Chapter 6
ICD-9-CM Diagnosis and Procedure Coding
1. Define terms, phrases, abbreviations, and acronyms.
2. Demonstrate an understanding of the history and purpose of coding.
3. Discuss how ICD-9-CM data are used for research, education, and administrative purposes.
4. Provide an explanation of the relationship among documentation, medical necessity, claim forms, reimbursement, and coding.
5. Outline the content of ICD-9-CM Volumes I-III.
6. Demonstrate an understanding of ICD-9-CM coding conventions and guidelines.
7. Assign ICD-9-CM diagnosis and procedure codes to scenarios following the basic steps of coding.
Adverse reaction (adverse effect)
International Classification of Diseases (ICD)
International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)
International Classification of Diseases, 10th Revision (ICD-10)
International List of Causes of Death
American Health Information Management Association
Acquired immunodeficiency syndrome
Centers for Disease Control and Prevention
Commission on Professional and Hospital Activities
Centers for Medicare and Medicaid Services
Department of Health and Human Services
International Classification of Diseases
International Classification of Diseases, 7th Revision
International Classification of Diseases, 8th Revision
International Classification of Diseases, 9th Revision, Clinical Modification
International Classification of Diseases, 10th Revision
Medicare Severity-Diagnosis Related Groups
National Center for Health Statistics
Severe acute respiratory syndrome
Standard Nomenclature of Diseases and Operations
The objective of this chapter is to provide an overview of the history and purpose of coding medical conditions (diagnosis) and significant procedures using ICD-9-CM. A review of how coding relates to documentation, medical necessity, claim form submission, and reimbursement will demonstrate the importance of coding conditions and procedures in the hospital. The content of the ICD-9-CM coding manual is outlined to show how the coding system is organized. A discussion of ICD-9-CM coding conventions is important to understand how the conventions are used to communicate instructions to the coder. The chapter will close with a review of the basic steps of coding using ICD-9-CM diagnosis and procedure codes to provide an enhanced understanding of coding using this system. We will explore coding of diagnosis and procedures using the ICD-10, HCPCS Level I CPT and HCPCS Level II Medicare National coding systems in the next three chapters.
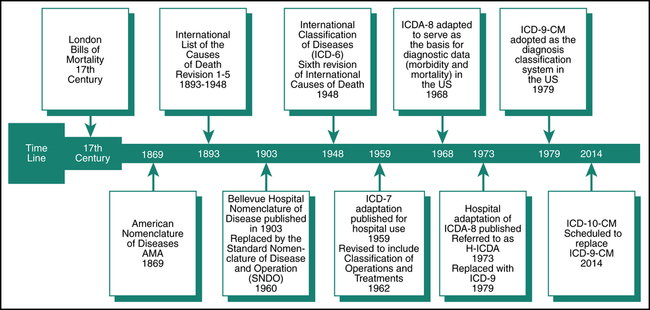
History of Diagnosis Coding
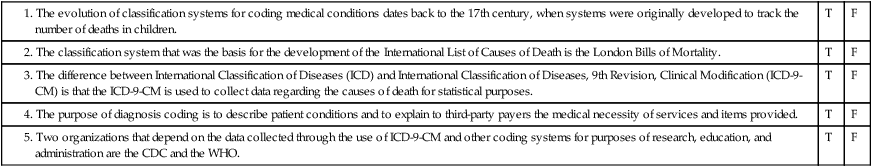
The evolution of classification systems for coding medical conditions dates back to the 17th century, when systems were originally developed to track the number of deaths in children. The classification and coding of medical conditions (diseases) began in England with the work of John Graunt. The London Bills of Mortality was developed by John Graunt in an attempt to estimate the proportion of live-born children who died before reaching the age of 6 years. As centuries passed, the attempts to classify causes of death and diseases continued. Many systems were developed, such as the International List of the Causes of Death, American Nomenclature of Diseases, International Classification of Diseases (ICD), Standard Nomenclature of Diseases and Operations (SNDO), and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). Figure 6-1 illustrates the evolution of diagnosis classification systems. Three major diagnosis classification systems that have been used over the years are the International List of the Causes of Death, the International Classification of Diseases (ICD), and the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). The ICD-9-CM is the standard coding system used today to code patient conditions and significant procedures. Legislation was passed that requires the replacement of ICD-9-CM with the International Classification of Diseases, 10th Revision (ICD-10) diagnosis and procedure coding system, effective October 1, 2014.
International Classification of Diseases (ICD)
The International Classification of Diseases (ICD) is a classification system that was used to collect data regarding the causes of death for statistical purposes. It was a revised version of the International List of the Causes of Death. The ICD was published by the World Health Organization (WHO). The Interim Commission of the WHO was given the responsibility for the sixth revision and also for the establishment of a list of causes of morbidity for international use. In 1948, WHO published ICD-6, which was a combined classification of causes of death (mortality) and disease (morbidity). With this publication came internationally accepted rules for selecting the underlying cause of death. The National Committee on Vital and Health Statistics (NCVHS) was established to serve as a liaison between national statistical institutions and WHO. From 1948 to today, there have been several revisions of the ICD. Information about WHO can be viewed on its Web site at http://www.who.int.
International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)
ICD-9-CM Coordination and Maintenance Committee
Maintenance and update of the ICD-9-CM is the result of a collaborative effort of members of the ICD-9-CM Coordination and Maintenance Committee. The committee consists of representatives from four organizations: the National Center for Health Statistics (NCHS), the Centers for Medicare and Medicaid Services (CMS), the American Hospital Association (AHA), and the American Health Information Management Association (AHIMA). The organizations are referred to as cooperating parties. Table 6-1 outlines the cooperating parties and responsibilities of each organization. Information regarding the ICD-9-CM Coordination and Maintenance Committee can be viewed on their Web site at http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm.
TABLE 6-1
ICD-9-CM Coordination and Maintenance Committee (Cooperating Parties)
| Organization | Responsibilities |
| National Center for Health Statistics (NCHS) | |
| Centers for Medicare and Medicaid Services (CMS) | |
| American Hospital Association (AHA) | |
| American Health Information Management Association (AHIMA) |
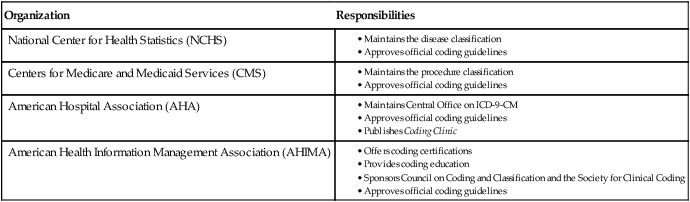
Data from Abdelhak M, Grostick S, Hanken MA, and associates (Eds): Health information: management of a strategic resource, ed 4, St Louis, 2012, Saunders.
International Classification of Diseases, 10th Revision (ICD-10)
The International Classification of Diseases, 10th Revision (ICD-10) is the standard code set for coding conditions and hospital procedures under HIPAA that is scheduled to replace ICD-9-CM effective October 1, 2014. ICD-10 was published in 1993 by the World Health Organization (WHO). The clinically modified version of ICD-10, referred to as ICD-10-CM, is the system that is scheduled to replace the ICD-9-CM Volume I and II for coding conditions. The ICD-10-PCS will replace ICD-9-CM Volume III procedure codes used for coding hospital significant procedures. The ICD-10 is currently used in many European countries. The United States has passed legislation requiring the implementation ICD-10. The Department of Health and Human Services released a final rule on January 16, 2009 mandating implementation of ICD-10 effective October 1, 2013. More recent legislation contains language that delays the compliance date to October 1, 2014. ICD-10 information can be viewed on the CDC Web site at http://www.cdc.gov/nchs/icd/icd10cm.htm.
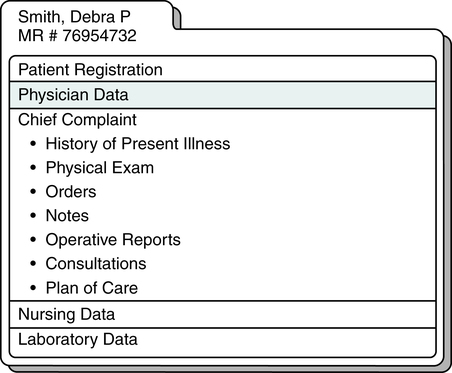
Purpose of Diagnosis Coding
The process begins when the patient arrives at the hospital with a health care issue(s) that requires attention or for a service involving health care status. Chief complaint is the term used to describe the main reason (medical condition or symptom) why the patient is seeking health care services. A clinical interview is conducted with the patient for the purpose of obtaining information regarding the patient’s chief complaint and the history of the present illness. Details about the chief complaint can include when the condition occurred, how bad the condition is, and if it gets worse during certain activities or at particular times. Information regarding other conditions that may relate to the main condition is also obtained. The physician or other provider reviews the history, performs an examination, and prepares a plan of care. The written descriptions of the patient’s signs, symptoms, conditions, illness, injury, disease, or other reason for the visit, as well as procedures, services, and items, are recorded in the patient’s medical record. The coder translates descriptions of medical conditions into diagnosis codes. Information in the patient’s medical record that is used for diagnosis coding is illustrated in Figure 6-2.
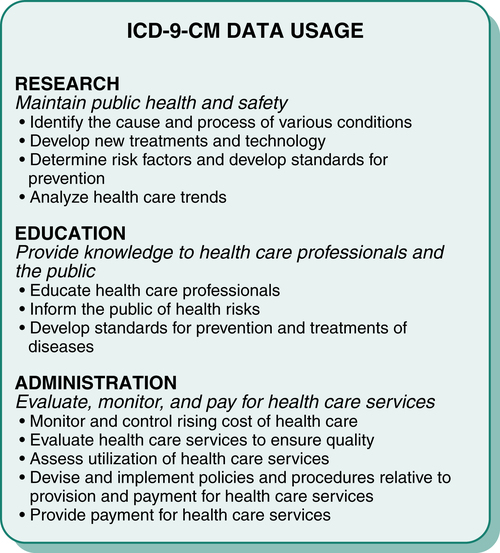
Diagnosis Code Data Usage
Data collected through the use of the ICD-9-CM coding system are used in a number of ways, as outlined in Figure 6-3. Various organizations and other entities such as government agencies, research organizations, medical associations, and insurance companies use ICD-9-CM data. Data collected are used for purposes such as research, education, and administration.
Organizations Using Diagnosis Code Data
The Centers for Disease Control and Prevention (CDC) is an agency of the U.S. government that provides facilities and services for the investigation, identification, prevention, and control of disease. The CDC is primarily concerned with communicable diseases, environmental health, and foreign quarantine activities. The CDC also works with state and local agencies, and it provides consultation, education, and training on communicable disease issues. For example, the CDC has established recommendations (standards) called “Universal Precautions” that specify how to minimize the risk of contracting communicable diseases such as acquired immunodeficiency syndrome (AIDS). The CDC uses ICD-9-CM coded data for many reasons, such as the identification of potential epidemics, including severe acute respiratory syndrome (SARS) or anthrax, and to predict trends regarding disease. Information regarding the CDC can be obtained from the Web site at http://www.cdc.gov/nchs/icd/icd9cm.htm.
The Centers for Medicare and Medicaid Services (CMS) is an agency within the Department of Health and Human Services that is responsible for the administration of Medicare and Medicaid programs. Data from ICD-9-CM are used by the CMS for many purposes, such as utilization and monitoring of health care costs and reimbursement. The government is one of the largest payers for health care services, and CMS is responsible for ensuring appropriate utilization of health care services and controlling health care costs. ICD-9-CM codes provide explanations for why services were provided. They are used by providers to communicate with payers regarding the medical necessity of services provided. CMS must also monitor health care costs for the Medicare and Medicaid programs to ensure that federal budgets are in balance. Reimbursement methods implemented under the Prospective Payment System (PPS) were developed using data from various coding systems. For example, Medicare Severity-Diagnosis Related Groups (MS-DRG) was developed through the classification of diseases, and payments are determined based on that classification. Information regarding CMS can be obtained from the Web site at http://www.cms.gov.
Diagnosis Coding Relationships
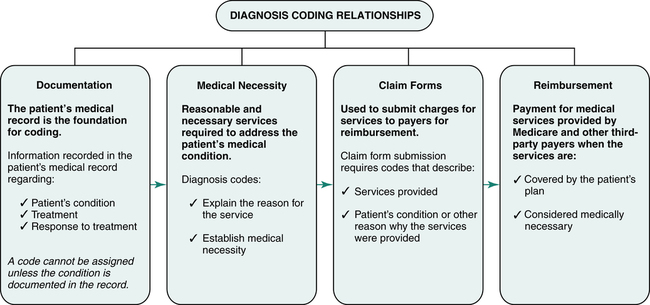
The ICD-9-CM is the standard coding system used by providers and facilities to describe a patient’s condition, injury, illness, disease, or other reasons the patient is receiving health care services. The coding of signs, symptoms, illness, injury, conditions, diseases, or other reasons that a patient seeks health care services requires knowledge of medical terminology, anatomy and physiology, pharmacology, and coding principles and guidelines. To code effectively, it is first important to have an understanding of how diagnosis coding relates to documentation, medical necessity, claim forms, and reimbursement (Figure 6-4).
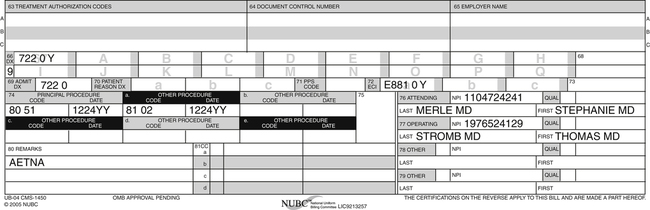
Claim Forms
The CMS-1500 and CMS-1450 (UB-04) are the two universal claim forms used for submission of charges to payers for reimbursement. The primary claim form used by hospitals is the CMS-1450 (UB-04); however, there may be circumstances when a CMS-1500 is required. The CMS-1450 (UB-04) contains 81 fields, referred to as form locators (FL). Codes that describe services provided are listed on the claim form. Diagnosis codes that explain the patient’s condition or other reason why the services were provided are also required on the claim form. Figure 6-5 illustrates CMS-1450 (UB-04) fields designated for reporting conditions and procedures using ICD-9-CM codes. The codes assigned for Mr. Jammes’s case in Example #2 are reported as follows: 722.0 “Displacement of cervical intervertebral disc” is reported in FL 67 and FL 69 since the herniated disc is the admitting and principal diagnosis. The external cause of injury code E881.00 “Fall on or from ladder” is reported in FL 72a. Diagnosis codes reported on the claim form may represent the principal diagnosis, other secondary diagnoses, admitting diagnosis, patient’s reason for visit diagnosis, or an external cause.
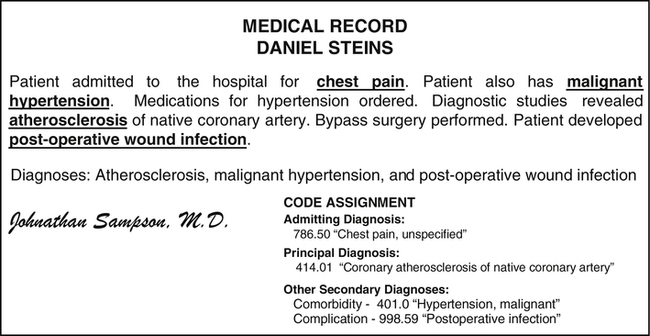
Principal Diagnosis
The principal diagnosis is the condition determined after study to be chiefly responsible for the admission. Study refers to the examination and other diagnostic testing used to determine the diagnosis. Figure 6-6 illustrates the principal diagnosis code assignment for the medical record of Daniel Steins. The patient presented with chest pain; however, the condition determined after study is atherosclerosis, and therefore 414.01 “Coronary atherosclerosis of native coronary artery” is recorded as the principal diagnosis in FL 67.
Other Secondary Diagnoses
A complication is a disease or condition that develops during the course of a hospital stay. Complications may prolong the patient’s length of stay, usually by 1 day in 75% of cases. Complications generally have an impact on the MS-DRG assignment. Figure 6-6 illustrates an example of a complication where the patient developed an infection of a surgical wound. Code 998.59 is assigned to describe the “Postoperative infection”. Codes that describe complications are recorded in FL 67A-Q. A comorbidity is a secondary condition that coexists with the condition for which the patient is seeking health care services. Comorbidities may prolong the patient’s length of stay, usually by 1 day in 75% of cases, which will have an impact on the MS-DRG assignment. An example of comorbidity is a patient presenting with atherosclerosis of an extremity who also has malignant hypertension. Malignant hypertension would be coded, 401.0, as the secondary diagnosis as illustrated in Figure 6-6. Codes that describe comorbidities are recorded in FL 67 A-Q.
Admitting Diagnosis
The admitting diagnosis is the major most significant reason why the patient is being admitted. For example, if a patient is admitted because he or she is experiencing chest pain and fatigue, the chest pain is the major most significant reason for the admission and therefore is the admitting diagnosis as illustrated in Figure 6-6. The admitting diagnosis is reported in FL 69.
Reimbursement
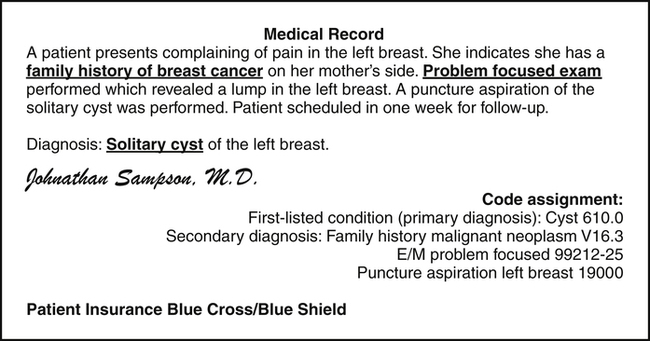
Reimbursement is the term used to describe payment from payers for services provided. Claim forms are submitted to third-party payers, such as insurance companies, Medicare, and other government payers, to obtain reimbursement for services provided. Diagnosis codes are used on the claim form to explain why the services were provided. They are also used to explain the medical necessity for the services. Payers provide reimbursement for services covered by the patient’s plan that are considered medically necessary based on standards of medical care. Therefore, it is critical to ensure that the codes submitted completely describe the patient’s medical condition(s) to establish medically necessity. Figure 6-7 highlights an example of a medical record that contains information required to establish medical necessity. The patient has a lump in her left breast and she has a family history of breast cancer. If the claim was submitted with a diagnosis of pain in the left breast, the payer might not consider the puncture aspiration medically necessary. The submission of diagnosis codes describing the lump and family history of breast cancer provides a clear explanation of why the aspiration was required.
ICD-9-CM Content
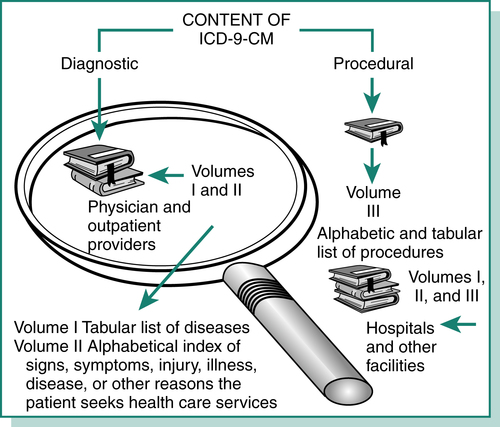
The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) consists of three sections referred to as Volumes. Volumes I and II are used to code descriptions of the patient’s signs, symptoms, injury, illness, disease, or other reason the patient is seeking health care services. Volume III is used to code descriptions of significant procedures performed during a hospital inpatient stay. Physician and outpatient providers use Volumes I and II. Hospitals and other facilities use Volumes I, II, and III of the ICD-9-CM to report patient conditions and significant procedures performed during the hospital visit. The ICD-9-CM can be purchased with Volume I and II only for physician and outpatient coding or with all three Volumes for use by hospitals and facilities (Figure 6-8).
ICD-9-CM Volume I Content
Volume I is the Tabular List of Diseases generally located in the middle of the ICD-9-CM coding manual. It is listed in the middle of the manual because the coder will reference Volume II, the alphabetic index, first to identify possible codes. Volume I is used to review codes identified in the index (Volume II) for selection of the code that most accurately describes the diagnostic statement in the record. Volume I contents include the Tabular List of Diseases, two supplemental classifications, and appendices, as outlined in Table 6-2.
TABLE 6-2
ICD-9-CM Volume I: Tabular List of Diseases
| CHAPTER | Heading | Range | |
| 1 | Infectious and Parasitic Diseases | 001–139 | |
| 2 | Neoplasms | 140–239 | |
| 3 | Endocrine, Nutritional, and Metabolic Diseases and Immunity Disorders | 240–279 | |
| 4 | Diseases of the Blood and Blood-Forming Organs | 280–289 | |
| 5 | Mental, Behavioral, and Neurodevelopment Disorders | 290–319 | |
| 6 | Diseases of the Nervous System and Sense Organs | 320–389 | |
| 7 | Diseases of the Circulatory System | 390–459 | |
| 8 | Diseases of the Respiratory System | 460–519 | |
| 9 | Diseases of the Digestive System | 520–579 | |
| 10 | Diseases of the Genitourinary System | 580–629 | |
| 11 | Complications of Pregnancy, Childbirth, and the Puerperium | 630–679 | |
| 12 | Diseases of the Skin and Subcutaneous Tissue | 680–709 | |
| 13 | Diseases of the Musculoskeletal System and Connective Tissue | 710–739 | |
| 14 | Congenital Anomalies | 740–759 | |
| 15 | Certain Conditions Originating in the Perinatal Period | 760–779 | |
| 16 | Symptoms, Signs, and Ill-Defined Conditions | 780–799 | |
| 17 | Injury and Poisoning | 800–999 | |
| Supplemental Classifications | |||
| 1. | Factors Influencing Health Status and Contact with Health Services | V01–V89 | |
| 2. | External Causes of Injury and Poisoning | E000–E999 | |
| Appendices∗ | |||
Classification of drugs by American Hospital Formulary Service List Number and their ICD-9-CM equivalents Classification of industrial accidents according to agency Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||