Measuring Vital Signs
Objectives
• Define the key terms and key abbreviations in this chapter.
• Explain why vital signs are measured.
• List the factors affecting vital signs.
• Identify the normal ranges for each temperature site.
• Explain when to use each temperature site.
• Explain how to use thermometers.
• Describe a normal pulse and normal respirations.
• Describe the practices to follow when measuring blood pressure.
• Perform the procedures described in this chapter.
• Know the normal vital signs for the different age-groups.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| BP | Blood pressure |
| C | Centigrade |
| DUS | Doppler ultrasound stethoscope |
| F | Fahrenheit |
| Hg | Mercury |
| ID | Identification |
| IV | Intravenous |
| mm | Millimeter |
| mm Hg | Millimeters of mercury |
| TPR | Temperature, pulse, and respirations |
Vital signs reflect the function of 3 body processes essential for life: regulation of body temperature, breathing, and heart function. The vital signs of body function are:
Vital signs are often called TPR (temperature, pulse, and respirations) and BP (blood pressure). Some agencies include “pain” as a vital sign (p. 511 and Chapter 31). Also see “Pulse Oximetry” in Chapter 39.
Measuring and Reporting Vital Signs
A person’s vital signs vary within certain limits. See Box 29-1 for the factors affecting vital signs.
Vital signs are measured to detect changes in normal body function. They tell about treatment response. They often signal life-threatening events. Vital signs are part of the assessment step in the nursing process. Vital signs are measured:
• When the person is admitted to a health care agency
• As often as the person’s condition requires
• Before and after surgery, complex procedures, and diagnostic tests
• After some care measures, such as ambulation (walking)
• After a fall or other injury
• When drugs affect the respiratory or circulatory system
• As stated on the care plan (usually daily, twice a day, or weekly in nursing centers)
Vital signs show even minor changes in the person’s condition. Accuracy is essential when you measure, record, and report vital signs. If unsure of your measurements, promptly ask the nurse to take them again. Unless otherwise ordered, take vital signs with the person at rest—lying or sitting. Report the following at once.
• Any vital sign that is changed from a prior measurement
• An abnormal vital sign (a vital sign above or below the normal range)
Vital signs are recorded in the person’s medical record. If measured often, a flow sheet may be used. The doctor or nurse compares past and current measurements.
See Focus on Communication: Measuring and Reporting Vital Signs.
See Focus on Children and Older Persons: Measuring and Reporting Vital Signs.
Body Temperature
Body temperature is the amount of heat in the body. It is a balance between the amount of heat produced and the amount lost by the body. Heat is produced as cells use food for energy. It is lost through the skin, breathing, urine, and feces. Body temperature is fairly stable. It is lower in the morning and higher in the afternoon and evening. Body temperature is affected by the factors listed in Box 29-1, pregnancy, and the menstrual cycle.
You use thermometers to measure temperature. Temperature is measured using the Fahrenheit (F) and centigrade (C) scales. The degrees symbol (°) is used to record temperatures.
Temperature Sites
Temperature sites are the mouth, rectum, axilla (underarm), tympanic membrane (ear), and temporal artery (forehead) (Box 29-2). Each site has a normal range (Table 29-1). Always report temperatures above or below the normal range.
TABLE 29-1
Normal Body Temperatures
| Site | Baseline | Normal Range |
| Oral | 98.6°F (37.0°C) | 97.6°F to 99.6°F (36.5°C to 37.5°C) |
| Rectal | 99.6°F (37.5°C) | 98.6°F to 100.6°F (37.0°C to 38.1°C) |
| Axillary | 97.6°F (36.5°C) | 96.6°F to 98.6°F (35.9°C to 37.0°C) |
| Tympanic membrane | 98.6°F (37.0°C) | 98.6°F (37.0°C) |
| Temporal artery | 99.6°F (37.5°C) | 99.6°F (37.5°C) |
Fever means an elevated body temperature. These terms are used to describe the person.
See Focus on Communication: Temperature Sites.
See Focus on Children and Older Persons: Temperature Sites.
See Promoting Safety and Comfort: Temperature Sites.
Thermometers
A thermometer is a device used to measure (meter) temperature (thermo). Follow the manufacturer’s instructions and agency procedures to use, clean, and store thermometers.
Electronic Thermometers.
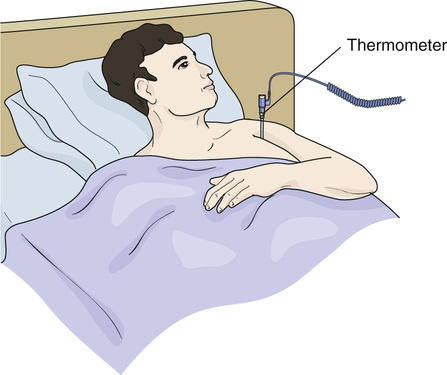
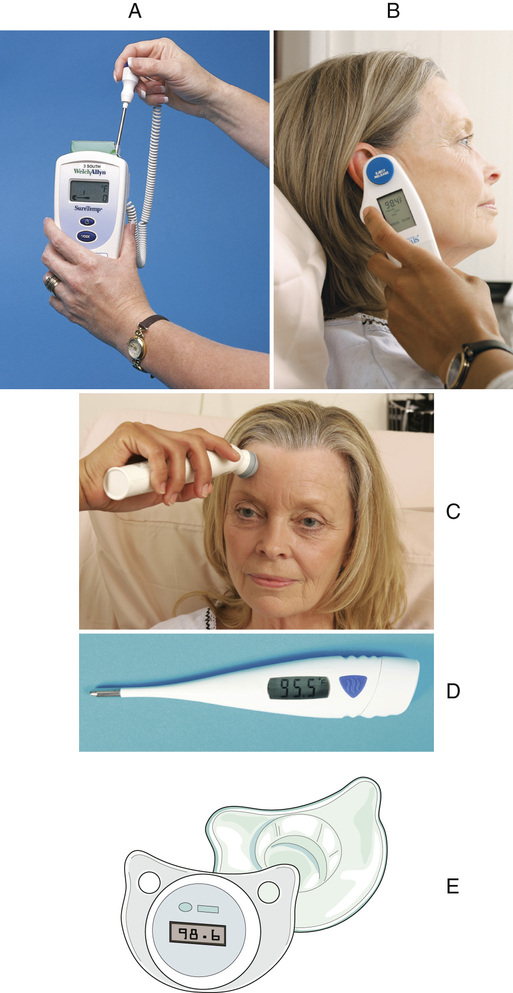
Electronic thermometers show the temperature on the front of the device. Probe covers prevent the spread of infection. Battery operated, they are kept in chargers when not in use.
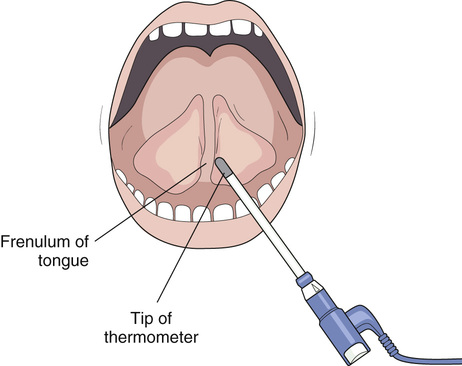
• Standard electronic thermometers—measure body temperature at the oral, rectal, and axillary sites in a few seconds. They have oral (blue) and rectal (red) probes. The oral (blue) probe is also used for axillary temperatures. A disposable cover (sheath) protects the probe. See Figure 29-1, A.
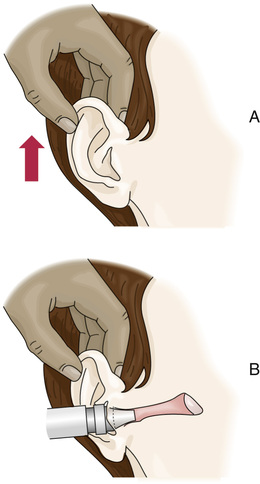
• Tympanic membrane thermometers—measure body temperature at the tympanic membrane in the ear in 1 to 3 seconds (Fig. 29-1, B). They are comfortable and not invasive. There are fewer microbes in the ear than in the mouth or rectum. The risk of spreading infection is reduced. These devices are not used if there is ear drainage. To use one, gently insert the covered probe into the ear.
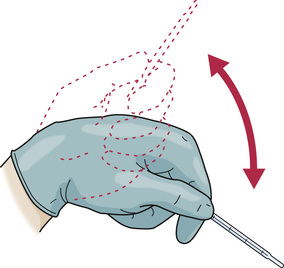
• Temporal artery thermometers—measure body temperature at the temporal artery in the forehead in 3 to 4 seconds (Fig. 29-1, C ). Non-invasive, they measure the temperature of the blood in the temporal artery. It is the same temperature of the blood coming from the heart. To use one:
2. Place a disposable cap or cover on the thermometer.
3. Place the device in the center of the forehead.
5. Slide the device across the forehead and across the temporal artery (see Fig. 29-1, C).
7. Read the temperature display.
• Digital thermometers—measure body temperature at the oral, rectal, and axillary sites. Depending on the type, the temperature is measured in 6 to 60 seconds. See Figure 29-1, D.
