Chapter 7
ICD-10-CM Diagnosis Coding
1. Define terms, phrases, abbreviations, and acronyms.
2. Provide a brief overview of the evolution of diagnosis coding to ICD-10-CM.
3. Discuss the impact ICD-10 on documentation, coding, medical necessity, claim forms, and reimbursement.
4. Identify three key areas of ICD-10-CM data usage and discuss organizations that use ICD-10-CM data.
5. Demonstrate an understanding of various aspects of the ICD-10-CM transition, including certification, mapping and crosswalks, and the ICD-10-CM Coordination and Maintenance Committee.
6. State key differences between ICD-10-CM and ICD-9-CM.
7. Provide an outline of ICD-10-CM manual content and explain the use of each section.
8. Identify coding conventions and apply coding principals related to conventions and coding.
9. Demonstrate an understanding of the steps to coding using the ICD-10-CM diagnosis coding system.
Adverse reaction (adverse effect)
International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)
International Classification of Diseases, 10th Revision (ICD-10)
International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM)
International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS)
International List of Causes of Death
American Academy of Professional Coders
American Health Information Management Association
Acquired immune deficiency syndrome
American National Standards Institute
Centers for Disease Control and Prevention
Clinical documentation improvement
Centers for Medicare and Medicaid Services
Department of Health and Human Services
Health Insurance Portability and Accountability Act
International Classification of Diseases
International Classification of Diseases, 9th Revision, Clinical Modification
International Classification of Diseases, 10th Revision
International Classification of Diseases, 10th Revision, Clinical Modification
International Classification of Diseases, 10th Revision, Procedure Coding System
Inpatient Prospective Payment System
Medicare Severity-Diagnosis Related Groups
National Center for Health Statistics
Severe acute respiratory syndrome
Hospital coding and billing professionals will be required to have an understanding of the ICD-9-CM coding system and will need to transition to ICD-10. In an effort to provide current and future knowledge required for hospital professionals, this text presents concepts on coding using ICD-9-CM and ICD-10. The previous chapter presented concepts on coding medical conditions and significant procedures using ICD-9-CM. This chapter will focus on coding medical conditions using the ICD-10-CM coding system.
Evolution of Diagnosis Coding
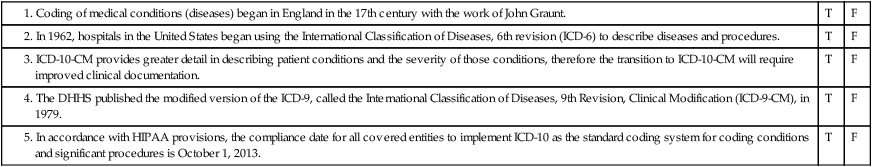
As discussed in the prior chapter, the evolution of classification systems for coding medical conditions dates back to the 17th century, when systems were originally developed to track the number of deaths in children. Coding of medical conditions (diseases) began in England in the 17th century with the work of John Graunt. John Graunt developed the London Bills of Mortality in an attempt to estimate the proportion of live-born children who died before reaching the age of 6 years. As centuries passed, the attempts to classify causes of death and diseases continued. The International List of the Causes of Death was developed based on the London Bills of Mortality. I was presented at the International Statistical Institute and was adopted in 1893. Several countries adopted the International List of the Causes of Death during the 19th century. Six revisions were made to the International List of the Causes of Death through 1948, and the sixth revision included a name change to the International Classification of Diseases (ICD). The Interim Commission of the World Health Organization (WHO) was given the responsibility for the sixth revision and also for the establishment of a list of causes of morbidity for international use. Information about the World Health Organization (WHO) can be viewed on its Web site at http://www.who.int/en/.
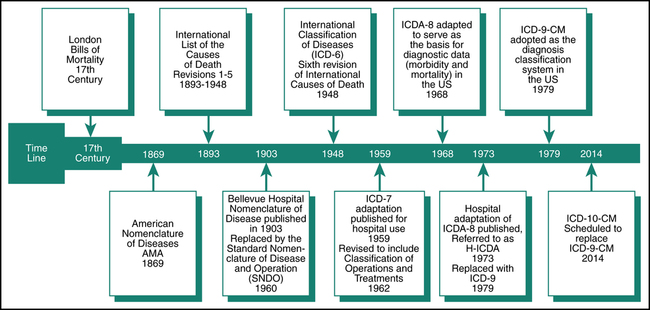
The International Classification of Diseases (ICD) underwent revisions 1-9 as the quest continued to develop a uniform system to classify disease that could be adopted worldwide. The ideal system would statistically capture detailed information regarding morbidity and mortality that could be adopted internationally. Figure 7-1 illustrates the evolution of diagnosis coding systems to ICD-10-CM.
