Infectious Disease Prevention and Control
Objectives
After reading this chapter, the student should be able to do the following:
1. Discuss the current impact and threats of infectious diseases on society.
2. Explain how the elements of the epidemiologic triangle interact to cause infectious diseases.
4. Explain the multisystem approach to control of communicable diseases.
5. Define surveillance and discuss the functions and elements of a surveillance system.
6. Discuss the factors contributing to newly emerging or reemerging infectious diseases.
9. Describe issues and agents associated with foodborne illness and appropriate prevention measures.
10. Define the bloodborne pathogen reduction strategy and universal precautions.
Key Terms
acquired immunity, p. 289
active immunization, p. 289
agent, p. 289
common vehicle, p. 290
communicable diseases, p. 286
communicable period, p. 290
disease, p. 290
elimination, p. 294
emerging infectious diseases, p. 291
endemic, p. 291
environment, p. 289
epidemic, p. 290
epidemiologic triangle, p. 288
eradication, p. 294
herd immunity, p. 289
horizontal transmission, p. 290
hospital-acquired infection, p. 312
host, p. 289
incubation period, p. 290
infection, p. 290
infectiousness, p. 289
natural immunity, p. 289
pandemic, p. 290
passive immunization, p. 289
resistance, p. 290
surveillance, p. 290
universal precautions, p. 312
vectors, p. 290
vertical transmission, p. 290
—See Glossary for definitions
 Francisco S. Sy, MD, DrPH
Francisco S. Sy, MD, DrPH
Dr. Francisco S. Sy is the Director of the Division of Extramural Activities and Scientific Programs at the National Center on Minority Health and Health Disparities (NCMHD) at the National Institutes of Health (NIH) in Bethesda, MD. Before joining NIH, Dr. Sy served as a Senior Health Scientist in the Division of HIV/AIDS Prevention (DHAP), National Center for HIV, STD and TB Prevention (NCHSTP), at the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. Dr. Sy was a tenured professor at the University of South Carolina (USC) School of Public Health in Columbia, SC, where he taught infectious disease epidemiology for 15 years. At USC, he served as Graduate Director of the Department of Epidemiology and Biostatistics for 7 years and as Director of the school-wide Master of Public Health (MPH) program for 3 years. Dr. Sy has written several book chapters and scientific articles on various infectious and tropical diseases, HIV disease epidemiology, prevention, and program evaluation. He is the Editor of the AIDS Education and Prevention: An Interprofessional Journal since its inception in 1988. It is a bimonthly peer-reviewed journal published by Guilford Press in New York. Dr. Sy earned his Doctor of Public Health (DrPH) degree in Immunology and Infectious Diseases from Johns Hopkins University in 1984, Master of Science in Tropical Public Health from Harvard University in 1981, and Doctor of Medicine degree from the University of the Philippines in 1975.
 Susan C. Long-Marin, DVM, MPH
Susan C. Long-Marin, DVM, MPH
Susan C. Long-Marin developed an interest in infectious disease and public health while serving as a Peace Corps Volunteer in the Philippines in the 1970s. Training in veterinary medicine further increased her respect for the ingeniousness of microbes and the importance of primary prevention. Today she manages the epidemiology program of a county health department in Charlotte, NC, which serves a growing and rapidly changing population from a variety of racial, ethnic, and national backgrounds.
The topic of infectious diseases includes the discussion of a wide and complex variety of organisms; the pathology they may cause; and their diagnosis, treatment, prevention, and control. This chapter presents an overview of the communicable diseases that nurses encounter most often. Diseases are grouped according to descriptive category (by mode of transmission or means of prevention) rather than by individual organism (e.g., Escherichia coli) or taxonomic group (e.g., viral, parasitic). Detailed discussion of sexually transmitted diseases, human immunodeficiency virus (HIV), acquired immunodeficiency syndrome (AIDS), viral hepatitis, and tuberculosis (TB) is provided in Chapter 14. Although not all infectious diseases are directly communicable from person to person, the terms infectious disease and communicable disease are used interchangeably throughout this chapter.
Historical and Current Perspectives
In the United States, at the beginning of the twentieth century, infectious diseases were the leading cause of death. By 2000 improvements in nutrition and sanitation, the discovery of antibiotics, and the development of vaccines had put an end to infectious disease epidemics like diphtheria and typhoid fever that once ravaged entire populations. In 1900 respiratory and diarrheal diseases were major killers. For example, TB led to over 11% of all deaths in the United States and was the second leading cause of death; by the early twenty-first century, only 0.02% of all deaths were attributed to this once frequently fatal disease (CDC, 2009a). As individuals live longer, chronic diseases—heart disease, cancer, and stroke—have replaced infectious diseases as the leading causes of death.
Infectious diseases, however, have by no means vanished, and they remain a continuing cause for concern. They persist as the third-leading cause of death in the United States and the second-leading cause worldwide, where they are responsible for killing an estimated 15 million people a year (Fauci, Touchette, and Folkers, 2005). In the United States, the downward trend in mortality from infectious diseases, seen since 1900—with the exception of the 1918 influenza pandemic—reversed itself in the 1980s, with the emergence of new entities such as HIV disease and the increasing development of antibiotic resistance. Respiratory diseases in the form of pneumonias and influenza remain among the 10 leading causes of death, and new strains such as novel influenza A H1N1 and avian influenza A H5N1 test our disease control abilities and consume resources. Previously unknown causal connections between infectious organisms and chronic diseases have been recognized, such as Helicobacter pylori and peptic ulcer disease, and human papillomaviruses (HPVs) and cervical cancer. Also, in the twenty-first century, infectious diseases have become a means of terrorism, as illustrated by the anthrax letters of 2001.
New killers emerge and old familiar diseases take on different, more virulent characteristics. Consider the following developments from the past 30 years. HIV disease reminds us of plagues from the past and challenges our ability to control and contain infection like no other disease in recent history. Because drugs have been developed to slow the progression but there is still neither vaccine nor cure, this initially infectious disease is now a chronic condition as well. Legionnaires’ disease and toxic shock syndrome, unknown at mid-twentieth century, have become part of common vocabulary. The identification of infectious agents causing Lyme disease and ehrlichiosis provided two new tickborne diseases to worry about. And, in the summer of 1993 in the southwestern United States, healthy young adults were stricken with a mysterious and unknown but often fatal respiratory disease that is now known as hantavirus pulmonary syndrome. The summer of 1994 brought public attention to a severe, invasive strain of Streptococcus pyogenes group A, referred to by the press as the “flesh-eating” bacteria.
In the 1990s the transmission of infectious disease through the food supply became a newsworthy concern when the consumption of improperly cooked hamburgers and unpasteurized apple juice contaminated with a highly toxic strain of E. coli (E. coli 0157:H7) caused illness and death in children across the country. In 1996 multiple states reported outbreaks of diarrheal disease traced to imported fresh berries; the implicated organism in these outbreaks, Cyclospora cayetanensis (a coccidian parasite), was only first diagnosed in humans in 1977. Also in 1996, the fear that “mad cow disease” (bovine spongiform encephalopathy [BSE]) could be transferred to humans through beef consumption led to the slaughter of thousands of British cattle and a ban on the international sale of British beef. Initially seen only in Europe and Japan as well as Great Britain, the first case of BSE was diagnosed in the United States in 2003. Variant Creutzfeldt-Jakob disease (vCJD), which attacks the brain with fatal results, is the human disease hypothesized but not yet proven to result from eating beef infected with the transmissible agent causing BSE; only three acquired cases of vCJD have been seen in the United States, but these individuals were born outside of and resided in the country for only a short period (CDC, 2009b).
In 1997 vancomycin-resistant Staphylococcus aureus (VRSA) was first reported; previously, vancomycin had been considered the only effective antibiotic against methicillin-resistant S. aureus (MRSA). Although MRSA is still largely a hospital-acquired infection, community-associated disease is becoming more common with outbreaks frequently associated with school athletic programs and prison populations. Also in 1997, the first reported outbreak of avian flu affecting humans occurred in Hong Kong. No subsequent reports suggested an isolated incident, but in 2004, avian influenza A H5N1 again emerged in Southeast Asia with resulting human cases. This virus has now infected avian populations in Asia, Europe, the Near East, and North Africa, and it continues to cause sporadic human cases, especially in Southeast Asia and Egypt. Human cases are determined to largely spread through direct contact with infected poultry or infected surfaces, with human to human transmission largely ineffective and only a few rare cases thought to have occurred. In 1999 the first western hemisphere activity of West Nile virus (WNV), a mosquito-transmitted illness that can affect livestock, birds, and humans, occurred in New York City. By 2002 WNV, thought to be carried by infected birds and possibly mosquitoes in cargo containers, had spread across the United States as far west as California and was reported in Canada and Central America as well.
The viral hemorrhagic fevers Ebola and Marburg, unknown to most people 30 years ago, have become the premise of movies and books. Although caused by different viruses within the Filoviridae family, these sporadically occurring but lethal killers have similar clinical presentations. The most recent large outbreaks of Ebola have been in 2007 in the Democratic Republic of the Congo (249 cases, 183 deaths) and in Uganda (149 cases, 37 deaths). Marburg virus had only been reported five times since its recognition in 1967 before a major outbreak in Angola occurred during 2004 and 2005, affecting more than 350 people with a fatality rate of close to 90%. Since then, a much smaller outbreak occurred in Uganda in 2007 among gold miners. The source for both of these viruses is still undetermined, but there is an association with non-human primates, and evidence is also beginning to point toward a bat reservoir (Heymann, 2008).
Severe acute respiratory syndrome (SARS) was first recognized in China in February 2003. And as if in a bestselling thriller, this newly emerging infectious disease quickly achieved pandemic proportions. By the summer of 2003, major outbreaks had occurred in Hong Kong, Taiwan, Vietnam, Singapore, and Canada. Three months after the first official news of SARS, over 8000 cases with more than 700 deaths had been reported to the World Health Organization (WHO) from 28 countries. Played out on television in pictures of people wearing face masks for protection, the rapid spread of a previously unknown disease with an initially unknown cause and no definitive treatment contributed to the creation of a perception of risk of infection far greater than actually existed. Frightened Americans canceled trips to China and Hong Kong and avoided people who had recently returned from Asia. Then, as suddenly as it began, the pandemic subsided. SARS was eventually determined to be caused by a new strain of Coronavirus, but since 2003, only a few cases, largely associated with laboratory workers, have been reported. A large number of individuals infected by SARS could be traced back to unrecognized cases in hospitals, suggesting that prompt identification and isolation of symptomatic people is the key to interrupting transmission. Global efforts continue to clarify the epidemiology of this disease as well as develop a reliable diagnostic test and vaccine. Additional information on SARS can be obtained at the WHO Global Alert and Response website (http://www.who.int/csr/sars/).
In the first decade of the twenty-first century, foodborne infections again have made headlines as E. coli–infected spinach sickened and killed individuals across the United States. In 2008, tomatoes were blamed for a nation-wide outbreak of salmonellosis but were ruled innocent when the green chilies that accompanied them in salsa were found to be the actual culprit. Salmonella again made the news as contaminated peanut butter forced recalls across the United States, sickened hundreds, and resulted in several deaths. Even chocolate chip cookie dough was not safe; a national recall in 2009 followed the discovery that people had been sickened after eating raw dough contaminated by E. coli. Perhaps the most publicized infectious disease event of 2009 was the advent of a new strain of flu, novel influenza A H1N1. First reported from Mexico and rapidly acquired by travelers to that country, H1N1 spread quickly across the world, causing the WHO to declare a pandemic and stimulate the race for a vaccine.
