Chapter 4
Patient Accounts and Data Flow
1. Define terms, phrases, abbreviations, and acronyms.
2. Discuss the variations in patient accounts and data flow for outpatient, ambulatory surgery, and inpatient services.
3. Outline the patient care process and provide an explanation of each phase.
4. Identify the tasks performed during the admission process and discuss forms used during the process.
5. Provide an explanation of the insurance verification process.
6. Discuss the purpose of medical record documentation and various forms and documents used in the medical record.
7. Provide an overview of patient care services provided by a hospital and explain how charges are captured for the services.
8. State the role of Health Information Management (HIM) in billing patient care services.
9. Discuss phases of the hospital billing process and how it relates to accounts receivable (A/R) management.
Admission Evaluation Protocols (AEP)
Advance Beneficiary Notice (ABN)
Charge Description Master (CDM)
HIPAA Notice of Privacy Practices
Hospital-Issued Notice of Non-Coverage (HINN)
Informed consent for treatment
Medication Administration Record (MAR)
Medicare Secondary Payer (MSP) Questionnaire
Quality Improvement Organization (QIO)
Patient Accounts and Data Flow
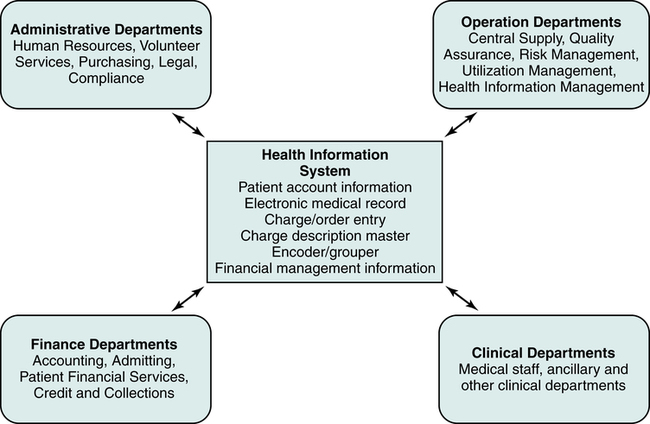
The flow of data begins when the patient reports to the hospital for patient care services. The patient’s demographic, insurance, and medical information is collected. Various administrative, financial, operational, and clinical departments use the data to perform functions required to provide efficient patient care services. The data is also used to prepare and submit charges for services rendered to patients, government, and other third-party payers. Clinical departments provide patient care services. Administrative and operational departments perform other critical functions such as human resource management, compliance, health information management, and utilization management. Financial departments are responsible for preparing charges for submission and accounts receivable management. The data flow in a hospital is designed to ensure that required data are accessible for personnel to perform various functions. Automation of the patient’s accounts, order entry, charge capture, billing, and accounts receivable allow greater access to patient information by various individuals within the hospital, as illustrated in Figure 4-1.
Outpatient
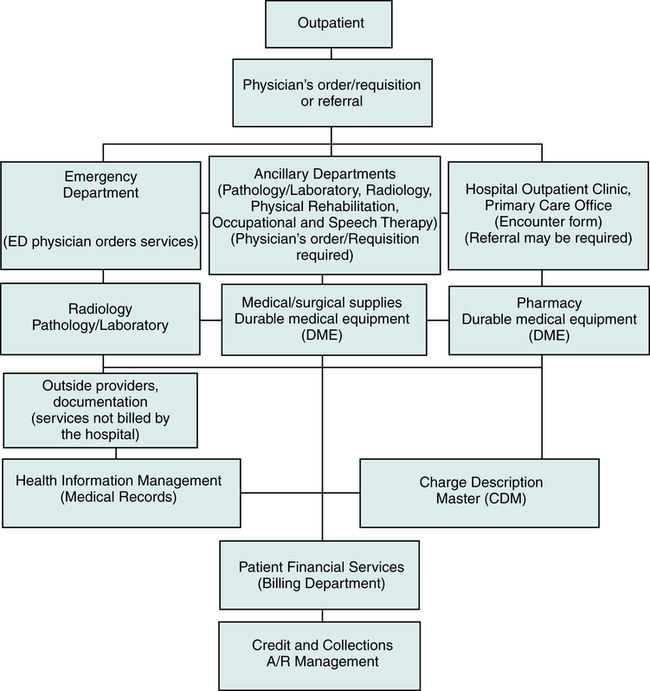
Outpatient services are those that are provided on the same day that the patient is released. The patient is received in various outpatient areas such as the Emergency Department (ED), clinic, primary care office, Ambulatory Surgery Center (ASC), or other ancillary departments, such as Laboratory or Radiology. The flow of data for outpatient services is illustrated in Figure 4-2. Admission tasks required to receive the patient are performed. Patient care services are rendered. Pharmaceuticals and other items such as supplies and equipment may be required. All patient care services are recorded in the medical record. Charges for hospital outpatient services are posted through the Charge Description Master (CDM), commonly referred to as the chargemaster. The Charge Description Master (CDM) is a computerized system used by the hospital to inventory and record services and items provided by the hospital. Charges for services provided in a clinic or primary care office are posted to the patient’s account. The patient is released and the services are billed to the patient or a third-party payer. Accounts are monitored for follow-up to ensure that payment is received in a timely manner.