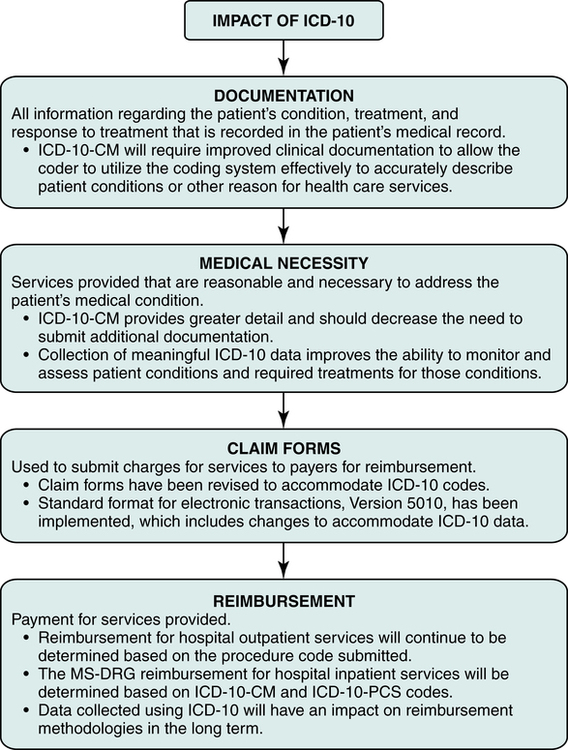
Impact of ICD-10
The implementation of the ICD-10 coding systems will impact all aspects of the health care industry from technology to health care policy. ICD-10 has been adopted in many countries and will be adopted in the United States. ICD-10 will provide meaningful health care data that accurately reflects conditions and treatments seen in today’s medical practice, and the data can be used worldwide. ICD-10-CM provides greater detail in describing patient conditions and the severity of those conditions. The terminology and disease information is updated. Combination codes that describe symptom, manifestations, and diagnosis are included. Details regarding injuries have been expanded. ICD-10-CM also includes expanded information on health care encounters for reasons other than disease as well as information relevant to ambulatory and managed care encounters. The level of detail in ICD-10-CM will promote quality coding, which is necessary to ensure that accurate and reliable data is gathered for budgeting, clinical research, credentialing, peer review, education, financial analysis, marketing, patient care, quality assurance, risk management, strategic planning, utilization management, and other internal or external facility purposes. It is important for hospital coding and billing professionals to understand the impact of ICD-10 on documentation, medical necessity, claim forms, and reimbursement (Figure 7-2).
Documentation
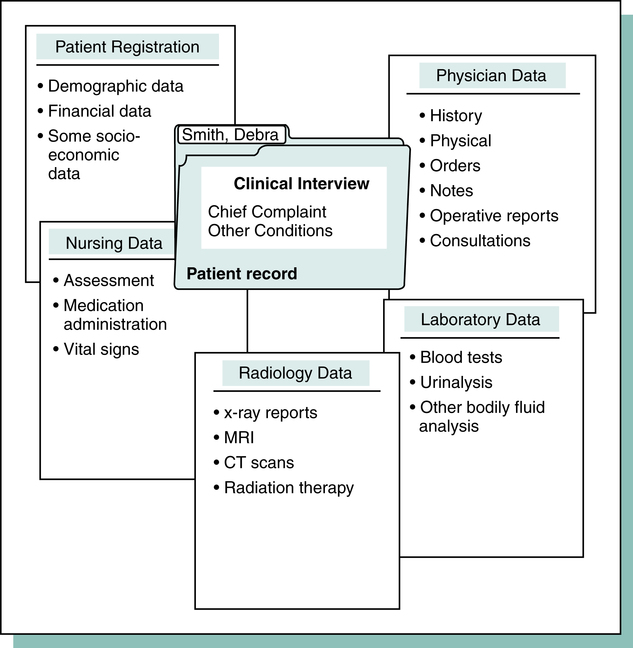
Coding is the process of translating written descriptions of procedures, services, items, and patient conditions into numeric or alphanumeric codes. It involves the assignment of numeric or alphanumeric codes to all health care data elements of inpatient and outpatient care. Documentation is the term used to describe information recorded in the medical record regarding the patient’s condition, treatment, and response to treatment as illustrated in Figure 7-3. Information contained in the patient’s medical record is used to assign diagnosis and procedure codes that are submitted on a claim form. Diagnosis coding is the process of translating written descriptions of signs, symptoms, illness, injury, disease, and other reasons for health care services that are documented in the patient’s medical record into codes. Diagnosis coding is essential to explain why the patient is receiving health care services.
