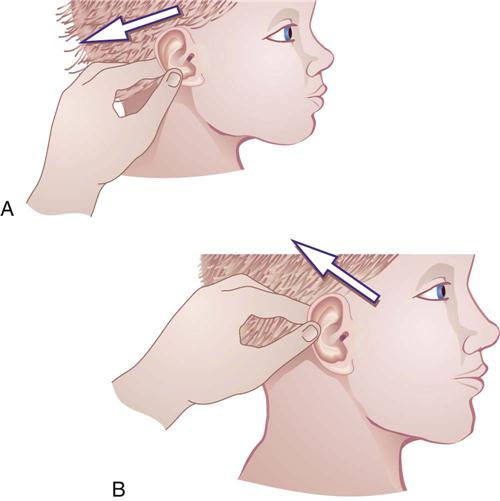
• Eardrops (Box 13-3 and Figure 13-5)
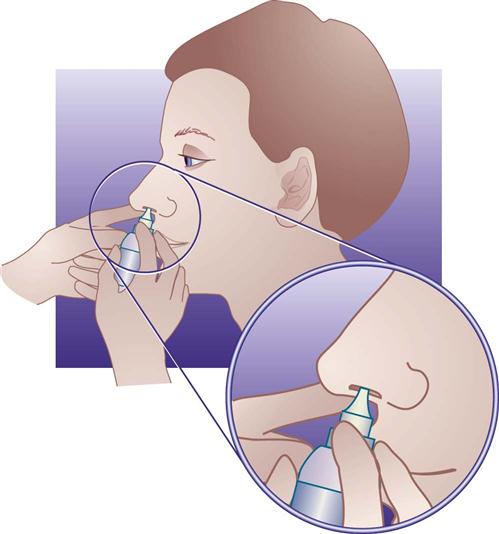
• Nose drops and sprays (Box 13-4 and Figures 13-6 and 13-7)

 -inch–wide strip of ointment onto the conjunctival sac.
-inch–wide strip of ointment onto the conjunctival sac.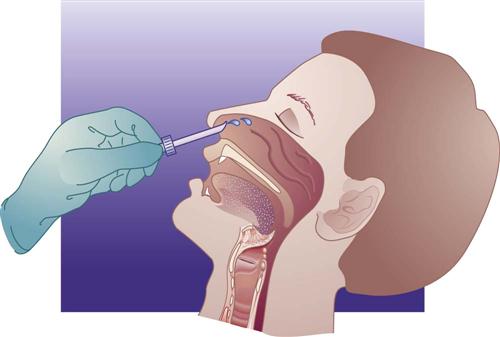
Inhalations
• Metered-dose inhalers (MDIs) are handheld devices that deliver medication to the lower respiratory tract (Box 13-5). Some MDIs have a counter to indicate the number of inhalations used. For those that do not, the most accurate way to determine this number is for the patient to count and record (e.g., on the box or a calendar) the number of inhalations used; however, this is often not practical. Inhalation counters are now on some inhalation products and are a most welcome addition. Every effort should be made to have the patient know how much medication is in the canister and to anticipate/obtain refills in a timely manner.
• Spacers are devices used to enhance the delivery of medications from the MDI. Figure 13-8 illustrates the distribution of medication with and without a spacer. A nebulizer is a device that changes a liquid medication into a fine mist or aerosol that has the ability to reach the lower, smaller airways. Handheld nebulizers deliver a very-fine–sized particle spray of medication.
• Instruct the patient on the correct use and cleaning of MDIs or nebulizers.
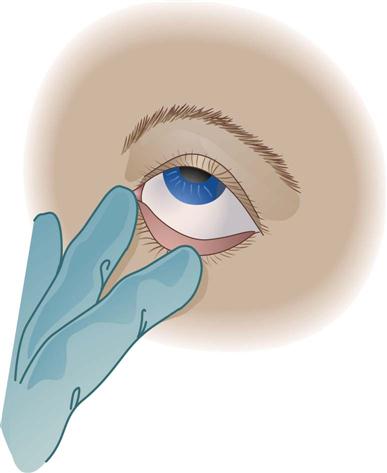
 inch unless stated otherwise) onto conjunctival sac. Medication placed directly on the cornea can cause discomfort or damage. Avoid touching eyelids or eyelashes with tip of applicator.
inch unless stated otherwise) onto conjunctival sac. Medication placed directly on the cornea can cause discomfort or damage. Avoid touching eyelids or eyelashes with tip of applicator.