Geriatric Pharmacology
Objectives
• Explain the physiologic changes of the aging process that have a major effect on drug therapy.
• Explain the pharmacokinetics and pharmacodynamics of the older adult that relate to drug dosing.
• Differentiate the effects of two drug categories on the older adult.
• Discuss reasons for noncompliance to drug regimen by the older adult.
• Describe nursing implications related to drug therapy in the older adult.
Key Terms
adherence, p. 94
nonadherence, p. 93
older adult, p. 88
polypharmacy, p. 89
In coming years, nurses will care for increasing numbers of older adults, who will represent the “core business” of health care. Geriatric pharmacology for the older adult requires special attention to the age-related factors of drug absorption, distribution, metabolism, and excretion. Drug dosages are adjusted according to the older adult’s weight, adipose tissue, laboratory results (e.g., serum protein, electrolytes, liver enzymes, blood urea nitrogen [BUN], creatinine clearance), and current health problems. Modifications in drug therapy for the older adult are frequently required. Because of declining organ functioning in older adults, the effects of drug therapy must be closely monitored to prevent adverse reactions to drugs and possible drug toxicity.
Approximately 85% of adults older than 65 years take medications. By 2030, it is expected that the number of older adults will be nearly twice the number in 2000. Women 65 years old presently outnumber men of that age by 134 to 100; in the 75-year-old age group, there are 100 women to 55 men. A fast-growing population is those age 85 years and older, and their use of drug therapy will likely continue to grow.
Older adults take pain, sleep, and laxative over-the-counter (OTC) drugs more frequently than younger populations. At the time of hospital admission, only about 15% of patients older than 65 years are not taking any medications (prescribed or self-medicated). During hospitalization, older adults take an average of three to five drugs. In nursing homes, 33% of patients receive 6 to 12 drugs daily.
The adverse reactions and drug interactions that occur in the older adult are three to seven times greater than those for middle-aged and young adults. Older adults consume numerous drugs because of chronic and multiple illnesses; therefore, they are susceptible to adverse reactions and interactions. Additional problems that can cause adverse reactions from drugs include self-medicating with OTC drugs, taking drugs prescribed for other health problems, taking drugs ordered by several different health care providers, overdosing when symptoms do not subside, taking new drugs to treat the side effects of other drugs, using drugs that were prescribed for another person, and, of course, the ongoing physiologic aging process. Intentional noncompliance (possibly related to drug costs or side effects) and unintentional noncompliance (possibly related to complicated, confusing drug regimens or impaired mental status) must be assessed, as should alcohol use or abuse and its interactions with medications.
Drug toxicity may develop in the older adult for drug doses that are within the therapeutic range for the younger adult. These therapeutic drug ranges are usually safe for young and middle-aged adults but are not always within safe range for older adults. It has been suggested that the drug dose for older adults should initially be prescribed at a low to low-average therapeutic range and then gradually increased according to tolerance and lack of adverse reactions; start low and go slow is an important concept. This approach prevents a toxic reaction to the drug in older adults. Older adults who are at risk for problems with medication administration frequently have common characteristics such as lack of coordinated care, recent discharge from the hospital, self-treatment, multiple diagnoses, sensory and physical changes associated with aging, multiple health care providers, and cognitive impairment.