• Ambulatory and managed care encounter information such as the designation of encounters for fracture care as initial, subsequent, or sequela. Fracture care also requires information regarding healing of the fracture, including delayed, failure to heal, malunion, or non-union.
• Expanded injury codes including designations for encounters.
• Combination codes that describe the diagnosis and symptom or manifestation such as heart disease with angina or diabetes with retinopathy. Poisoning and adverse effect codes include the external cause of injury.
• Left and right designations are included within the codes ranges; right side is “1,” left side is “2,” and bilateral is “3.”
• Higher level of detail to explain the condition and the severity, such as heart failure codes that require documentation of the type of failure: systolic, diastolic, acute, and/or chronic or ulcer codes that require indication of staging. Fracture coding requires documentation of the type of fracture such as greenstick or spiral; open or closed; displaced or non-displaced; right or left; and the episode of care. In addition, fracture coding requires specification of the exact bone and the exact location within the bone.
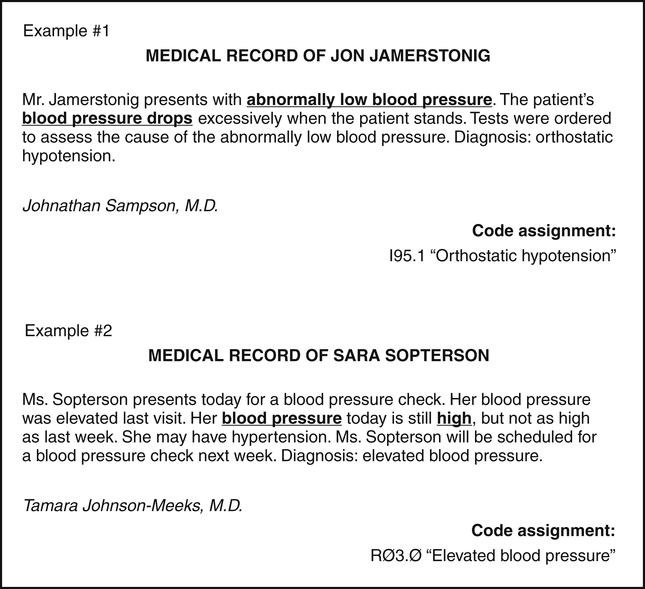
When coding medical conditions, it is necessary to read the record to identify the condition(s) that is being treated and the condition(s) that can affect treatment. A code(s) is then selected from the ICD-10-CM that accurately describes the statement in the medical record. Examples of information recorded in the patient’s medical record and the code assignments are illustrated in Figure 7-4. The challenge for coders is to be absolutely certain the code assignment represents what is in the record. The coder must follow the Golden Rule of coding: IF IT IS NOT DOCUMENTED, DO NOT CODE IT. It is important that the coder does not read into the scenario and code a condition that is not supported by the documentation. If the record lacks specific information required to select a code, the coder should pursue more specific information from the physician or other provider. Most hospitals have a physician query process for coders to clarify information.
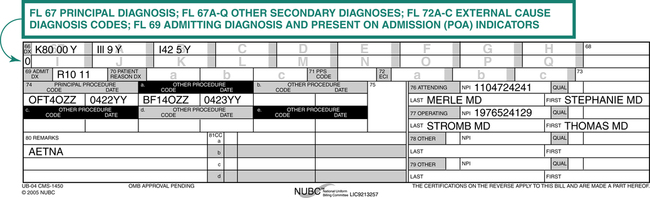
Claim Forms
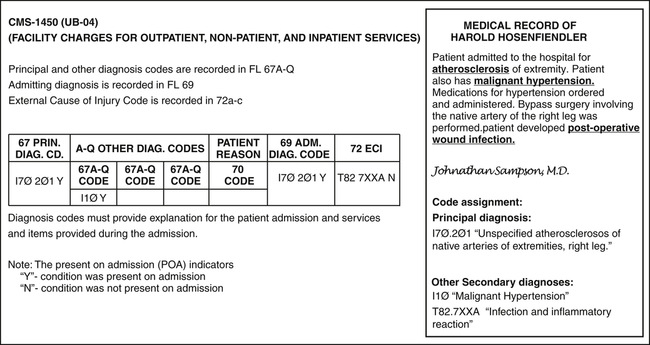
Claim forms are used to submit charges for services rendered to payers for reimbursement. The CMS-1450 (UB-04) is the claim form primarily used to submit hospital services. There may be a situation where a payer requires the CMS-1500 for specified services. Codes that describe services and diagnoses are listed on the claim form. As illustrated on the CMS-1450 (UB-04), diagnosis codes explain the patient’s condition or other reason why the services were provided (Figure 7-5).
Principal Diagnosis
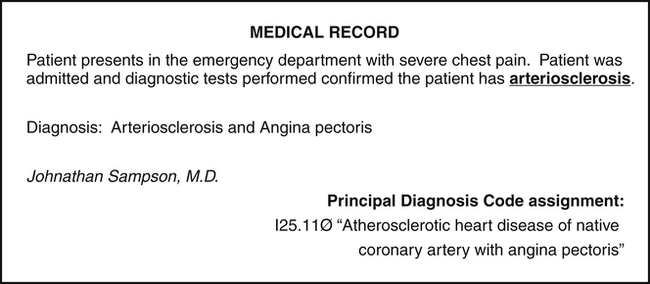
The principal diagnosis is the condition determined after study to be chiefly responsible for admission of the patient to the hospital for care. Study refers to the examination and other diagnostic testing used to determine the diagnosis. For example, a patient is admitted to the hospital for chest pain. After diagnostic tests are performed, the physician records a diagnosis of arteriosclerosis. The principal diagnosis is the condition determined after study, therefore a code is assigned for arteriosclerosis (Figure 7-6). If the physician does not document a definitive diagnosis, then the principal diagnosis would be the same as the admitting diagnosis. This record provides an example of combination codes found in ICD-10. One code is assigned to explain the atherosclerotic heart disease and the symptom, angina pectoris.
Other Secondary Diagnoses
Complication
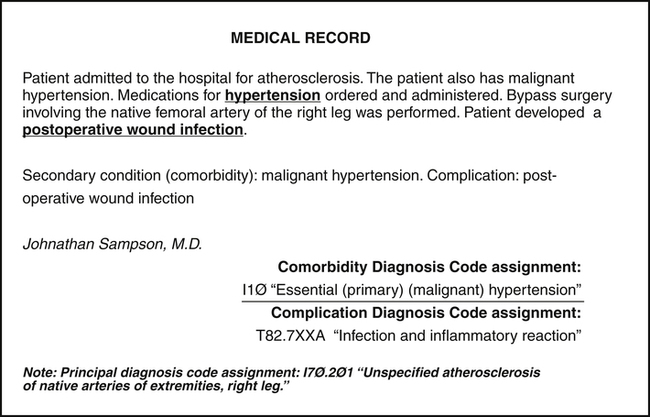
A complication is a disease or condition that develops during the course of a hospital stay. Complications may prolong the patient’s length of stay, usually by 1 day in 75% of cases. Complications generally have an impact on the MS-DRG assignment. A postoperative infection is an example of a complication, since the surgical wound became infected. A code(s) is assigned to describe complications as illustrated in Figure 7-7.
Comorbidity
Comorbidity is a secondary condition that coexists with the condition for which the patient is seeking health care services. Comorbidities may also prolong the patient’s length of stay and therefore can affect the MS-DRG assignment. An example of comorbidity is a patient presenting with atherosclerosis of an extremity who also has malignant hypertension. Malignant hypertension would be coded as the secondary diagnosis (see Figure 7-7).
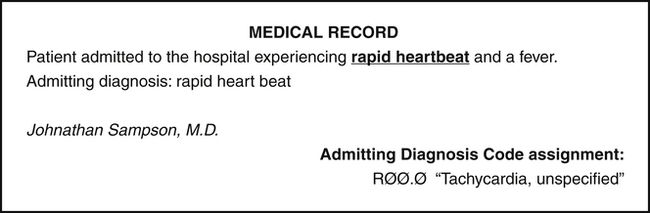
Admitting Diagnosis
The admitting diagnosis is the major most significant reason why the patient is being admitted for an inpatient stay. For example, a patient presents with a chief complaint of rapid heartbeat and fever. The attending physician decides to admit the patient after reviewing results from diagnostic tests. The admitting diagnosis would be rapid heartbeat (tachycardia) because it is the major most significant reason for the admission (Figure 7-8).
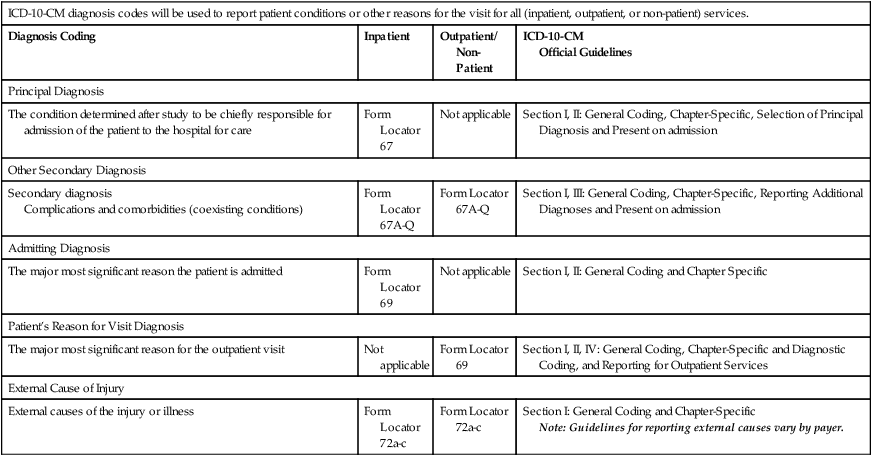
Reporting Diagnoses – CMS-1450 (UB-04)
It is important for coders to understand what diagnosis is required for the claim form, where the diagnosis code is recorded, and what coding guidelines apply to the patient case, as illustrated in Table 7-1. ICD-10-CM implementation has not changed the reporting requirements for diagnoses on the CMS-1450 (UB-04). The form is used to submit facility charges for outpatient, non-patient, and inpatient services provided by a hospital or other facility. The CMS-1450 (UB-04) contains 81 fields referred to as form locators (FL). The CMS-1450 (UB-04) claim form completion requirements include the reporting of all patient diagnoses to explain the medical reason for the admission and services provided. Figure 7-9 illustrates how ICD-10-CM diagnosis code(s) are recorded on the CMS-1450 (UB-04).
TABLE 7-1
Claim Variations for ICD-10-CM Diagnosis Codes
| ICD-10-CM diagnosis codes will be used to report patient conditions or other reasons for the visit for all (inpatient, outpatient, or non-patient) services. | |||
| Diagnosis Coding | Inpatient | Outpatient/ Non-Patient | ICD-10-CM Official Guidelines |
| Principal Diagnosis | |||
| The condition determined after study to be chiefly responsible for admission of the patient to the hospital for care | Form Locator 67 | Not applicable | Section I, II: General Coding, Chapter-Specific, Selection of Principal Diagnosis and Present on admission |
| Other Secondary Diagnosis | |||
| Secondary diagnosis Complications and comorbidities (coexisting conditions) | Form Locator 67A-Q | Form Locator 67A-Q | Section I, III: General Coding, Chapter-Specific, Reporting Additional Diagnoses and Present on admission |
| Admitting Diagnosis | |||
| The major most significant reason the patient is admitted | Form Locator 69 | Not applicable | Section I, II: General Coding and Chapter Specific |
| Patient’s Reason for Visit Diagnosis | |||
| The major most significant reason for the outpatient visit | Not applicable | Form Locator 69 | Section I, II, IV: General Coding, Chapter-Specific and Diagnostic Coding, and Reporting for Outpatient Services |
| External Cause of Injury | |||
| External causes of the injury or illness | Form Locator 72a-c | Form Locator 72a-c | Section I: General Coding and Chapter-Specific Note: Guidelines for reporting external causes vary by payer. |
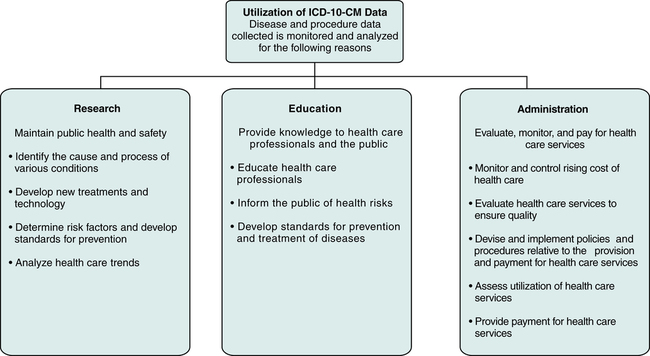
ICD-10-CM Data Usage
Data collected through the use of the ICD-10-CM coding system will be used in a number of ways, as outlined in Figure 7-10. Various organizations and other entities, such as government agencies, research organizations, medical associations, and insurance companies, use data collected for purposes such as research, education, and administration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree