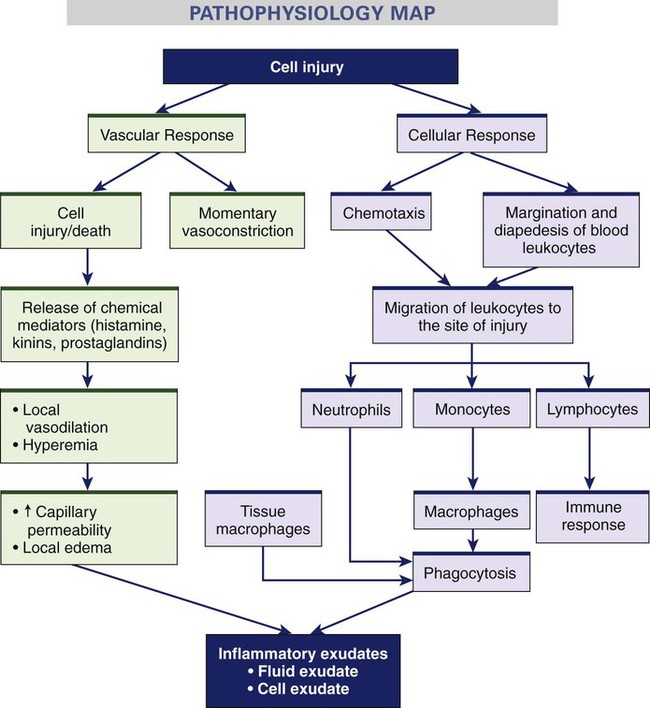
Chapter 12 1. Describe the inflammatory response, including vascular and cellular responses and exudate formation. 2. Explain local and systemic manifestations of inflammation and their physiologic bases. 3. Describe the drug therapy, nutrition therapy, and nursing management of inflammation. 4. Differentiate among healing by primary, secondary, and tertiary intention. 5. Describe the factors that delay wound healing and common complications of wound healing. 6. Describe the nursing and collaborative management of wound healing. 7. Explain the etiology and clinical manifestations of pressure ulcers. 8. Apply a patient risk assessment for pressure ulcers to measures used to prevent the development of pressure ulcers. 9. Discuss nursing and collaborative management of a patient with pressure ulcers. The mechanism of inflammation is basically the same regardless of the injuring agent. The intensity of the response depends on the extent and severity of injury and on the injured person’s reactive capacity. The inflammatory response can be divided into a vascular response, a cellular response, formation of exudate, and healing. Fig. 12-1 illustrates the vascular and cellular response to injury. eTABLE 12-1 WOUND CLASSIFICATION BY ETIOLOGY eTABLE 12-2 Category I: Skin tears without tissue loss. Linear types: skin is pulled apart with a linear tear. Flap types: an epidermal flap covers within 1 mm of the wound margin. Category II: Skin tears with partial tissue loss. Scant tissue loss types: Less than 25% or less of the epidermal flap is lost. Moderate to large types: More than 25% of the epidermal flap is lost. Grade 0: No open lesion but may have deformity or cellulitis Grade 1: Superficial ulcer, partial or full-thickness Grade 2: Ulcer extends to ligament, tendon, joint capsule, or fascia; no abscess or osteomyelitis Grade 3: Deep ulcer with abscess, osteomyelitis, or joint sepsis Grade 4: Gangrene localized to forefoot or heel Stages eTABLE 12-3 BRADEN SCALE FOR PREDICTING PRESSURE SORE RISK Copyright © Barbara Braden and Nancy Bergstrom. All rights reserved. Available at www.bradenscale.com. From Braden B, Bergstrom N: Predictive validity of the Braden scale for pressure sore risk in a nursing home population, Res Nurs Health 17:459, 1994. eTABLE 12-4 PRESSURE ULCER SCALE FOR HEALING (PUSH) 4. Necrotic tissue (eschar): Black, brown, or tan tissue that adheres firmly to the wound bed or ulcer edges and may be either firmer or softer than surrounding skin. 3. Slough: Yellow or white tissue that adheres to the ulcer bed in strings or thick clumps, or is mucinous. 2. Granulation tissue: Pink or beefy red tissue with a shiny, moist, granular appearance. 1. Epithelial tissue: For superficial ulcers, new pink or shiny tissue (skin) that grows in from the edges or as islands on the ulcer surface. 0. Closed/resurfaced: The wound is completely covered with epithelium (new skin).