Outpatient Data and Flow Variations
Clinic or Primary Care Office
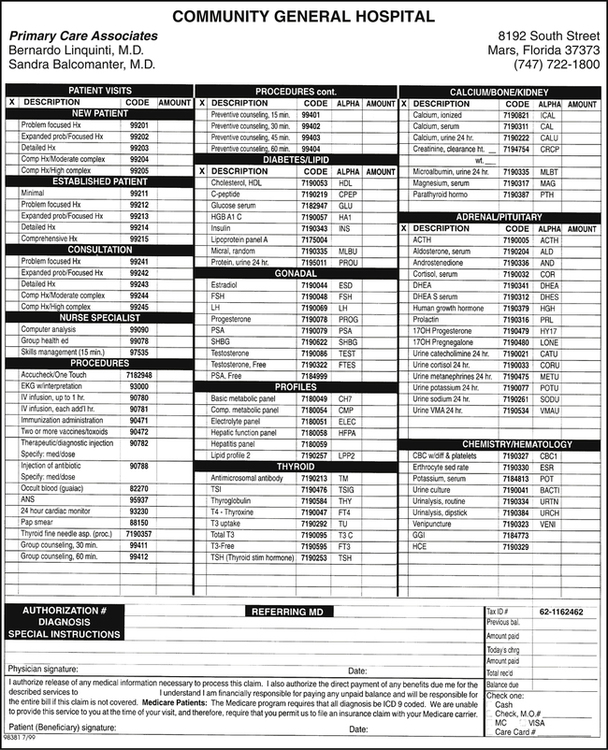
Hospital-based physician clinics or offices do not require a requisition when the patient presents for services. Hospital-based physician services are recorded in the patient’s medical record. An encounter form is used as a charge tracking document to record services, procedures, and items provided during the visit and the medical reason for the services provided (Figure 4-3). If services are required from other departments within the hospital, the clinic or primary care physician will prepare the required order or requisition.
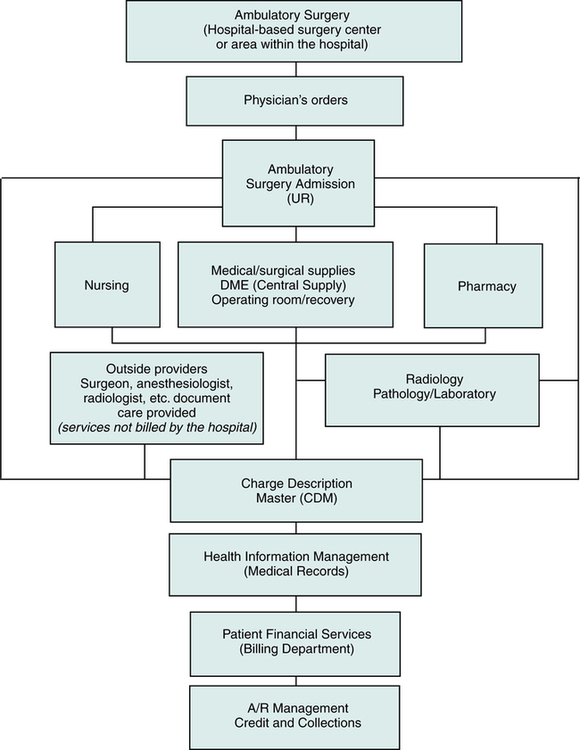
Ambulatory Surgery
Ambulatory surgery is a surgical procedure that is performed on a patient on the same day the patient is discharged to home. It is considered an outpatient service. Ambulatory surgeries can be performed in a hospital-based Ambulatory Surgery Center (ASC) or in a designated area within the hospital. Physician’s orders are prepared by the surgeon and submitted to the ambulatory surgery unit. The patient is received in the ambulatory surgery unit or the preadmission testing area. The appropriate clinical departments render patient care services. Pharmaceuticals, supplies, equipment, and other items may be required. All patient care services are recorded in the medical record. Services and the patient’s condition are assigned procedure and diagnosis codes. Hospital charges for services and items are posted through the chargemaster. The patient is discharged and the services are billed to the patient or a third-party payer. Accounts are monitored for follow-up to ensure that payment is collected in a timely manner. The flow of data for ambulatory surgery services is illustrated in Figure 4-4.
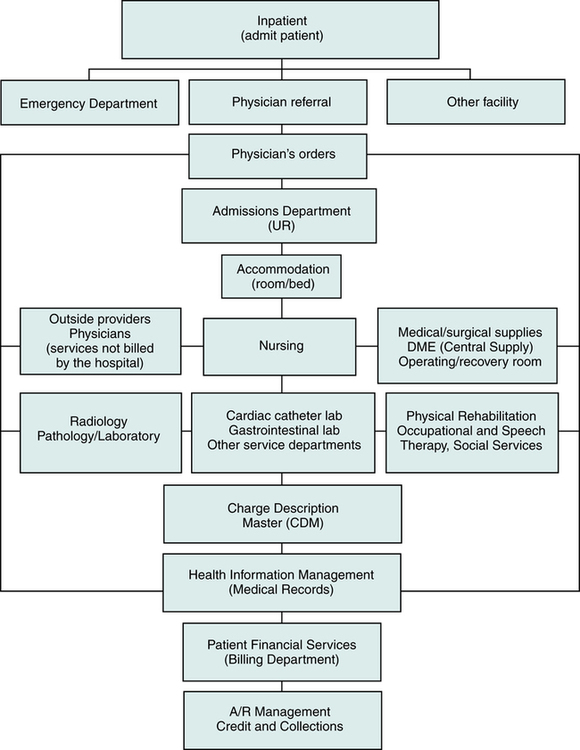
Inpatient
Physician’s orders are prepared by the admitting physician. The appropriate clinical departments render patient care services. Pharmaceuticals, supplies, equipment, and other items may be required. All patient care services are recorded in the medical record. Hospital charges for services and items are posted through the chargemaster. The patient is discharged and the services are billed to the patient or a third-party payer. Accounts are monitored for follow-up to ensure that payment is collected in a timely manner. The flow of data for inpatient services is illustrated in Figure 4-5.
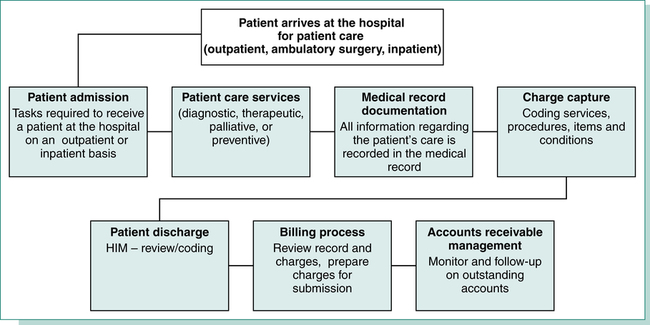
Patient Care Process
The patient care process is complex, as it involves many departments simultaneously performing various tasks related to patient care services. The process of providing patient care begins when a patient arrives at the hospital for care and continues until the patient is discharged. To provide effective and efficient patient care services and maintain financial stability, it is necessary to obtain all information required to evaluate and treat the patient and to bill for patient care services. All patient care activities must be recorded in the patient’s medical record to ensure that appropriate care is provided based on the patient’s condition. It is critical to capture all charges for submission to patients and third-party payers. Outstanding accounts must be monitored to obtain reimbursement in a timely manner. To achieve high standards of patient care and maintain financial stability, the hospital must have an efficient flow of information through the patient care process. Figure 4-6 illustrates the phases of the patient care process: patient admission, patient care services, medical record documentation, charge capture, coding, patient discharge, billing, and accounts receivable management.
Patient Admission
Utilization Review (UR)
• Federal and state licensing requirements
• Participating provider agreements with various payers and government programs
• Peer review organizations, such as the QIO, have the authority to deny payment for services that do not meet stated requirements
• Services are medically necessary as defined in participating provider agreements.
• The level of service for provision of health care is appropriate according to the patient’s condition.
• Quality patient care services are provided in accordance with standards of medical care.