Worldwide, infectious diseases are the leading killer of children and young adults and are responsible for almost half of all deaths in developing countries. Of these infectious disease deaths, 90% result from six causes: acute respiratory infections, diarrheal diseases, malaria and measles among children; and TB and HIV infection among adults. Malaria alone is estimated to kill 1.2 million people a year and TB another 1.7 million (or over 4600 people per day) (Heymann, 2008). The CDC in its Ounce of Prevention campaign notes that in the United States as many as 160,000 people die per year with infectious diseases as an underlying cause. The economic burden of infectious diseases is staggering. In the United States, the USDA Economic Research Service estimated the cost of foodborne illnesses caused by just two organisms—salmonella and E. coli 0157:H7—at over $3 billion in 2008 dollars (USDA, 2009). The Produce Safety Project at Georgetown University in 2010 suggested that the total cost from foodborne illness could be more than $152 billion (Pew Charitable Trusts, 2010). CDC researchers determined that in the United States in 2000, nine million cases of sexually transmitted infections occurred among young people 15 to 24 years of age with a total estimated cost of $6.5 billion, with HIV disease and HPV accounting for 90% of the total burden (Chesson et al, 2004). Hospital-acquired infections are estimated to have killed 48,000 people and cost $8.1 billion to treat in 2006 (Eber et al, 2010).
Because of the morbidity, mortality, and associated cost of infectious diseases, the national health promotion and disease prevention goals outlined in Healthy People 2020 list a number of objectives for reducing the incidence of these illnesses in the section on Immunization & Infectious Disease (see the Healthy People 2020 box). Objectives for reducing salmonellosis and other foodborne infections are found in the section on Food Safety and an objective for reducing malaria cases reported in the United States may be seen under Global Health. Although infectious diseases are not currently the leading causes of death in the United States, they continue to present varied, multiple and complex challenges to all health care providers. Nurses must know about these diseases to effectively participate in diagnosis, treatment, prevention, and control.
Transmission of Communicable Diseases
Agent, Host, and Environment
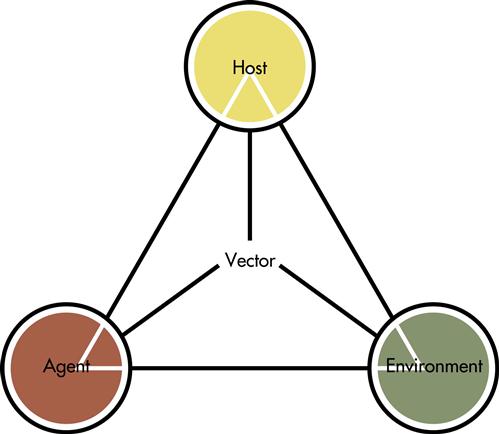
The transmission of communicable diseases depends on the successful interaction of the infectious agent, the host, and the environment. These three factors make up the epidemiologic triangle (Figure 13-1) as discussed in Chapter 12. Changes in the characteristics of any of the factors may result in disease transmission. Consider the following examples. Antibiotic therapy not only may eliminate a specific pathological agent, but also alter the balance of normally occurring organisms in the body. As a result, one of these agents overruns another and disease, such as a yeast infection, occurs. HIV performs its deadly work not by directly poisoning the host but by destroying the host’s immune reaction to other disease-producing agents. Individuals living in the temperate climate of the United States do not normally contract malaria at home, but they may become infected if they change their environment by traveling to a climate where malaria-carrying mosquitoes thrive. As these examples illustrate, the balance among agent, host, and environment is often precarious and may be unintentionally disrupted. At present, the potential results of such disturbance require attention as advances in science and technology, destruction of natural habitats, explosive population growth, political instability, and a worldwide transportation network combine to alter the balance among the environment, people, and the agents that produce disease.
Agent Factor
Four major categories of agents cause most infections and infectious disease: bacteria (e.g., Salmonella and E. coli); fungi (e.g., Aspergillus spp. and Candida spp.), parasites (e.g., helminthes and protozoa) and viruses (e.g., hepatitis A and B and HIV). Less commonly seen is the prion, a transmissible agent that causes abnormal folding of normal cellular prion proteins in the brain, resulting in a family of rare progressive neurodegenerative disorders that affect both humans and animals. Variant Creutzfeldt-Jakob disease and kuru are examples of prion diseases. The individual agent may be described by its ability to cause disease and by the nature and the severity of the disease. Infectivity, pathogenicity, virulence, toxicity, invasiveness and antigenicity, terms commonly used to characterize infectious agents, are defined in Box 13-1.
Host Factor
A human or animal host can harbor an infectious agent. The characteristics of the host that may influence the spread of disease are host resistance, immunity, herd immunity, and infectiousness of the host. Resistance is the ability of the host to withstand infection, and it may involve natural or acquired immunity.
Natural immunity refers to species-determined, innate resistance to an infectious agent. For example, opossums rarely contract rabies. Acquired immunity is the resistance acquired by a host as a result of previous natural exposure to an infectious agent. Having measles once protects against future infection. Acquired immunity may be induced by active or passive immunization. Active immunization refers to the immunization of an individual by administration of an antigen (infectious agent or vaccine) and is usually characterized by the presence of an antibody produced by the individual host. Vaccinating children against childhood diseases is an example of inducing active immunity. Passive immunization refers to immunization through the transfer of a specific antibody from an immunized individual to a non-immunized individual, such as the transfer of antibody from mother to infant or by administration of an antibody-containing preparation (immunoglobulin or antiserum). Passive immunity from immunoglobulin is almost immediate but short lived. It is often induced as a stopgap measure until active immunity has time to develop after vaccination. Examples of commonly used immunoglobulins include those for hepatitis A, rabies, and tetanus.
