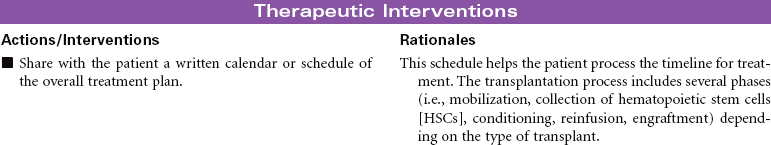
Chapter 10 Bone Marrow Transplant; Peripheral Blood Stem Cell Transplant There are three major types of transplants: • Syngeneic: Donor from an identical twin • Allogeneic: Can be related (from a matched sibling) or unrelated (from a volunteer in the Be The Match Registry). This is also referred to as a matched unrelated donor (MUD) transplant. There are three sources of hematopoietic stem cells: • Peripheral blood: The stem cells that normally reside in the bone marrow can be moved or mobilized into the bloodstream (peripheral circulation) and collected in an outpatient procedure via a cell separator or apheresis machine. This procedure does not require anesthesia. The majority of all transplants performed today use peripheral blood stem cells rather than bone marrow stem cells. • Bone marrow: These cells are collected from the pelvic bones through a series of aspirations. Bone marrow harvesting is a surgical procedure done under general anesthesia. • Umbilical cord, placental: This is a rich source of stem cells that are collected at the time of delivery from tissue that is normally discarded.
Hematolymphatic, Immunological, and Oncological Care Plans
![]() For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
Hematopoietic Stem Cell Transplantation
Hematolymphatic, Immunological, and Oncological Care Plans
Get Clinical Tree app for offline access

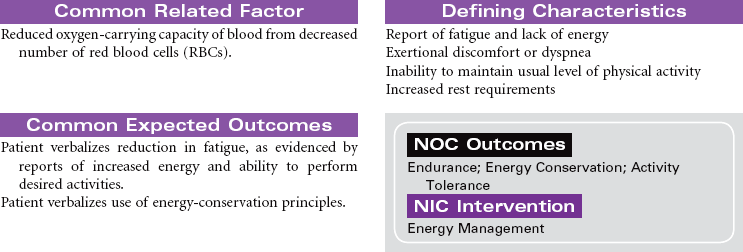
 = Independent
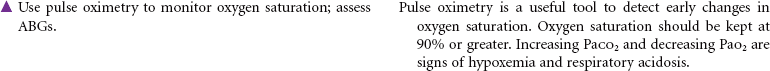
= Independent  = Collaborative
= Collaborative