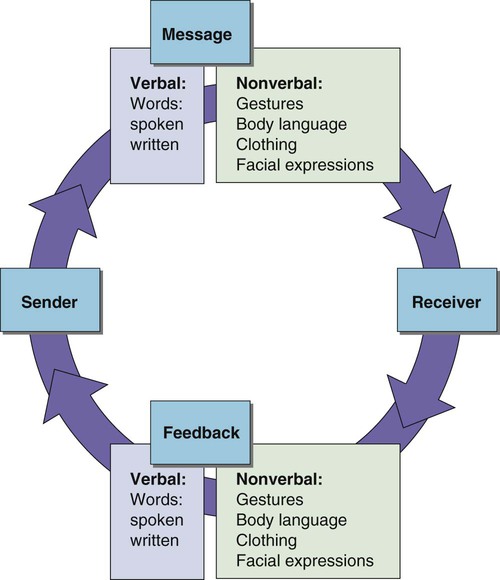
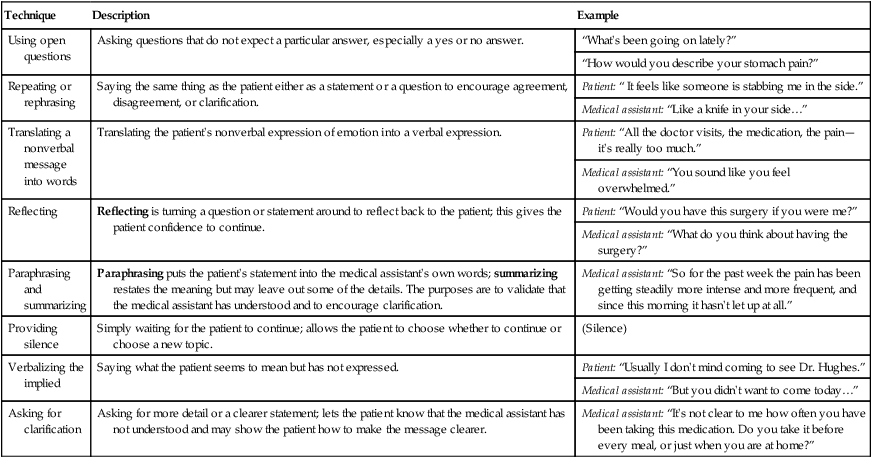
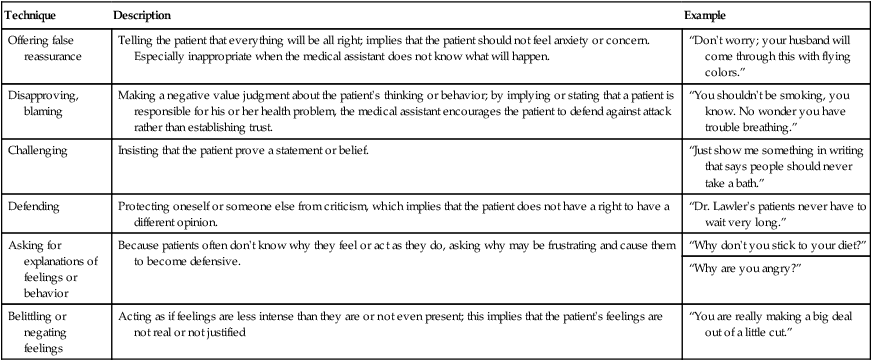
1. Describe the steps in the communication process. 2. Differentiate between verbal and nonverbal communication. 3. List several types of nonverbal communication. 4. Identify and describe factors that can interfere with effective communication. 5. Explain the elements of active listening. 6. Describe how eye contact can have different meanings based on cultural background. 7. Give examples of techniques that encourage a patient to continue speaking. 8. Explain how to overcome sensory and language barriers to communication. 9. Describe ways to evaluate if communication has been effective. Establishing Relationships to Meet Patient Needs 10. List factors that affect patient expectations of health care. 11. Explain the levels of Maslow’s hierarchy of needs. 12. Correlate the existence of unmet needs to types of patient behavior in the health care setting. 13. List several ways to establish caring relationships with patients. 14. Describe the importance of maintaining appropriate personal boundaries 15. Explain the role of empathy in the relationship between the medical assistant and patients. 16. Describe how the medical assistant can handle common emotional responses to illness. 17. Clarify how empathy helps improve the relationship between the medical assistant and the patient. 18. Describe ways to support the terminally ill patient in all stages of the grieving process. 19. Demonstrate respect for diversity in approaching patients and families. Figure 4-1 outlines the basic model of communication. A sender sends a message to a receiver. The message can be verbal, meaning that spoken or written words are used to send the message. It can also be nonverbal, meaning the message is expressed without words through body language, facial expression, and other means. Most messages are sent using a combination of verbal and nonverbal communication. The feedback from the receiver to the sender, also verbal or nonverbal, helps the sender decide whether to initiate a new message, expand on the original message, or clarify the message. Nonverbal communication refers to information that is received from body language. Body language is the way a person’s body signals feelings or emotions. For example, hands folded across the chest and a rigid posture may signal anger. Nonverbal communication also includes the secondary communication that occurs during oral conversation. Secondary communication consists of tone of voice, voice pitch, voice volume, and voice quality. Nonverbal communication often provides more information than the words themselves (Figure 4-2). 1. Checking to make sure the patient’s interpretation of a message is correct. This may involve asking the patient to repeat what has been said by rephrasing a question. 2. Listening for feelings. Medical assistants should be alert for key words or themes the patient uses frequently to describe his or her medical condition. These can be important clues as to the patient’s emotional state. The medical assistant should also be aware of changes in his or her own feelings. The medical assistant’s emotions may mirror the emotions of patients. For example, if the medical assistant begins to get impatient or aggravated with a patient, it may be a clue that the patient is upset or angry. 3. Being observant while listening. The patient’s facial expressions, body language, tone of voice, and other nonverbal cues can tell a lot about what the patient is feeling. 4. Being patient and listening completely. Patients should be allowed to “tell their story” in their own time and in their own way. Interruption interferes with this process. Although there are questions that need to be asked, the medical assistant should introduce questions in a way that interferes as little as possible with the patient’s natural storytelling flow. In the United States, eye contact is important (Figure 4-3). Maintaining eye contact is a sign of interest and involvement. However, being aware that in many cultures it is not respectful to look directly at older people is important. This is especially true in Asian and Native American cultures. Many Latinos also do not look directly at a person they respect, such as a teacher or a physician. Active listening includes techniques to draw a patient out and/or clarify what a patient is saying. This is especially important when the patient is trying to cope with strong feelings about his or her medical problems. Refer to Table 4-1 for a full listing of communication techniques that demonstrate active listening. Table 4-1 Communication Techniques That Demonstrate Active Listening The responses that should be avoided are summarized in Table 4-2. Table 4-2 Responses That Inhibit Communication