Herd immunity refers to the immunity of a group or community. It is the resistance of a group of people to invasion and spread of an infectious agent. Herd immunity is based on the resistance of a high proportion of individual members of a group to infection. It is the basis for increasing immunization coverage for vaccine-preventable diseases. Through studies, experts determine what percent coverage (e.g., >90%) of a specified group of people (e.g., children entering school) by a specified vaccine (e.g., one dose of measles vaccine) is necessary to ensure adequate protection for the entire community against a given disease and target immunization campaigns and initiatives to meet that goal. The higher the immunization coverage, the greater the herd immunity.
Infectiousness is a measure of the potential ability of an infected host to transmit the infection to other hosts. It reflects the relative ease with which the infectious agent is transmitted to others. Individuals with measles are extremely infectious; the virus spreads readily on airborne droplets. A person with Lyme disease cannot spread the disease to other people (although the infected tick can).
Environment Factor
The environment refers to everything that is external to the human host, including physical, biological, social, and cultural factors. These environmental factors facilitate the transmission of an infectious agent from an infected host to other susceptible hosts. Reduction in communicable disease risk can be achieved by altering these environmental factors. Using mosquito nets and repellants to avoid bug bites, installing sewage systems to prevent fecal contamination of water supplies, and washing utensils after contact with raw meat to reduce bacterial contamination are all examples of altering the environment to prevent disease.
Modes of Transmission
Infectious diseases can be transmitted horizontally or vertically. Vertical transmission is the passing of the infection from parent to offspring via sperm, placenta, milk, or contact in the vaginal canal at birth. Examples of vertical transmission are transplacental transmission of HIV and syphilis. Horizontal transmission is the person-to-person spread of infection through one or more of the following four routes: direct/indirect contact, common vehicle, airborne, or vector-borne. Most sexually transmitted infections are spread by direct sexual contact. Enterobiasis, or pinworm infection, can be acquired through direct contact or indirect contact with contaminated objects such as toys, clothing, and bedding. Common vehicle refers to transportation of the infectious agent from an infected host to a susceptible host via food, water, milk, blood, serum, saliva, or plasma. Hepatitis A can be transmitted through contaminated food and water, and hepatitis B through contaminated blood. Legionellosis and TB are both spread via contaminated droplets in the air. Vectors are arthropods such as ticks and mosquitoes or other invertebrates such as snails that transmit the infectious agent by biting or depositing the infective material near the host. Vectors may be necessary to the life cycle of the organism (e.g., mosquitoes and malaria) or may act as mechanical transmitters (e.g., flies and food).
Disease Development
Exposure to an infectious agent does not always lead to an infection. Similarly, infection does not always lead to disease. Infection depends on the infective dose, the infectivity of the infectious agent and the immunocompetence of the host. It is important to differentiate infection and disease, as clearly illustrated by the HIV disease epidemic. Infection refers to the entry, development, and multiplication of the infectious agent in the susceptible host. Disease is one of the possible outcomes of infection and it may indicate a physiological dysfunction or pathological reaction. An individual who tests positive for HIV is infected, but if that person shows no clinical signs, the individual is not diseased. Similarly, if an individual tests positive for HIV and also exhibits clinical signs consistent with AIDS (HIV stage III), that individual is both infected and diseased.
Incubation period and communicable period are not synonymous. The incubation period is the time interval between invasion by an infectious agent and the first appearance of signs and symptoms of the disease. The incubation periods of infectious diseases vary from between 2 and 4 hours for staphylococcal food poisoning to between 10 and 15 years for AIDS (HIV stage III). The communicable period is the interval during which an infectious agent may be transferred directly or indirectly from an infected person to another person. The period of communicability for influenza is 3 to 5 days after the clinical onset of symptoms. Hepatitis B–infected persons are infectious many weeks before the onset of the first symptoms and remain infective during the acute phase and chronic carrier state, which may persist for life.
Disease Spectrum
Persons with infectious diseases may exhibit a broad spectrum of disease that ranges from subclinical infection to severe and fatal disease. Those with subclinical or inapparent infections are important from the public health point of view because they are a source of infection but may not be receiving care like those with clinical disease. They should be targeted for early diagnosis and treatment. Those with clinical disease may exhibit localized or systemic symptoms and mild to severe illness. The final outcome of a disease may be recovery, death, or something in between, including a carrier state, complications requiring extended hospital stay, or disability requiring rehabilitation.
At the community level, the disease may occur in endemic, epidemic, or pandemic proportion. Endemic refers to the constant presence of a disease within a geographic area or a population. Pertussis is endemic in the United States. Epidemic refers to the occurrence of disease in a community or region in excess of normal expectancy. Although people tend to associate large numbers with epidemics, even one case can be termed epidemic if the disease is considered previously eliminated from that area. For example, one case of polio, a disease considered eliminated from the United States, would be considered epidemic. Pandemic refers to an epidemic occurring worldwide and affecting large populations. HIV disease is both epidemic and pandemic, as the number of cases continues to grow across various regions of the world as well as in the United States. SARS and novel influenza A H1N1 are both emerging infectious diseases and responsible for recent pandemics.
Surveillance of Communicable Diseases
During the first half of the twentieth century, the weekly publication of national morbidity statistics by the U.S. Surgeon General’s Office was accompanied by the statement, “No health department, state or local, can effectively prevent or control disease without knowledge of when, where, and under what conditions cases are occurring” (CDC, 1996a, p 531). Surveillance gathers the “who, when, where, and what”; these elements are then used to answer “why.” A good surveillance system systematically collects, organizes, and analyzes current, accurate, and complete data for a defined disease condition. The resulting information is promptly released to those who need it for effective planning, implementation, and evaluation of disease prevention and control programs.