Inflammation and Wound Healing
Inflammatory Response
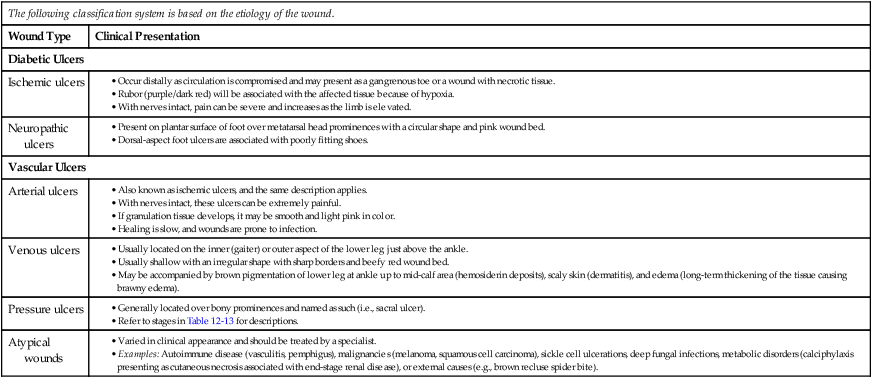
Classification System
Description
Clinical Use
Surgical
Wounds are approximated and heal by primary intention if there are no complications.
All surgical incisions
Depth of Skin Destruction (superficial, partial, and full thickness)
Superficial has intact and inflamed tissue, partial thickness involves only dermis and epidermis, and full thickness extends through the dermis.
Abrasions, burns, skin grafts including donor sites
NPUAP Staging
See Table 12-13 in text
Pressure ulcers only
Payne-Martin
Skin tears
Meggit-Wagner
Originally developed to classify diabetic foot ulcers. This system has been modified and used with other ulcers and wounds because of descriptors of tissue depth, infection, and necrosis.
University of Texas
Grading
Originally developed for diabetic foot wounds. Has been validated in other locations. This system uses two tiers; grades a wound 0-3 and uses stage descriptors A-D to more specifically describe the wound.
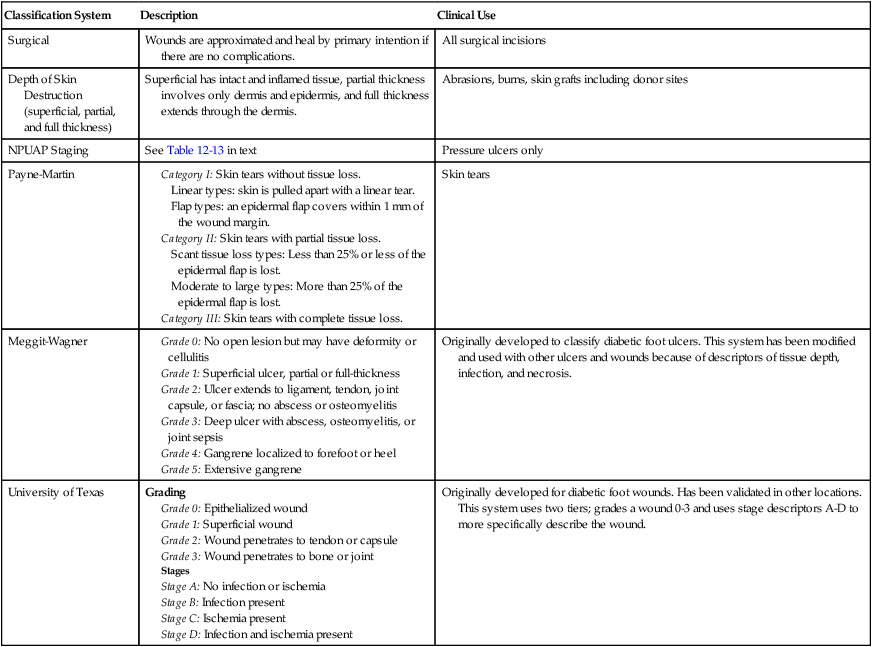
Patient Name ____________________________________
Evaluator’s Name _______________________________
Point Value
Date of Assessment and Score
1
2
3
4
Sensory Perception: Ability to Respond Meaningfully to Pressure-Related Discomfort
Completely limited: unresponsive (does not moan, flinch, or grasp) to painful stimuli, because of diminished level of consciousness or sedation
OR
limited ability to feel pain over most of body
Very limited: responds only to painful stimuli; cannot communicate discomfort except by moaning or restlessness
OR
has a sensory impairment that limits the ability to feel pain or discomfort over half of body
Slightly limited: responds to verbal commands, but cannot always communicate discomfort or the need to be turned
OR
has some sensory impairment that limits ability to feel pain or discomfort in one or two extremities
No impairment: responds to verbal commands; has no sensory deficit that would limit ability to feel or to voice pain or discomfort
Moisture: Degree to Which Skin Is Exposed to Moisture
Constantly moist: skin is kept moist almost constantly by perspiration, urine, etc.; dampness is detected every time patient is moved or turned
Very moist: skin is often, but not always, moist; linen must be changed at least once per shift
Occasionally moist: skin is occasionally moist, requiring an extra linen change approximately once per day
Rarely moist: skin is usually dry; linen only requires changing at routine intervals
Activity: Degree of Physical Activity
Bedfast: confined to bed
Chairfast: ability to walk severely limited or nonexistent; cannot bear own weight and/or must be assisted into chair or wheelchair
Walks occasionally: walks occasionally during day, but for very short distances, with or without assistance; spends most of each shift in bed or chair
Walks frequently: walks outside room at least twice per day and inside room at least once every 2 hours during waking hours
Mobility: Ability to Change and Control Body Position
Completely immobile: does not make even slight changes in body or extremity position without assistance
Very limited: makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently
Slightly limited: makes frequent although slight changes in body or extremity position independently
No limitation: makes major and frequent changes in position without assistance
Nutrition: Usual Food Intake Pattern
Very poor: never eats a complete meal; rarely eats more than half of any food offered; eats two servings or less of protein (meat or dairy products) per day; takes fluids poorly; does not take a liquid dietary supplement or is NPO and/or maintained on clear liquids or IVs for more than 5 days
Probably inadequate: rarely eats a complete meal and generally eats only about half of any food offered; protein intake includes only three servings of meat or dairy products per day; occasionally will take a dietary supplement or receives less than optimum amount of liquid diet or tube feeding
Adequate: eats over half of most meals; eats four servings of protein (meat or dairy products) per day; occasionally will refuse a meal, but will usually take a supplement when offered or is on a tube feeding or parenteral nutrition regimen that probably meets most nutritional needs
Excellent: eats most of every meal; never refuses a meal; eats four or more servings of protein (meat or dairy products); occasionally eats between meals; does not require supplementation
Friction and Shear
Problem: requires moderate to maximum assistance in moving; complete lifting without sliding against sheets is impossible; frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance; spasticity, contractures, or agitation lead to almost constant friction
Potential problem: moves feebly or requires minimum assistance; during a move, skin probably slides to some extent against sheets, chair, restraints, or other devices; maintains relatively good position in chair or bed most of the time but occasionally slides down
No apparent problem: moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move; maintains good position in bed or chair
Scoring: To obtain a patient’s pressure ulcer risk assessment score, add the numeric scores for the factors in each of the six subscales (sensory perception, moisture, activity, mobility, nutrition, and friction and shear) to obtain the total score. Scores can range from 6 to 23. The lower the numeric score, the higher the patient’s predicted risk of developing a pressure ulcer. Incremental changes in the score indicate the level of risk: no risk (19 to 23), at risk (15 to 18), moderate risk (13 to 14), high risk (10 to 12), and very high risk (9 or below).
