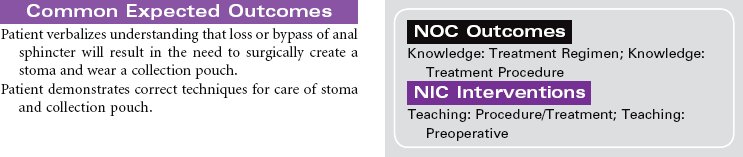
Chapter 8 Overweight; Obesity; Gastric Banding; Gastric Bypass
Gastrointestinal and Digestive Care Plans
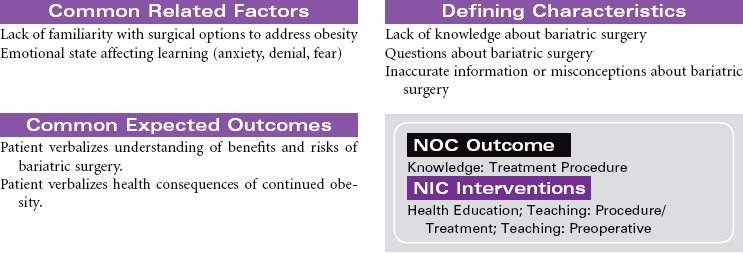
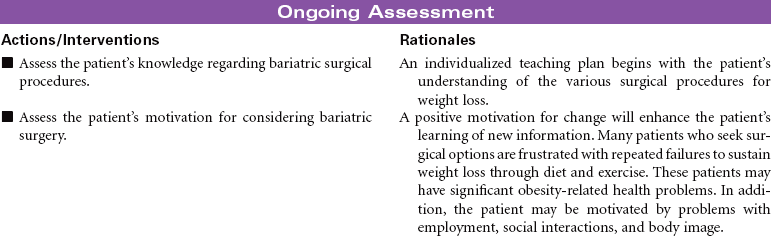
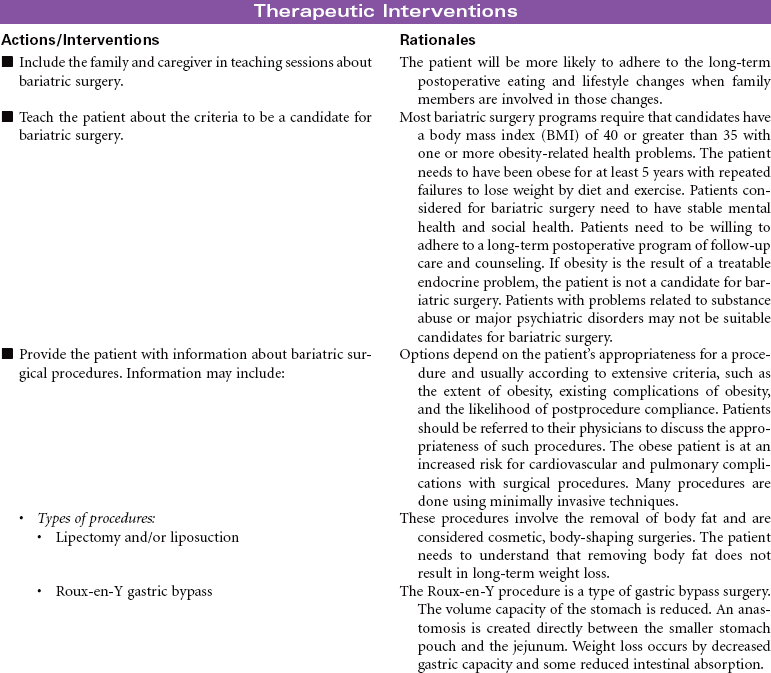
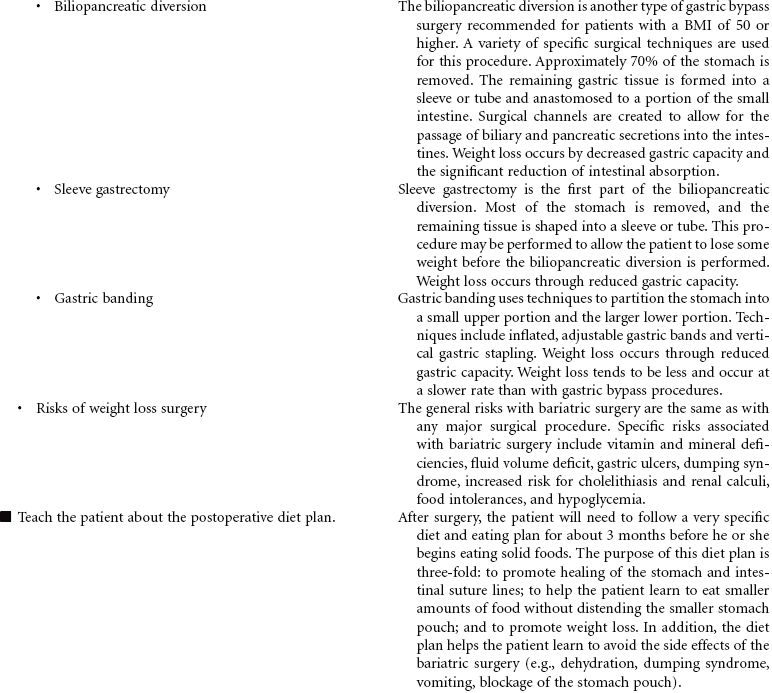
Bariatric Surgery
![]() For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
Gastrointestinal and Digestive Care Plans
Get Clinical Tree app for offline access

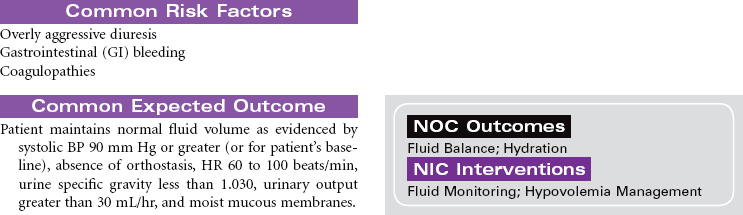
 = Independent
= Independent  = Collaborative
= Collaborative