Elements of Surveillance
Infectious disease surveillance incorporates and analyzes data from a variety of sources. Box 13-2 lists 10 commonly used data elements.
Surveillance for Agents of Bioterrorism
Since September 11, 2001, increased emphasis has been placed on surveillance for any disease that might be associated with the intentional release of a biological agent. The concern is that, because of the interval between exposure and disease, a covert release may go unrecognized and without response for some time if the resulting outbreak closely resembles a naturally occurring one. Health care providers are asked to be alert to: (1) temporal or geographic clustering of illnesses (people who attended the same public gathering or visited the same location), especially those with clinical signs that resemble an infectious disease outbreak—previously healthy people with unexplained fever accompanied by sepsis, pneumonia, rash, or flaccid paralysis, and (2) an unusual age distribution for a common disease (e.g., chickenpox-like disease in adults without a child source case).
Because of the heightened concern about possible bioterrorist attacks, various sorts of syndromic surveillance systems have been developed by public health agencies across the country. These systems incorporate factors such as the previously mentioned temporal and geographic clustering and unusual age distributions with groups of disease symptoms or syndromes (e.g., flaccid paralysis, respiratory signs, skin rashes, gastrointestinal symptoms) with the goal of detecting early signs of diseases that could result from a bioterrorism-related attack. Syndromic surveillance systems may include tracking emergency department visits sorted by syndrome symptoms as well as other indicators of illness including school absenteeism and sales of selected over-the-counter medications. The CDC has developed EARS (Early Aberration Reporting System), a surveillance tool that is available at no charge and used by various public health officials across the country and abroad. Although more active infectious disease surveillance is being encouraged because of the potential for bioterrorism, the positive benefit is increased surveillance for other communicable diseases as well. Such heightened surveillance can just as easily warn of a community salmonellosis or influenza outbreak. Although the benefit of syndromic surveillance as a warning system has not been proved, it has been valuable in tracking disease outbreaks such as the 2009 H1N1 pandemic. (For additional information on preparedness surveillance and EARS, see the CDC website at http://www.bt.cdc.gov/episurv/.)
Nurses are frequently involved at different levels of the surveillance system. They play important roles in collecting data, making diagnoses, investigating and reporting cases, and providing information to the general public. Examples of possible activities include investigating sources and contacts in outbreaks of pertussis in school settings or shigellosis in day care; performing TB testing and contact tracing; collecting and reporting information pertaining to notifiable communicable diseases; performing infection control in hospitals; and providing morbidity and mortality statistics to those who request them, including the media, the public, service planners, and grant writers.
List of Reportable Diseases
“A notifiable disease is one for which regular, frequent, and timely information regarding individual cases is considered necessary for the prevention and control of the disease” (CDC, 2009c, p 2). Requirements for disease reporting in the United States are mandated by state rather than federal law and as such, vary slightly from state to state. State health departments, on a voluntary basis, report cases of selected diseases to the CDC through the National Notifiable Diseases Surveillance System (NNDSS). State public health officials collaborate with the CDC to determine which diseases should be nationally notifiable. The list of nationally notifiable diseases may be revised as new diseases emerge or disease incidence declines. The diseases designated as notifiable at the national level and reported in 2010 are listed in Box 13-3. The NNDSS data are collated and published weekly in the Morbidity and Mortality Weekly Report (MMWR). Final reports are published annually in the Summary of Notifiable Diseases. (Learn more about the NNDSS at the CDC website at http://www.cdc.gov/ncphi/disss/nndss/nndsshis.htm.)
Emerging Infectious Diseases
Emergence Factors
Emerging infectious diseases are those in which the incidence has actually increased in the past several decades or has the potential to increase in the near future. These emerging diseases may include new or known infectious diseases. Consider the following selected examples. Identified only in 1976 when sporadic outbreaks occurred in Sudan and Zaire, Ebola virus is a mysterious killer with a frightening mortality rate that sometimes reaches 90%, has no known treatment, and has no recognized reservoir in nature. It appears to be transmitted through direct contact with bodily secretions and as such can be contained once cases are identified. Why outbreaks occur is not understood, although index cases have been associated with the handling of wild primates. Evidence is also building for a bat reservoir. Ebola and its fellow virus Marburg are examples of new viruses that may appear as civilization intrudes farther and farther into previously uninhabited natural environments, changing the landscape and disturbing ecological balances that may have existed unaltered for hundreds of years. (Read more about the viral hemorrhagic viruses Ebola and Marburg at the CDC’s special pathogens website: http://www.cdc.gov/ncidod/dvrd/spb/index.htm.)
Hantavirus pulmonary syndrome was first detected in 1993 in the Four Corner area of Arizona and New Mexico, when young, previously healthy Native Americans fell ill with a mysterious and deadly respiratory disease. The illness was soon discovered to be a variant of, but to exhibit different pathology from, a rodent-borne virus previously known only in Europe and Asia. Transmission is thought to occur through aerosolization of rodent excrement. One explanation for the outbreak in the Southwest is that an unseasonably mild winter led to an unusual increase in the rodent population; more people than usual were exposed to a virus that had until that point gone unrecognized in this country. Infection in Native Americans first brought attention to hantavirus pulmonary syndrome because of a cluster of cases in a small geographic area, but no evidence suggests that any ethnic group is particularly susceptible to this disease. Hantavirus pulmonary syndrome has now been diagnosed in sites across the United States. The best protection against this virus seems to be avoiding rodent-infested environments.
Not only is HIV disease relatively new but the resultant immunocompromise gave rise to previously rare opportunistic infections such as cryptosporidiosis, toxoplasmosis, and Pneumocystis pneumonia (PCP). HIV may have existed in isolated parts of sub-Saharan Africa for years and emerged, only recently, into the rest of the world as the result of a combination of factors, including new roads, increased commerce, and prostitution. TB is a familiar face turned newly aggressive. After years of decline, it has resurged as a result of infection resulting from HIV disease and the development of multi-drug resistance. New influenza viruses like A H1N1 and A H5N1 challenge scientists to rapidly develop vaccines to protect a world population with little or no immunity.