Interacting with Patients
Introduction to Communication
Communicating with Patients
Verbal and Nonverbal Communication
Listening Skills
Nonverbal Measures to Facilitate Communication
Interviewing Techniques
Drawing Patients Out
Technique
Description
Example
Using open questions
Asking questions that do not expect a particular answer, especially a yes or no answer.
“What’s been going on lately?”
“How would you describe your stomach pain?”
Repeating or rephrasing
Saying the same thing as the patient either as a statement or a question to encourage agreement, disagreement, or clarification.
Patient: “ It feels like someone is stabbing me in the side.”
Medical assistant: “Like a knife in your side…”
Translating a nonverbal message into words
Translating the patient’s nonverbal expression of emotion into a verbal expression.
Patient: “All the doctor visits, the medication, the pain—it’s really too much.”
Medical assistant: “You sound like you feel overwhelmed.”
Reflecting
Reflecting is turning a question or statement around to reflect back to the patient; this gives the patient confidence to continue.
Patient: “Would you have this surgery if you were me?”
Medical assistant: “What do you think about having the surgery?”
Paraphrasing and summarizing
Paraphrasing puts the patient’s statement into the medical assistant’s own words; summarizing restates the meaning but may leave out some of the details. The purposes are to validate that the medical assistant has understood and to encourage clarification.
Medical assistant: “So for the past week the pain has been getting steadily more intense and more frequent, and since this morning it hasn’t let up at all.”
Providing silence
Simply waiting for the patient to continue; allows the patient to choose whether to continue or choose a new topic.
(Silence)
Verbalizing the implied
Saying what the patient seems to mean but has not expressed.
Patient: “Usually I don’t mind coming to see Dr. Hughes.”
Medical assistant: “But you didn’t want to come today…”
Asking for clarification
Asking for more detail or a clearer statement; lets the patient know that the medical assistant has not understood and may show the patient how to make the message clearer.
Medical assistant: “It’s not clear to me how often you have been taking this medication. Do you take it before every meal, or just when you are at home?”
Avoiding Responses That Inhibit Communication
Technique
Description
Example
Offering false reassurance
Telling the patient that everything will be all right; implies that the patient should not feel anxiety or concern. Especially inappropriate when the medical assistant does not know what will happen.
“Don’t worry; your husband will come through this with flying colors.”
Disapproving, blaming
Making a negative value judgment about the patient’s thinking or behavior; by implying or stating that a patient is responsible for his or her health problem, the medical assistant encourages the patient to defend against attack rather than establishing trust.
“You shouldn’t be smoking, you know. No wonder you have trouble breathing.”
Challenging
Insisting that the patient prove a statement or belief.
“Just show me something in writing that says people should never take a bath.”
Defending
Protecting oneself or someone else from criticism, which implies that the patient does not have a right to have a different opinion.
“Dr. Lawler’s patients never have to wait very long.”
Asking for explanations of feelings or behavior
Because patients often don’t know why they feel or act as they do, asking why may be frustrating and cause them to become defensive.
“Why don’t you stick to your diet?”
“Why are you angry?”
Belittling or negating feelings
Acting as if feelings are less intense than they are or not even present; this implies that the patient’s feelings are not real or not justified
“You are really making a big deal out of a little cut.”
Interacting with Patients
Get Clinical Tree app for offline access