• Pacifier thermometers—look like a baby’s pacifier (Fig. 29-1, E ). The baby sucks on the device for 90 seconds. The temperature is displayed on the front.
See Teamwork and Time Management: Electronic Thermometers.
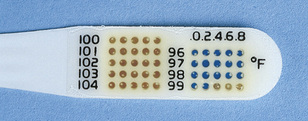
Disposable Oral Thermometers.
Small chemical dots change color when heated (Fig. 29-2). Each dot is heated to a certain temperature before it changes color. Used once, these thermometers measure temperature in 45 to 60 seconds.
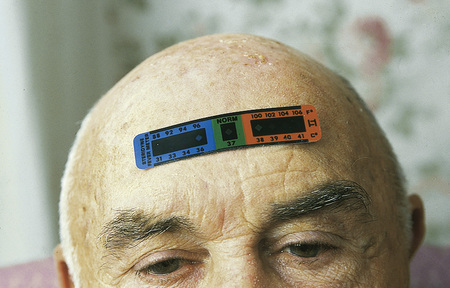
Temperature-Sensitive Tape.
The tape is applied to the forehead and changes color in response to body heat (Fig. 29-3). The measurement takes about 15 seconds.
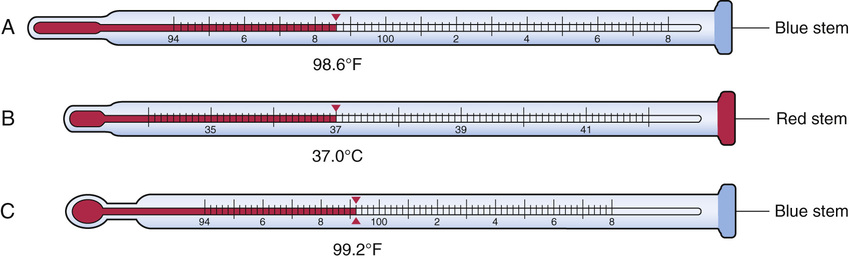
Glass Thermometers.
Glass thermometers have a hollow glass tube and a bulb tip (Fig. 29-4). The device is filled with a substance. When heated, the substance expands and rises in the tube. When cooled, the substance contracts and moves down the tube.
Long- or slender-tip thermometers are used for oral and axillary temperatures. So are thermometers with stubby and pear-shaped tips. Rectal thermometers have stubby tips. See Figure 29-4.
Glass thermometers are color-coded.
Glass thermometers are re-usable. However, the following are problems.
• They take a long time to register—3 to 10 minutes depending on the site (p. 494).
• They break easily. Broken rectal thermometers can injure the rectum and colon.
See Focus on Long-Term Care and Home Care: Glass Thermometers.
See Promoting Safety and Comfort: Glass Thermometers.
Taking Temperatures
The nurse and care plan tell you:
See Focus on Children and Older Persons: Taking Temperatures.
See Delegation Guidelines: Taking Temperatures.
See Promoting Safety and Comfort: Taking Temperatures.
 Taking Temperatures With Electronic Thermometers.
Taking Temperatures With Electronic Thermometers.
There are many types of electronic thermometers. Follow the manufacturer’s instructions. The procedure that follows is used as a guide.
See procedure: Taking a Temperature With an Electronic Thermometer, p. 492.
 Taking Temperatures With Glass Thermometers.
Taking Temperatures With Glass Thermometers.
While uncommon in hospitals and nursing centers, glass thermometers may be used in homes. See Box 29-3 for how to use and read glass thermometers.

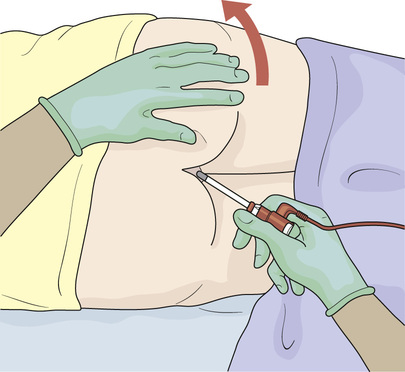
 inch into the rectum.
inch into the rectum.