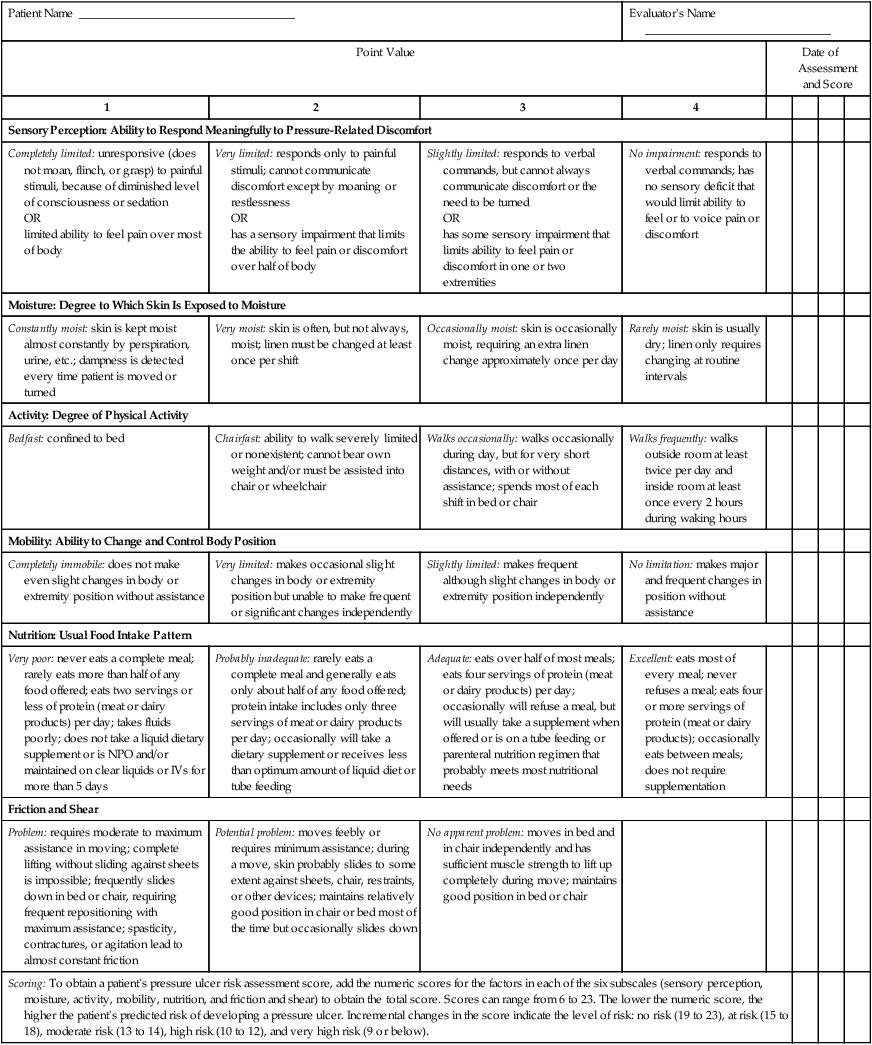
PUSH Tool 3.0
Patient Name ___________________________________
Patient ID# __________________
Ulcer Location ___________________________________
Date _______________________
Directions
Observe and measure the pressure ulcer. Categorize the ulcer with respect to surface area, exudate, and type of wound tissue. Record a sub-score for each of these ulcer characteristics. Add the sub-scores to obtain the total score. A comparison of total scores measured over time provides an indication of the improvement or deterioration in pressure ulcer healing.
LENGTH × WIDTH (in cm2)
0
0
1
<0.3
2
0.3-0.6
3
0.7-1.0
4
1.1-2.0
5
2.1-3.0
Sub-score
6
3.1-4.0
7
4.1-8.0
8
8.1-12.0
9
12.1-24.0
10
>24.0
EXUDATE AMOUNT
0
None
1
Light
2
Moderate
3
Heavy
Sub-score
TISSUE TYPE
0
Closed
1
Epithelial Tissue
2
Granulation Tissue
3
Slough
4
Necrotic Tissue
Sub-score
TOTAL SCORE
Length × Width
Measure the greatest length (head to toe) and the greatest width (side to side) using a centimeter ruler. Multiply these two measurements (length × width) to obtain an estimate of surface area in square centimeters (cm2). caveat: Do not guess! Always use a centimeter ruler and always use the same method each time the ulcer is measured.
Exudate Amount
Estimate the amount of exudate (drainage) present after removal of the dressing and before applying any topical agent to the ulcer. Estimate the exudate (drainage) as none, light, moderate, or heavy.
Tissue Type
This refers to the types of tissue that are present in the wound (ulcer) bed. Score as a “4” if there is any necrotic tissue present. Score as a “3” if there is any amount of slough present and necrotic tissue is absent. Score as a “2” if the wound is clean and contains granulation tissue. A superficial wound that is reepithelializing is scored as a “1.” When the wound is closed, score as a “0.”
www.npuap.org PUSH Tool Version 3.0: 9/15/98.
11F ©National Pressure Ulcer Advisory Panel.
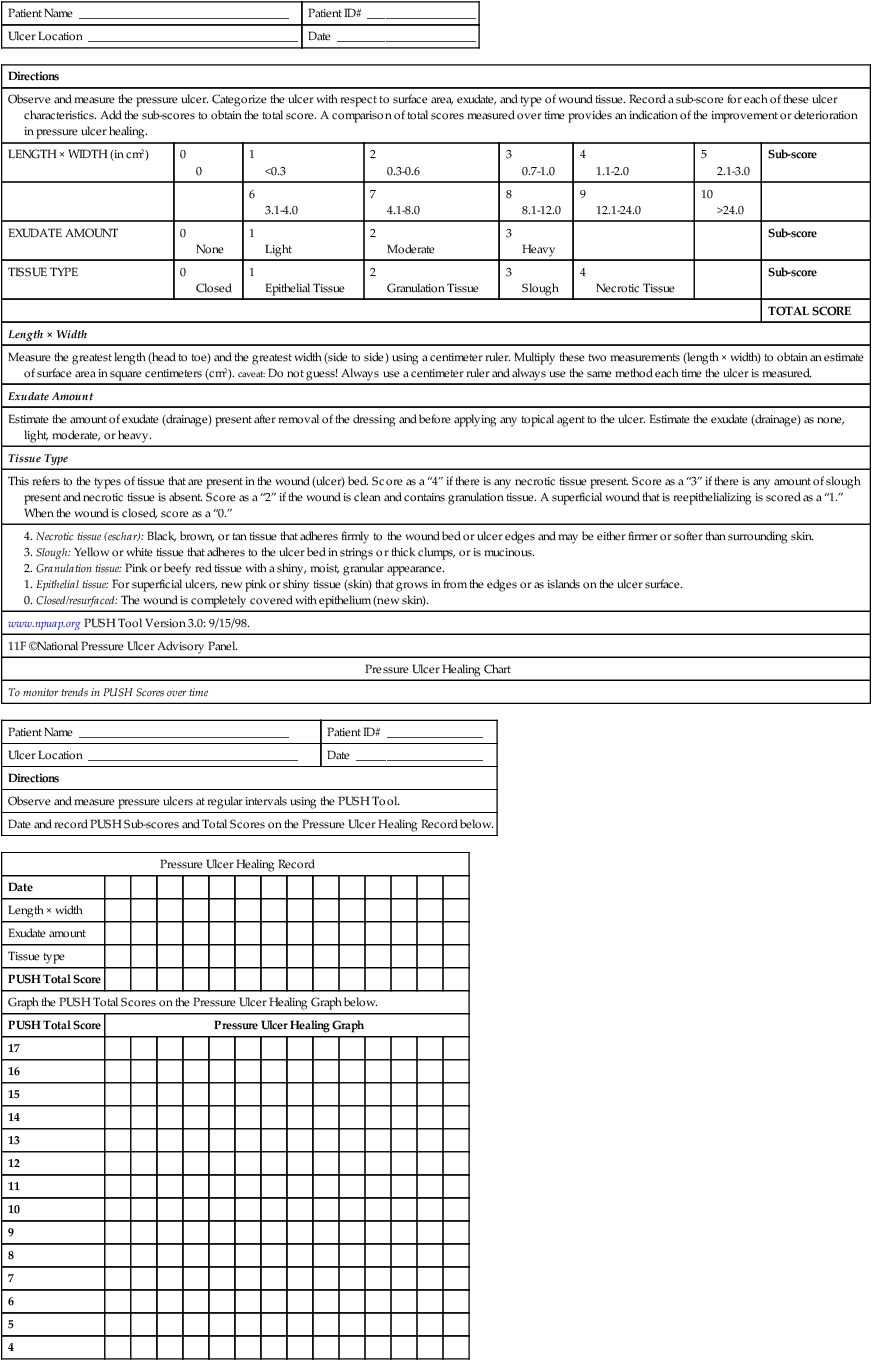
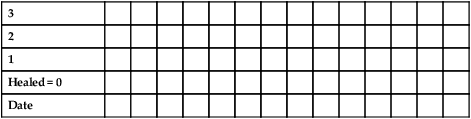
Pressure Ulcer Healing Chart
To monitor trends in PUSH Scores over time
Patient Name ___________________________________
Patient ID# ________________
Ulcer Location ___________________________________
Date _____________________
Directions
Observe and measure pressure ulcers at regular intervals using the PUSH Tool.
Date and record PUSH Sub-scores and Total Scores on the Pressure Ulcer Healing Record below.
Pressure Ulcer Healing Record
Date
Length × width
Exudate amount
Tissue type
PUSH Total Score
Graph the PUSH Total Scores on the Pressure Ulcer Healing Graph below.
PUSH Total Score
Pressure Ulcer Healing Graph
17
16
15
14
13
12
11
10
9
8
7
6
5
4
3
2
1
Healed = 0
Date
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Inflammation and Wound Healing
Get Clinical Tree app for offline access