WNV, a mosquito-borne seasonal disease, was first identified in Uganda in 1937 and first detected in the United States in 1999. How WNV arrived in the United States may never be known, but the answer most likely involves infected birds or mosquitoes. Because the virus was new in this country and the outbreak of 2002 caused numerous deaths, WNV garnered a great deal of media attention. However, for the majority of people, infection with WNV results in no clinical signs (about 80%) or only mild flu-like symptoms. In a small percentage of individuals, approximately 1 of 150 cases, a more severe, potentially fatal neuroinvasive form may develop, which may leave permanent neurological deficits for those who survive. The incidence of neuroinvasive disease increases with age with the highest rates in those 70 years and older. After first appearing in New York City in 1999, the virus spent several years quietly spreading up and down the East Coast without remarkable morbidity or mortality. This situation changed abruptly in the summer of 2002 when it began moving across the country, accompanied by significant avian, equine, and human mortality. WNV has now been reported in every state except Maine, Hawaii, and Alaska and is the most common arbovirus (virus carried by arthropods) disease in the country. The CDC estimates that during its introduction into the United States, between 1999 and 2008, WNV led to almost 30,000 confirmed and probable cases and over 1000 deaths. The number of reported cases varies widely per year. These periodic outbreaks appear to result from a complex interaction of multiple factors, including weather—hot, dry summers followed by rain, which influences mosquito breeding sites and population growth. Because the ecology of WNV is not fully understood, the future pattern and nature of the virus in the United States is uncertain. Until a human vaccine is developed (a vaccine for horses does exist), preventing human infection is dependent on mosquito control and preventing mosquito bites. Rarely, WNV has been transmitted through blood transfusions, in utero exposure, and possibly breastfeeding (CDC, 2010a). (Learn more about WNV and view maps of recent activity at the CDC website: http://www.cdc.gov/ncidod/dvbid/westnile/index.htm.)
Several factors, operating singly or in combination, can influence the emergence of these diseases (Table 13-1) (CDC, 1994). Except for microbial adaptation and changes made by the infectious agent, such as those likely in the emergence of E. coli 0157:H7, most of the emergence factors are consequences of activities and behavior of the human hosts, and of environmental changes such as deforestation, urbanization, and industrialization. The rise in households with two working parents has increased the number of children in day care and with this shift has come an increase in diarrheal diseases such as shigellosis. Changing sexual behavior and illegal drug use influence the spread of HIV disease as well as other sexually transmitted infections. Before the use of large air-conditioning systems with cooling towers, legionellosis was virtually unknown. Modern transportation systems closely and quickly connect regions of the world that for centuries had little contact. Insects and animals as well as humans may carry disease between continents on ships and planes. Immigrants, both legal and undocumented, as well as travelers bring with them a variety of known and potentially unknown diseases.
TABLE 13-1
FACTORS THAT CAN INFLUENCE THE EMERGENCE OF NEW INFECTIOUS DISEASES
| CATEGORIES | SPECIFIC EXAMPLES |
| Societal events | Economic impoverishment, war or civil conflict, population growth and migration, urban decay |
| Health care | New medical devices, organ or tissue transplantation, drugs causing immunosuppression, widespread use of antibiotics |
| Food production | Globalization of food supplies, changes in food processing and packaging |
| Human behavior | Sexual behavior, drug use, travel, diet, outdoor recreation, use of childcare facilities |
| Environmental | Deforestation/reforestation, changes in water ecosystems, flood/drought, famine, global changes (e.g., warming) |
| Public health | Curtailment or reduction in prevention programs, inadequate communicable disease infrastructure surveillance, lack of trained personnel (epidemiologists, laboratory scientists, vector and rodent control specialists) |
| Microbial adaptation | Changes in virulence and toxin production, development of drug resistance, microbes as co-factors in chronic diseases |
From Centers for Disease Control and Prevention: Addressing emerging infectious disease threats: a prevention strategy for the U.S., Atlanta, 1994, CDC.
To address the challenges of emerging and reemerging diseases, the CDC published Preventing Emerging Infectious Diseases: A Strategy for the 21st Century first in 1994 and then updated in 1998. This plan suggests that prevention and control of emerging diseases will require education to change behaviors and the development of effective drugs and vaccines. Also, current surveillance systems must be strengthened and expanded to improve detection and tracking (CDC, 1994, 1998a). Progress in addressing infectious disease as well as current findings and topics can be found in the CDC journal Emerging Infectious Diseases. (The journal is published monthly and is available online at http://www.cdc.gov/ncidod/EID/about/about.htm.)