Physiologic Changes
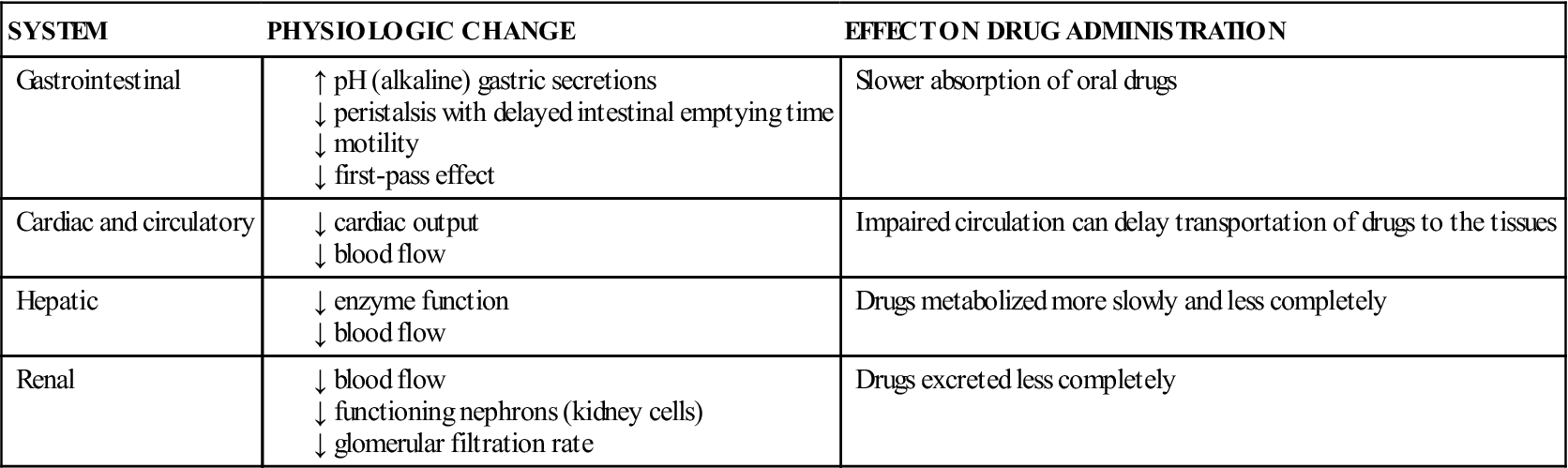
The physiologic changes associated with the aging process have a major effect on drug therapy. Table 8-1 describes the physiologic changes that occur in the gastrointestinal (GI), cardiac and circulatory, hepatic, and renal systems of the older adult and how these changes can affect pharmacologic response to drug therapy.
TABLE 8-1
PHYSIOLOGIC CHANGES IN THE OLDER ADULT
Polypharmacy
Polypharmacy (administration of many drugs together) is more common in older adults because of the use of (1) multiple health care providers, (2) herbal therapy, (3) OTC drugs, and (4) discontinued prescription drugs. Polypharmacy can cause confusion, falls, malnutrition, renal and liver dysfunction, and nonadherence. The nurse should coordinate the health care of older adults, including drug therapy, to avoid duplication of drugs from various health care providers and misuse of OTC and herbal supplements. For example, an older patient may take a prescribed drug, ranitidine (Zantac), with an OTC drug, famotidine (Pepcid AC), for GI discomfort; this drug combination causes duplication to occur. Some older adults do not think herbal drugs are actually drugs that could cause adverse reactions when taken with other prescription or OTC drugs. Older adults should be encouraged to use one pharmacy and give the pharmacist a list of all drugs they take, both prescribed and OTC. Pharmacists conduct clinical reviews of medications that focus primarily on drug interactions.
Pharmacokinetics
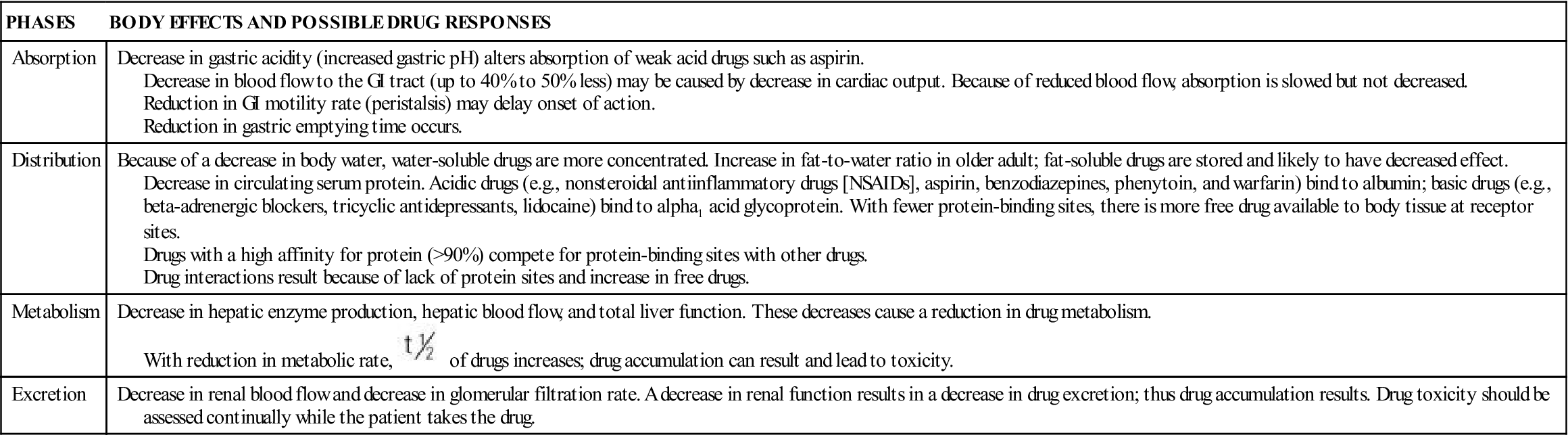
Parameters of pharmacokinetics for the older adult are described in Table 8-2.
TABLE 8-2
PHARMACOKINETICS IN GERIATRIC PHARMACOLOGY
| PHASES | BODY EFFECTS AND POSSIBLE DRUG RESPONSES |
| Absorption | Decrease in gastric acidity (increased gastric pH) alters absorption of weak acid drugs such as aspirin. Decrease in blood flow to the GI tract (up to 40% to 50% less) may be caused by decrease in cardiac output. Because of reduced blood flow, absorption is slowed but not decreased. Reduction in GI motility rate (peristalsis) may delay onset of action. Reduction in gastric emptying time occurs. |
| Distribution | Because of a decrease in body water, water-soluble drugs are more concentrated. Increase in fat-to-water ratio in older adult; fat-soluble drugs are stored and likely to have decreased effect. Decrease in circulating serum protein. Acidic drugs (e.g., nonsteroidal antiinflammatory drugs [NSAIDs], aspirin, benzodiazepines, phenytoin, and warfarin) bind to albumin; basic drugs (e.g., beta-adrenergic blockers, tricyclic antidepressants, lidocaine) bind to alpha1 acid glycoprotein. With fewer protein-binding sites, there is more free drug available to body tissue at receptor sites. Drugs with a high affinity for protein (>90%) compete for protein-binding sites with other drugs. Drug interactions result because of lack of protein sites and increase in free drugs. |
| Metabolism | Decrease in hepatic enzyme production, hepatic blood flow, and total liver function. These decreases cause a reduction in drug metabolism. With reduction in metabolic rate,  of drugs increases; drug accumulation can result and lead to toxicity. of drugs increases; drug accumulation can result and lead to toxicity. |
| Excretion | Decrease in renal blood flow and decrease in glomerular filtration rate. A decrease in renal function results in a decrease in drug excretion; thus drug accumulation results. Drug toxicity should be assessed continually while the patient takes the drug. |
Absorption
Drug absorption from the GI tract is slowed in the older adult because of decreases in both blood flow and GI motility. In this age group, acidic drugs are poorly absorbed because of increased alkaline gastric secretions, but enteric-coated tablets dissolved in alkaline fluid can break down more rapidly. Drugs remain in the GI tract longer because there is a decrease in gastric motility, causing delayed onset. Iron and calcium tablets may not be absorbed as readily; generally, however, the amount of an oral dose that is absorbed is not affected by age.
Distribution
Older adults have a loss of protein-binding sites for drugs, which causes increased circulation of free drug and increased chance for adverse drug reaction. During the aging process, there is a loss of body water, and water-soluble drugs become more concentrated in the body. Because of an increase in body fat in the older adult, a greater amount of lipid-soluble drugs is absorbed into fat, causing a decrease in desired drug effects.
Metabolism or Biotransformation
Hepatic blood flow in the older adult may be decreased by 40% to 45%, and aging causes a decrease in liver size. Drug clearance by hepatic metabolism is affected more in older male adults than in older female adults.
Liver dysfunction, caused by the aging process, decreases enzyme function, which decreases the liver’s ability to metabolize and detoxify drugs, thereby increasing the risk of drug toxicity.
The liver and kidneys are the major organs responsible for drug clearance from the body. Biotransformation refers to drug metabolism that occurs in the liver and contributes to drug clearance. Biotransformation during hepatic metabolism can occur either in phase I by oxidation reaction or in phase II by conjugation reaction. Hepatic microsomal enzymes are responsible for phase I, oxidation reaction. Hepatic microsomal oxidation can be impaired by the aging process, liver diseases (e.g., cirrhosis, hepatitis), and drugs that reduce oxidation capability. Drug clearance by the liver is then reduced. An example of a drug that undergoes a phase I biotransformation oxidation reaction is diazepam (Valium). Diazepam is biotransformed to its active metabolite, desmethyldiazepam. In the older adult, the plasma-serum diazepam level would remain high because of an impaired phase I oxidation reaction. Other drugs that are biotransformed by phase I include barbiturates, codeine, ibuprofen, phenytoin, meperidine, lidocaine, certain benzodiazepines (alprazolam [Xanax], midazolam [Versed]), and warfarin (Coumadin).
Phase II of biotransformation involves the conjugation or attachment of the drug to an inactive state. Hepatic conjugation is usually not influenced by older age, liver diseases, or drug interaction, so the drug is inactivated and excreted in the urine. Examples of drugs that are biotransformed or metabolized by phase II are aspirin, acetaminophen, certain benzodiazepines (lorazepam [Ativan], oxazepam [Serax], temazepam [Restoril]), procainamide, and sulfanilamide. The benzodiazepines lorazepam, oxazepam, and temazepam that undergo conjugation reaction do not have active metabolites. The drug metabolic process, phase I or II, for drug clearance for the older adult patient is an important consideration with drug selection.
To assess liver function, liver enzymes must be checked. Elevated levels indicate possible liver dysfunction. The older adult could have normal liver function test (LFT) results and still have impaired hepatic microsomal enzyme-drug oxidation reactions.
Excretion
Cardiac output and blood flow throughout the circulatory system are decreased in older adults, affecting blood flow to the liver and kidneys. After age 65 years, nephron function may be decreased by 35%; after age 70 years, blood flow to the kidneys may be decreased by 40%.
Kidney function is assessed by monitoring urine output, laboratory values of BUN and serum creatinine (Cr), and creatinine clearance (CLcr or CrCl) (estimated). Creatinine clearance is an indicator of glomerular filtration rate (GFR). To evaluate renal function based on serum creatinine alone may not be accurate for the older adult because of the decrease in muscle mass that can cause a decrease in serum creatinine. Creatinine, a by-product of muscle catabolism, is primarily excreted by the kidneys. With older adult patients, serum creatinine may be within normal values because of a lack of muscle mass, but there still could be a decrease in renal function.
The 24-hour creatinine clearance test and the serum creatinine level should be used to evaluate renal function. If a 24-hour creatinine clearance test is not feasible, the following formulas can be used to estimate creatinine clearance:
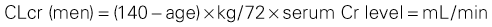
The normal creatinine clearance value for an adult is 80 to 130 mL/min.
With liver and kidney dysfunction, the efficacy of a drug dose is usually increased. Multiple drug use may intensify drug effect in the older adult. When the efficiency of the hepatic and renal systems is reduced, the half-life of the drug is prolonged and drug toxicity is probable.
Adverse Reactions
Factors contributing to adverse reactions in the older adult include a loss of protein-binding sites, which increases the amount of free circulating drug; a decline in hepatic first-pass metabolism; and a prolonged half-life of the drug because of decreased liver and kidney function. Because of these factors, the time interval between doses of a drug may need to be increased, or the dose decreased, for the older adult patient.
Pharmacodynamics
Because there is a lack of affinity to receptor sites throughout the body in the older adult, the pharmacodynamic response may be altered. The older adult could be more or less sensitive to drug action because of age-related changes in the central nervous system (CNS), changes in the number of drug receptors, and changes in the affinity of receptors to drugs. Frequently, the drug dose must be lowered. Consideration of changes in organ function is important in drug dosing.
In the older adult patient, the compensatory response to physiologic changes is decreased. When a drug with vasodilator properties is administered and the sympathetic feedback does not occur quickly, orthostatic hypotension (i.e., rapid decrease in blood pressure when changing position quickly) could result. In the younger adult, the sympathetic response of vasoconstriction works to avert a severe hypotensive effect.
Effects of Selected Drug Groups on Older Adults
Hypnotics, diuretics and antihypertensives, cardiac glycosides, anticoagulants, antibacterials (antibiotics), GI drugs (antiulcers, laxatives), antidepressants, and opioid analgesics are drug categories for which drug effects on the older adult are possible. The number of drugs taken, drug interactions (see Chapter 4), and physical health of the older adult (cardiac, renal, and hepatic function) are factors associated with drug effects in the older adult population. Drug selection is extremely important. Drugs with a shorter half-life are less likely to cause problems as a result of drug accumulation than drugs with a long half-life. If severe side effects occur, the drug with a shorter half-life is eliminated more quickly than the drug with a longer half-life.
Evaluation of hepatic and renal function is imperative, especially if the older adult takes multiple drugs. When side effects and adverse reactions occur, prescription and nonprescription drugs should be assessed (Herbal Alert 8-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 , half-life.
, half-life.