Examples of Emerging Infectious Diseases
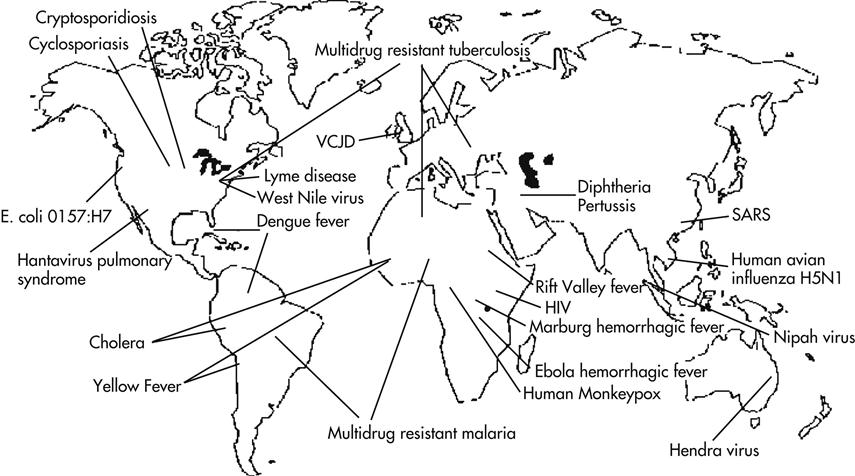
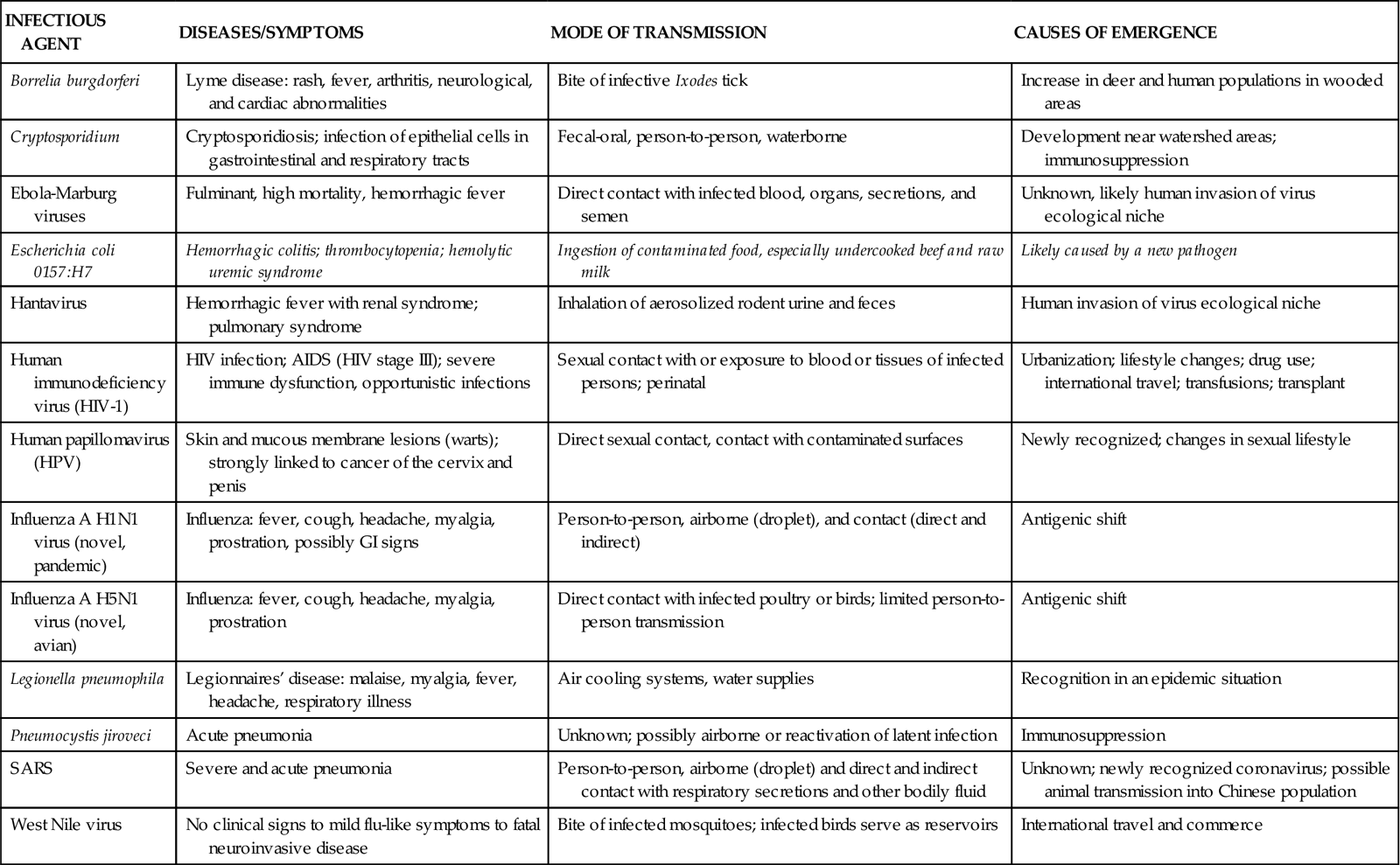
Examples of emerging and resurgent infectious diseases around the world are shown in Figure 13-2. Selected emerging infectious diseases, including a brief description of the diseases and symptoms they cause, their modes of transmission, and causes of emergence, are listed in Table 13-2.
TABLE 13-2
EXAMPLES OF EMERGING INFECTIOUS DISEASES
| INFECTIOUS AGENT | DISEASES/SYMPTOMS | MODE OF TRANSMISSION | CAUSES OF EMERGENCE |
| Borrelia burgdorferi | Lyme disease: rash, fever, arthritis, neurological, and cardiac abnormalities | Bite of infective Ixodes tick | Increase in deer and human populations in wooded areas |
| Cryptosporidium | Cryptosporidiosis; infection of epithelial cells in gastrointestinal and respiratory tracts | Fecal-oral, person-to-person, waterborne | Development near watershed areas; immunosuppression |
| Ebola-Marburg viruses | Fulminant, high mortality, hemorrhagic fever | Direct contact with infected blood, organs, secretions, and semen | Unknown, likely human invasion of virus ecological niche |
| Escherichia coli 0157:H7 | Hemorrhagic colitis; thrombocytopenia; hemolytic uremic syndrome | Ingestion of contaminated food, especially undercooked beef and raw milk | Likely caused by a new pathogen |
| Hantavirus | Hemorrhagic fever with renal syndrome; pulmonary syndrome | Inhalation of aerosolized rodent urine and feces | Human invasion of virus ecological niche |
| Human immunodeficiency virus (HIV-1) | HIV infection; AIDS (HIV stage III); severe immune dysfunction, opportunistic infections | Sexual contact with or exposure to blood or tissues of infected persons; perinatal | Urbanization; lifestyle changes; drug use; international travel; transfusions; transplant |
| Human papillomavirus (HPV) | Skin and mucous membrane lesions (warts); strongly linked to cancer of the cervix and penis | Direct sexual contact, contact with contaminated surfaces | Newly recognized; changes in sexual lifestyle |
| Influenza A H1N1 virus (novel, pandemic) | Influenza: fever, cough, headache, myalgia, prostration, possibly GI signs | Person-to-person, airborne (droplet), and contact (direct and indirect) | Antigenic shift |
| Influenza A H5N1 virus (novel, avian) | Influenza: fever, cough, headache, myalgia, prostration | Direct contact with infected poultry or birds; limited person-to-person transmission | Antigenic shift |
| Legionella pneumophila | Legionnaires’ disease: malaise, myalgia, fever, headache, respiratory illness | Air cooling systems, water supplies | Recognition in an epidemic situation |
| Pneumocystis jiroveci | Acute pneumonia | Unknown; possibly airborne or reactivation of latent infection | Immunosuppression |
| SARS | Severe and acute pneumonia | Person-to-person, airborne (droplet) and direct and indirect contact with respiratory secretions and other bodily fluid | Unknown; newly recognized coronavirus; possible animal transmission into Chinese population |
| West Nile virus | No clinical signs to mild flu-like symptoms to fatal neuroinvasive disease | Bite of infected mosquitoes; infected birds serve as reservoirs | International travel and commerce |
Based on information from Heymann DL, editor: Control of communicable diseases manual, ed 19, Washington, DC, 2008, American Public Health Association; Fauci AS, Touchette NA, Folkers GK: Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases, Emerg Infect Dis 11(4):519-525, 2005.
Prevention and Control of Communicable Diseases
Communicable disease can be prevented and controlled. The goal of prevention and control programs is to reduce the prevalence of a disease to a level at which it no longer poses a major public health problem. In some cases, diseases may even be eliminated or eradicated. The goal of elimination is to remove a disease from a large geographic area such as a country or region of the world. Eradication is removing a disease worldwide by ending all transmission of infection through the complete extermination of the infectious agent. WHO officially declared the global eradication of smallpox on May 8, 1980 (Evans, 1985). After the successful eradication of smallpox, the eradication of other communicable diseases became a realistic challenge, and in 1987 WHO adopted resolutions for eradication of paralytic poliomyelitis and dracunculiasis (guinea worm infection) from the world by the year 2000.
These eradication goals were not reached in 2000, but substantial progress has been made. When the resolution was made in 1987 for the eradication of Guinea worm disease, there were an estimated 3.5 million cases a year in 20 countries in Asia and Africa and 120 million people were at risk for the disease. By the end of 2007 the disease was endemic only in five countries in Africa and less than 10,000 cases were reported. Of the cases occurring during the first half of 2008, 98% were reported from Sudan, Ghana, and Mali. Sporadic violence appears to be the challenge to successful eradication of endemic dracunculiasis in this region of Africa (CDC, 2008a).
By 2010 the number of polio-endemic countries had decreased from 125 to 4 (Afghanistan, India, Nigeria, and Pakistan); 1256 cases of non–vaccine-derived or wild-type polio virus were reported from these four polio-endemic countries in 2009, compared with 350,000 cases reported from those 125 countries in 1988; another 350 imported cases from 10 non-endemic countries were also reported. Importation of cases resulting from the ease of worldwide travel or breakdowns in coverage in a neighboring country has led to outbreaks in non-endemic countries several times in the last 10 years, the largest being spillover into adjacent countries from Nigeria beginning in 2003 and cases in far-flung countries originating from exposure during the Muslim religious pilgrimage to Mecca. Such outbreaks point to the necessity of maintaining mass vaccination campaigns in polio-free countries to protect against cases imported from endemic areas. Challenges to eradication include political instability and sporadic violence, cultural beliefs about immunization, religious fears, and distrust of immunization (CDC, 2009d).
The Americas were certified polio free in 1994 (an outbreak in Haiti and the Dominican Republic in 2000 was vaccine derived), with the western Pacific certified in 2000 and Europe in 2002 (WHO, 2002). April 2005 marked the fiftieth anniversary of the polio vaccine. In 2004 WHO released an updated Global Polio Eradication Initiative Strategic Plan, outlining activities required to: (1) interrupt global polio transmission, (2) achieve global polio eradication certification, and (3) prepare for global cessation of childhood vaccination with the oral poliovirus vaccine (CDC, 2004). With the Global Polio Eradication Initiative, WHO partnered with national governments, Rotary International, the CDC and UNICEF in what has been called the largest public health initiative the world has ever known. Since 1988, over 2 billion children around the world have been immunized against polio through the cooperation of more than 200 countries and 20 million volunteers, supported by an international investment of over $3 billion. At the end of 2008, WHO reviewed the progress of the initiative with two independent outside agencies and concluded that the remaining technical and operational challenges to eradication could be overcome in each of the polio-endemic countries by ensuring the political commitment of all polio-affected countries to attain the highest possible coverage and enhancing routine vaccination and surveillance (CDC, 2009d). (Read more about global polio eradication efforts at http://www.polioeradication.org/.)
Primary, Secondary, and Tertiary Prevention
There are three levels of prevention in public health: primary, secondary, and tertiary. In prevention and control of infectious disease, primary prevention seeks to reduce the incidence of disease by preventing occurrence, and this effort is often assisted by the government. Many interventions at the primary level, such as federally supplied vaccines and “no shots, no school” immunization laws, are population based because of public health mandate. Nurses deliver childhood immunizations in public and community health settings, check immunization records in daycare facilities, and monitor immunization records in schools.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree