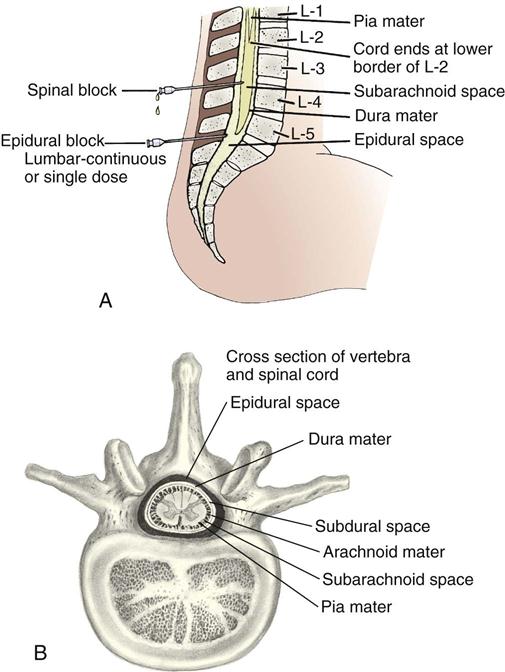
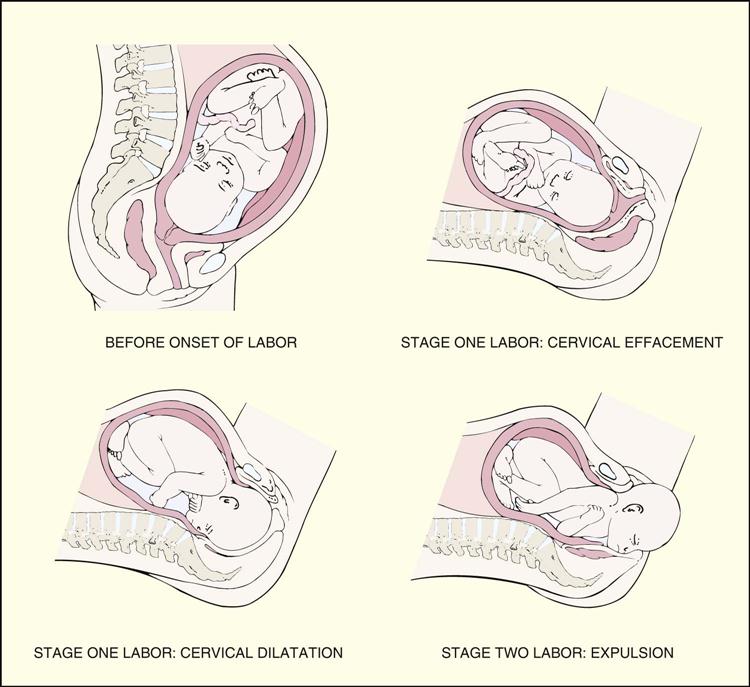
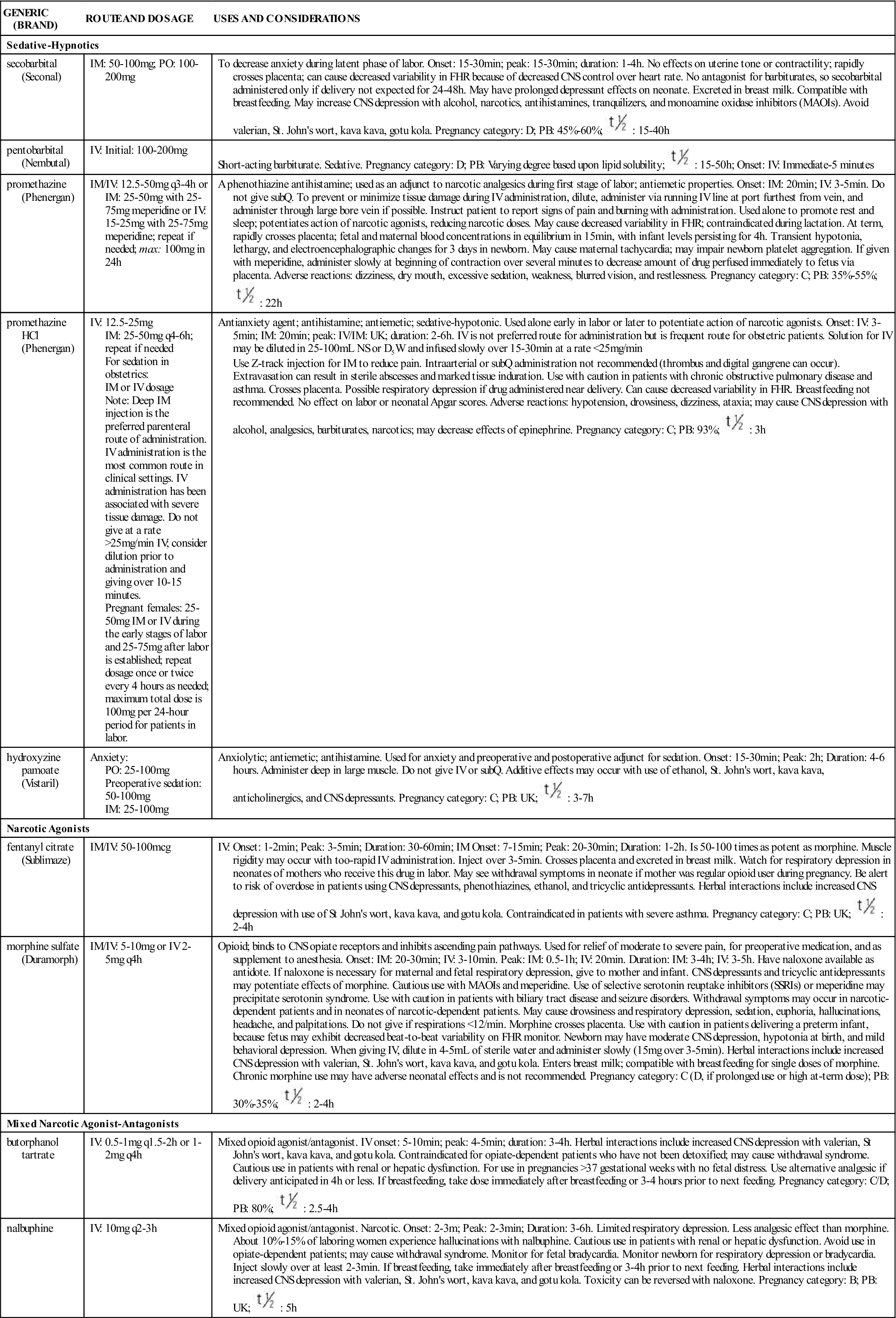
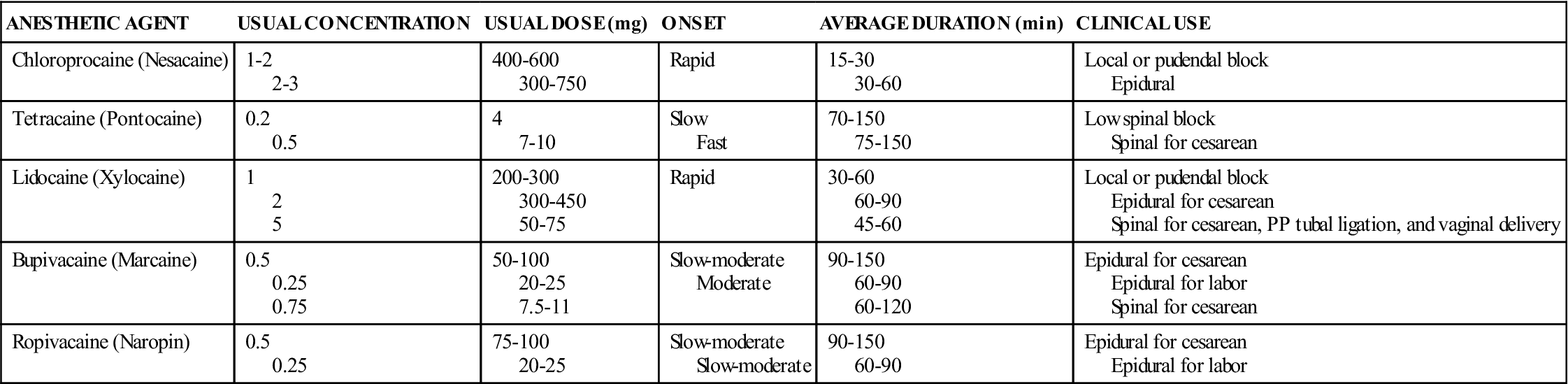
Robin Webb Corbett and Laura K. Williford Owens Bishop score, p. 816 cervical ripening, p. 816 ergot alkaloids, p. 820 ergotism, p. 820 labor augmentation, p. 817 labor induction, p. 816 respiratory distress syndrome, p. 821 surfactant, p. 821 uterine contractility, p. 817 uterine inertia, p. 817 Labor and delivery are divided into four stages, the first three specific to labor and delivery. During the first stage, the dilating stage, cervical effacement and dilation occur; the cervix thins and becomes fully dilated at 10 cm. The first stage consists of three phases categorized by cervical dilation: the latent phase (0 to 4 cm), the active phase (4 to 7 cm), and the transition phase (8 to 10 cm). The second stage of labor, the pelvic stage, begins with complete cervical dilation and ends with delivery of the newborn (Figure 54-1). During the third stage of labor, the placenta separates from the uterine wall and is delivered. The fourth stage of labor, or the first 1 to 4 hours postpartum, is a period of physiologic stabilization for the mother and initiation of familial attachment. During the first stage of labor, uterine contractions produce progressive cervical effacement and dilation. As the first stage of labor progresses, uterine contractions become stronger, longer, and more frequent, and discomfort increases. Pain and discomfort in labor are caused by uterine contraction, cervical dilation and effacement, hypoxia of the contracting myometrium, and perineal pressure from the presenting part. Pain perception is influenced by physiologic, psychological, social, and cultural factors, in particular, the woman’s past experience with pain, anticipation of pain, fear and anxiety, knowledge deficit of the labor and delivery process, and involvement of support persons. Before administering pharmacologic treatment, nonpharmacologic measures should be initiated. Nonpharmacologic measures for pain relief during labor include (1) ambulation, (2) supportive positioning of the gravid uterus and promotion of uterine perfusion, (3) touch and massage, (4) hygiene and comfort measures, (5) support persons, (6) breathing and relaxation techniques, (7) transcutaneous electrical nerve stimulation, (8) hypnosis, (9) acupuncture, and (10) hydrotherapy (warm-water baths or showers). Other nonpharmacologic measures include alternative and complementary medicine. Of particular concern is the use of herbal supplements by the pregnant patient later in pregnancy to stimulate labor. For example, some women ingest pregnancy toner tea, which includes raspberry, nettles, dandelion, alfalfa, and peppermint leaf. Other herbal supplements used include blue cohosh, castor oil, and evening primrose oil. Pregnant patients may self-administer, or the practice may be part of their traditional beliefs and framework of health. Concerns with herbal supplements are related to the often numerous physiologic active components of the herbs, adulterants, inconsistent dosing, and lack of proven efficacy. Herbs taken in late pregnancy may contribute to preterm labor or increased bleeding during delivery. Nurses must be culturally sensitive to the use of herbal supplements and health practices during pregnancy, specifically in the latter gestational weeks. When pharmacologic intervention is needed for pain relief, drugs are used as an adjunct to nonpharmacologic measures. Drugs should be selected not only to decrease the patient’s pain but also to minimize side effects for the patient and the fetus or neonate. Pain relief in labor can be obtained with systemic analgesics and regional anesthesia. Analgesics alter the patient’s perception and sensation of pain without producing unconsciousness. Systemic medications used during labor include sedative-tranquilizers, narcotics agonists, and mixed narcotic agonist-antagonists; these may be administered orally (sedative-hypnotic drugs), intravenously (IV), or intramuscularly (IM) (Table 54-1). Because of the variable response and blood levels with intramuscular administration, these drugs are more commonly administered intravenously. These medications should be administered at the onset of the uterine contraction, because parenteral administration at the onset of the contraction decreases neonatal drug exposure as blood flow is decreased to the uterus and fetus. TABLE 54-1 COMMON SYSTEMIC MEDICATIONS USED FOR PAIN RELIEF IN LABOR The sedative-tranquilizer drugs are most commonly given for false labor, latent labor, or with ruptured membranes without true labor. These drugs may also be administered to minimize maternal anxiety and fear. These drugs promote rest and relaxation and decrease fear and anxiety, but they do not provide pain relief. The sedative drugs most commonly used are barbiturates or hypnotics—generally secobarbital sodium (Seconal) and pentobarbital sodium (Nembutal). Other drugs, such as phenothiazine derivatives and hydroxyzine, can be given alone during early labor or in combination with narcotic agonists when the patient is in active labor. In addition to decreasing anxiety and apprehension, these drugs potentiate the analgesic action of the opioids and minimize emesis. These drugs include promethazine (Phenergan), a phenothiazine, and hydroxyzine hydrochloride (Vistaril), a sedative-hypnotic. The second group of drugs given for active labor are the narcotic agonists. These drugs may be administered parenterally or via regional blocks. When administered with neuraxial anesthesia, a lower dose of anesthetic is required for effective pain relief, thereby minimizing side effects. These drugs interfere with pain impulses at the subcortical level of the brain. To effect pain relief, opioids interact with mu and kappa receptors. For example, morphine sulfate activates both mu and kappa receptors. Meperidine (Demerol) is the most commonly prescribed synthetic opioid for pain control during labor. A second narcotic agonist used for pain relief during labor is fentanyl (Sublimaze). Fentanyl is a short-acting synthetic opioid that is best administered IV because of its short duration of action. Morphine sulfate may also be used for pain control in active labor, but it is less frequently used. High doses of opioids are required for effective labor analgesia when administered parenterally. The third group of systemic medications used for pain relief in labor are opioids with mixed narcotic agonist-antagonist effects. These drugs exert their effects at more than one site—often an agonist at one site and an antagonist at another. The two most commonly used narcotic-agonist-antagonist drugs are butorphanol tartrate and nalbuphine. A primary advantage of these drugs is their dose-ceiling effect. This means additional doses do not increase the degree of respiratory depression, maternal and/or neonatal, so there is less respiratory depression with these drugs than with opioids. The respiratory depression ceiling effect is believed to result from activation of kappa agonists and weak mu antagonists. Adverse effects of sedative-hypnotic drugs (secobarbital, pentobarbital) include paradoxically increased pain and excitability, lethargy, subdued mood, decreased sensory perception, and hypotension. Fetal and neonatal side effects include decreased fetal heart rate (FHR) variability and neonatal respiratory depression, sleepiness, hypotonia, and delayed breastfeeding with poor sucking response for up to 4 days. Side effects of phenothiazine derivatives and antiemetics/antihistamines (promethazine, hydroxyzine) include confusion, disorientation, excess sedation, dizziness, hypotension, tachycardia, blurred vision, headache, restlessness, weakness, and urinary retention with promethazine, and drowsiness, dry mouth, dizziness, headache, blurred vision, dysuria, urinary retention, and constipation with hydroxyzine. Decreased FHR variability occurs, and the neonate can experience moderate central nervous system (CNS) depression, hypotonia, lethargy, poor feeding, and hypothermia. The adverse effects of opioids depend on the responses activated by the mu and kappa receptors. Activation of mu receptors results in analgesia, decreased gastrointestinal (GI) motility, euphoria, respiratory depression, sedation, and physiologic dependence. In contrast, activation of kappa receptors results in analgesia, decreased gastrointestinal motility, miosis, and sedation. When parenterally administered, the side effects of opioids include nausea, vomiting, sedation, orthostatic hypotension, pruritus, and maternal and neonatal respiratory depression. The associated nausea and vomiting result from stimulation of the chemoreceptor trigger zone in the medulla. Motor block is another concern. Mothers may not walk after delivery until they are able to maintain a straight leg raise against downward pressure as applied by the practitioner. Fetal and neonatal effects include decreased FHR variability and depression of neonatal respirations and Apgar scores. Depression of neonatal neurobehavior is evidenced by lowered Apgar scores. For example, with meperidine, neonatal respiration occurs within 2 to 3 hours after administration. Neonatal respiratory depression may require reversal by administration of naloxone (Narcan). Through inhibition of both mu and kappa receptors, naloxone may reverse the effects of opioids. NOTE: With maternal administration of naloxone, there will be a subsequent increase in pain. Narcotic agonist drugs (morphine, fentanyl) can cause orthostatic hypotension, nausea, vomiting, headache, sedation, hypotension, and confusion. Decreased FHR variability and neonatal CNS depression can occur with meperidine. Mixed narcotic agonist-antagonist drugs (butorphanol tartrate, nalbuphine) can cause nausea, clamminess, sweating, sedation, respiratory depression, vertigo, lethargy, headache, and flush. Side effects in the fetus and neonate include decreased FHR variability, moderate CNS depression, hypotonia at birth, and mild behavioral depression. Anesthesia in labor and delivery represents the loss of painful sensations with or without loss of consciousness. Two types of pain are experienced in childbirth. Visceral pain from the cervix and uterus is carried by sympathetic fibers and enters the neuraxis at the thoracic 10, 11, 12, and lumbar 1 spinal levels. Early labor pain is transmitted to T11 and T12 with later progression to T10 and L1. Somatic pain is caused by pressure of the presenting part and stretching of the perineum and vagina. This pain is the pain of the transition phase and the second stage of labor and is transmitted to the sacral 2, 3, and 4 areas by the pudendal nerve. Regional anesthesia achieves pain relief during labor and delivery without loss of consciousness. Injected local anesthetic agents temporarily block conduction of painful impulses along sensory nerve pathways to the brain (Table 54-2). Regional anesthesia allows the patient to experience labor and childbirth with relief from discomfort in the blocked area. There are primarily two types of anesthesia: (1) local anesthetic agents for local infiltration (e.g., episiotomy) and (2) regional blocks (e.g., epidural; Table 54-3). The most common peridural anesthesias are spinal, epidural, and combined spinal-epidural (Figure 54-2). Other less commonly administered regional blocks include caudal, paracervical, and pudendal blocks. The anesthesiologist or nurse anesthetist is responsible for administering regional anesthesia. Nurses may assist with administration of anesthesia and monitor the patient for drug effectiveness and side effects during and after administration. TABLE 54-2 ANESTHETIC AGENTS USED IN OBSTETRICS TABLE 54-3 *The following adverse reactions/side effects apply to each of the above: Patient: hypotension; paresthesia or nerve injury, postdural puncture headache, infection, nausea, vomiting, backache, urinary retention. Headache is less common because of the small size (25 gauge) of needle used. Fetus or neonate: Few, unless secondary to maternal hypotension, then FHR late decelerations. †The following nursing considerations apply to all types of epidurals: Test dose (3 mL of lidocaine 1.5% with 1 : 200,000 epinephrine) is used to confirm correct placement of catheter; if local anesthetic is injected into vein, patient may experience dizziness, ringing in ears, numb mouth, metallic taste, or toxic response. Maternal lateral positioning is done to prevent aortocaval compression. Maternal diastolic BP should be less than 110 mm Hg before initiating the epidural. When maternal hypotension occurs, place patient on her left side, infuse IV fluids rapidly, and administer ephedrine 5 to 15 mg IV or 40 to 80 mcg phenylephrine IV. Repeat as necessary. Monitor BP every 1 to 2 minutes for first 10 minutes, then every 10 to 30 minutes until block wears off. Assess level of analgesia. After administration of the anesthetic, assess motor strength prior to ambulation. Women receiving parenteral analgesic for labor and delivery may require more focused anesthesia for episiotomies and repair of perineal lacerations. Local anesthetic agents may be administered alone, and the anesthetic agent primarily administered is lidocaine (Xylocaine). Burning at the site of injection is the most common side effect. Spinal anesthesia, also known as a saddle block, is injected in the subarachnoid space at the T10 to S5 dermatome. This anesthesia may be a single dose or administered as a combined spinal-epidural. Spinal anesthesia is administered immediately before delivery or late in the second stage when the fetal head is on the perineal floor. Drugs frequently administered either alone or in combination with the local anesthetic for a vaginal delivery include bupivacaine (Marcaine) (2.5 to 3 mg) with fentanyl (25 mcg). Dosages vary depending on whether administration of the anesthetic agent is plain or with epinephrine. Spinal anesthesia has a rapid onset, requires less local anesthetic, and may be used with high-risk patients. Postdural puncture headache is a primary concern, occurring 6 to 48 hours after dural puncture; it may also occur after accidental dural puncture with epidural anesthesia. Treatment for postdural headache includes analgesics, increased fluids, and bed rest. With resistant headaches, some health care providers may give 500 mg of caffeine in 1000 to 2000 mL of normal saline over 2 hours, though caffeine preparations have not been proved to be effective. An epidural blood patch (10 to 20 mL) is the most effective means to treat postdural headache. Lumbar epidurals may be administered as a single injection, intermittent injections, continuous patient-controlled epidural anesthesia (PCEA), and as a combined spinal-epidural. Epidurals may be administered as a single anesthetic agent or with opioids or epinephrine. Single-dose epidural anesthesia is infrequently used as analgesia and is limited to the single dosing action. Intermittent epidural bolus dosing was once commonly used for pain relief. Doses of the local anesthetic were injected intermittently via an epidural catheter. Limitations of this method included the need for frequent injections and decreased pain control because of the dosing schedule. Most frequently, patients now receive a continuous epidural infusion, which provides more consistent drug levels and more effective pain relief. Rescue doses are given as necessary to achieve pain relief. Opioids are administered with the local anesthetic to more effectively control the somatic pain of transition and second-stage labor pain. The opioids most frequently used in combination with the local anesthetic (e.g., 0.125% bupivacaine, 0.2% ropivacaine) are fentanyl or sufentanil (Sufenta). Fentanyl or sufentanil are lipophilic opioids commonly used with continuous or PCEA epidural. These opioids offer rapid analgesia and fewer side effects than hydrophilic opioids. In contrast, morphine sulfate and hydromorphone are hydrophilic opioids. They have a slower onset of action, variable duration, and increased side effects, specifically respiratory depression (Table 54-4). TABLE 54-4 PARENTERAL OPIOIDS FOR LABOR AND DELIVERY
Female Reproductive Cycle II
Labor, Delivery, and Preterm Neonatal Drugs
Objectives
Key Terms
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
Drugs for Pain Control during Labor
Analgesia/Sedation
GENERIC (BRAND)
ROUTE AND DOSAGE
USES AND CONSIDERATIONS
Sedative-Hypnotics
secobarbital (Seconal)
IM: 50-100 mg; PO: 100-200 mg
To decrease anxiety during latent phase of labor. Onset: 15-30 min; peak: 15-30 min; duration: 1-4 h. No effects on uterine tone or contractility; rapidly crosses placenta; can cause decreased variability in FHR because of decreased CNS control over heart rate. No antagonist for barbiturates, so secobarbital administered only if delivery not expected for 24-48 h. May have prolonged depressant effects on neonate. Excreted in breast milk. Compatible with breastfeeding. May increase CNS depression with alcohol, narcotics, antihistamines, tranquilizers, and monoamine oxidase inhibitors (MAOIs). Avoid valerian, St. John’s wort, kava kava, gotu kola. Pregnancy category: D; PB: 45%-60%;  : 15-40 h
: 15-40 h
pentobarbital (Nembutal)
IV: Initial: 100-200 mg
Short-acting barbiturate. Sedative. Pregnancy category: D; PB: Varying degree based upon lipid solubility;  : 15-50 h; Onset: IV: Immediate-5 minutes
: 15-50 h; Onset: IV: Immediate-5 minutes
promethazine (Phenergan)
IM/IV: 12.5-50 mg q3-4h or IM: 25-50 mg with 25-75 mg meperidine or IV: 15-25 mg with 25-75 mg meperidine; repeat if needed; max: 100 mg in 24 h
A phenothiazine antihistamine; used as an adjunct to narcotic analgesics during first stage of labor; antiemetic properties. Onset: IM: 20 min; IV: 3-5 min. Do not give subQ. To prevent or minimize tissue damage during IV administration, dilute, administer via running IV line at port furthest from vein, and administer through large bore vein if possible. Instruct patient to report signs of pain and burning with administration. Used alone to promote rest and sleep; potentiates action of narcotic agonists, reducing narcotic doses. May cause decreased variability in FHR; contraindicated during lactation. At term, rapidly crosses placenta; fetal and maternal blood concentrations in equilibrium in 15 min, with infant levels persisting for 4 h. Transient hypotonia, lethargy, and electroencephalographic changes for 3 days in newborn. May cause maternal tachycardia; may impair newborn platelet aggregation. If given with meperidine, administer slowly at beginning of contraction over several minutes to decrease amount of drug perfused immediately to fetus via placenta. Adverse reactions: dizziness, dry mouth, excessive sedation, weakness, blurred vision, and restlessness. Pregnancy category: C; PB: 35%-55%;  : 22 h
: 22 h
promethazine HCl (Phenergan)
IV: 12.5-25 mg
IM: 25-50 mg q4-6h; repeat if needed
For sedation in obstetrics:
IM or IV dosage
Note: Deep IM injection is the preferred parenteral route of administration. IV administration is the most common route in clinical settings. IV administration has been associated with severe tissue damage. Do not give at a rate >25 mg/min IV; consider dilution prior to administration and giving over 10-15 minutes.
Pregnant females: 25-50 mg IM or IV during the early stages of labor and 25-75 mg after labor is established; repeat dosage once or twice every 4 hours as needed; maximum total dose is 100 mg per 24-hour period for patients in labor.
Antianxiety agent; antihistamine; antiemetic; sedative-hypotonic. Used alone early in labor or later to potentiate action of narcotic agonists. Onset: IV: 3-5 min; IM: 20 min; peak: IV/IM: UK; duration: 2-6 h. IV is not preferred route for administration but is frequent route for obstetric patients. Solution for IV may be diluted in 25-100 mL NS or D5W and infused slowly over 15-30 min at a rate <25 mg/min
Use Z-track injection for IM to reduce pain. Intraarterial or subQ administration not recommended (thrombus and digital gangrene can occur). Extravasation can result in sterile abscesses and marked tissue induration. Use with caution in patients with chronic obstructive pulmonary disease and asthma. Crosses placenta. Possible respiratory depression if drug administered near delivery. Can cause decreased variability in FHR. Breastfeeding not recommended. No effect on labor or neonatal Apgar scores. Adverse reactions: hypotension, drowsiness, dizziness, ataxia; may cause CNS depression with alcohol, analgesics, barbiturates, narcotics; may decrease effects of epinephrine. Pregnancy category: C; PB: 93%;  : 3 h
: 3 h
hydroxyzine pamoate (Vistaril)
Anxiety:
PO: 25-100 mg
Preoperative sedation: 50-100 mg
IM: 25-100 mg
Anxiolytic; antiemetic; antihistamine. Used for anxiety and preoperative and postoperative adjunct for sedation. Onset: 15-30 min; Peak: 2 h; Duration: 4-6 hours. Administer deep in large muscle. Do not give IV or subQ. Additive effects may occur with use of ethanol, St. John’s wort, kava kava, anticholinergics, and CNS depressants. Pregnancy category: C; PB: UK;  : 3-7 h
: 3-7 h
Narcotic Agonists
fentanyl citrate (Sublimaze)
IM/IV: 50-100 mcg
IV: Onset: 1-2 min; Peak: 3-5 min; Duration: 30-60 min; IM Onset: 7-15 min; Peak: 20-30 min; Duration: 1-2 h. Is 50-100 times as potent as morphine. Muscle rigidity may occur with too-rapid IV administration. Inject over 3-5 min. Crosses placenta and excreted in breast milk. Watch for respiratory depression in neonates of mothers who receive this drug in labor. May see withdrawal symptoms in neonate if mother was regular opioid user during pregnancy. Be alert to risk of overdose in patients using CNS depressants, phenothiazines, ethanol, and tricyclic antidepressants. Herbal interactions include increased CNS depression with use of St John’s wort, kava kava, and gotu kola. Contraindicated in patients with severe asthma. Pregnancy category: C; PB: UK;  : 2-4 h
: 2-4 h
morphine sulfate (Duramorph)
IM/IV: 5-10 mg or IV 2-5 mg q4h
Opioid; binds to CNS opiate receptors and inhibits ascending pain pathways. Used for relief of moderate to severe pain, for preoperative medication, and as supplement to anesthesia. Onset: IM: 20-30 min; IV: 3-10 min. Peak: IM: 0.5-1 h; IV: 20 min. Duration: IM: 3-4 h; IV: 3-5 h. Have naloxone available as antidote. If naloxone is necessary for maternal and fetal respiratory depression, give to mother and infant. CNS depressants and tricyclic antidepressants may potentiate effects of morphine. Cautious use with MAOIs and meperidine. Use of selective serotonin reuptake inhibitors (SSRIs) or meperidine may precipitate serotonin syndrome. Use with caution in patients with biliary tract disease and seizure disorders. Withdrawal symptoms may occur in narcotic-dependent patients and in neonates of narcotic-dependent patients. May cause drowsiness and respiratory depression, sedation, euphoria, hallucinations, headache, and palpitations. Do not give if respirations <12/min. Morphine crosses placenta. Use with caution in patients delivering a preterm infant, because fetus may exhibit decreased beat-to-beat variability on FHR monitor. Newborn may have moderate CNS depression, hypotonia at birth, and mild behavioral depression. When giving IV, dilute in 4-5 mL of sterile water and administer slowly (15 mg over 3-5 min). Herbal interactions include increased CNS depression with valerian, St. John’s wort, kava kava, and gotu kola. Enters breast milk; compatible with breastfeeding for single doses of morphine. Chronic morphine use may have adverse neonatal effects and is not recommended. Pregnancy category: C (D, if prolonged use or high at-term dose); PB: 30%-35%;  : 2-4 h
: 2-4 h
Mixed Narcotic Agonist-Antagonists
butorphanol tartrate
IV: 0.5-1 mg q1.5-2h or 1-2 mg q4h
Mixed opioid agonist/antagonist. IV onset: 5-10 min; peak: 4-5 min; duration: 3-4 h. Herbal interactions include increased CNS depression with valerian, St John’s wort, kava kava, and gotu kola. Contraindicated for opiate-dependent patients who have not been detoxified; may cause withdrawal syndrome. Cautious use in patients with renal or hepatic dysfunction. For use in pregnancies >37 gestational weeks with no fetal distress. Use alternative analgesic if delivery anticipated in 4 h or less. If breastfeeding, take dose immediately after breastfeeding or 3-4 hours prior to next feeding. Pregnancy category: C/D; PB: 80%;  : 2.5-4 h
: 2.5-4 h
nalbuphine
IV: 10 mg q2-3h
Mixed opioid agonist/antagonist. Narcotic. Onset: 2-3 m; Peak: 2-3 min; Duration: 3-6 h. Limited respiratory depression. Less analgesic effect than morphine. About 10%-15% of laboring women experience hallucinations with nalbuphine. Cautious use in patients with renal or hepatic dysfunction. Avoid use in opiate-dependent patients; may cause withdrawal syndrome. Monitor for fetal bradycardia. Monitor newborn for respiratory depression or bradycardia. Inject slowly over at least 2-3 min. If breastfeeding, take immediately after breastfeeding or 3-4 h prior to next feeding. Herbal interactions include increased CNS depression with valerian, St. John’s wort, kava kava, and gotu kola. Toxicity can be reversed with naloxone. Pregnancy category: B; PB: UK;  : 5 h
: 5 h
Adverse Reactions
Anesthesia
Regional Anesthesia
ANESTHETIC AGENT
USUAL CONCENTRATION
USUAL DOSE (mg)
ONSET
AVERAGE DURATION (min)
CLINICAL USE
Chloroprocaine (Nesacaine)
1-2
2-3
400-600
300-750
Rapid
15-30
30-60
Local or pudendal block
Epidural
Tetracaine (Pontocaine)
0.2
0.5
4
7-10
Slow
Fast
70-150
75-150
Low spinal block
Spinal for cesarean
Lidocaine (Xylocaine)
1
2
5
200-300
300-450
50-75
Rapid
30-60
60-90
45-60
Local or pudendal block
Epidural for cesarean
Spinal for cesarean, PP tubal ligation, and vaginal delivery
Bupivacaine (Marcaine)
0.5
0.25
0.75
50-100
20-25
7.5-11
Slow-moderate
Moderate
90-150
60-90
60-120
Epidural for cesarean
Epidural for labor
Spinal for cesarean
Ropivacaine (Naropin)
0.5
0.25
75-100
20-25
Slow-moderate
Slow-moderate
90-150
60-90
Epidural for cesarean
Epidural for labor
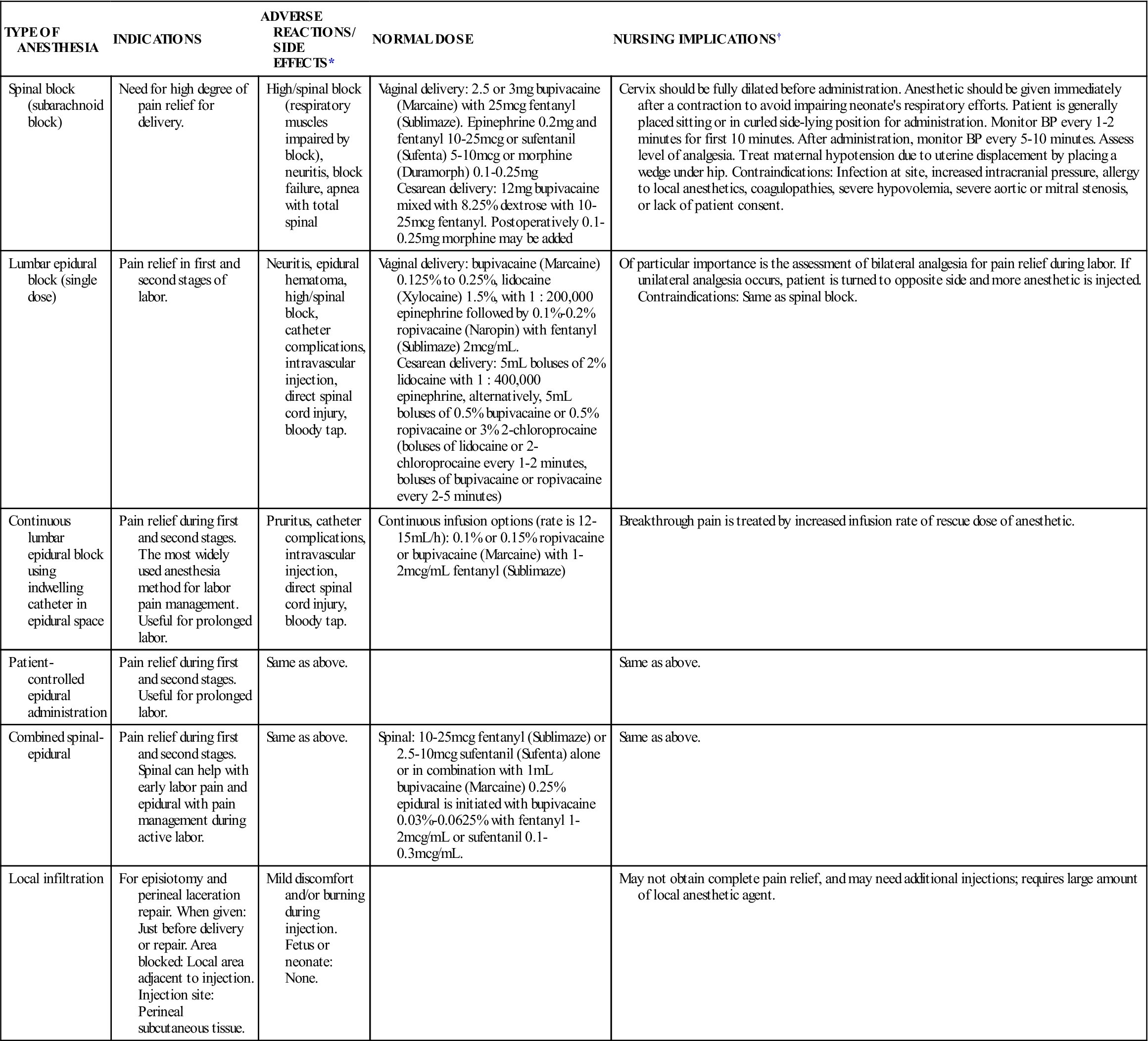
TYPE OF ANESTHESIA
INDICATIONS
ADVERSE REACTIONS/ SIDE EFFECTS*
NORMAL DOSE
NURSING IMPLICATIONS†
Spinal block (subarachnoid block)
Need for high degree of pain relief for delivery.
High/spinal block (respiratory muscles impaired by block), neuritis, block failure, apnea with total spinal
Vaginal delivery: 2.5 or 3 mg bupivacaine (Marcaine) with 25 mcg fentanyl (Sublimaze). Epinephrine 0.2 mg and fentanyl 10-25 mcg or sufentanil (Sufenta) 5-10 mcg or morphine (Duramorph) 0.1-0.25 mg
Cesarean delivery: 12 mg bupivacaine mixed with 8.25% dextrose with 10-25 mcg fentanyl. Postoperatively 0.1-0.25 mg morphine may be added
Cervix should be fully dilated before administration. Anesthetic should be given immediately after a contraction to avoid impairing neonate’s respiratory efforts. Patient is generally placed sitting or in curled side-lying position for administration. Monitor BP every 1-2 minutes for first 10 minutes. After administration, monitor BP every 5-10 minutes. Assess level of analgesia. Treat maternal hypotension due to uterine displacement by placing a wedge under hip. Contraindications: Infection at site, increased intracranial pressure, allergy to local anesthetics, coagulopathies, severe hypovolemia, severe aortic or mitral stenosis, or lack of patient consent.
Lumbar epidural block (single dose)
Pain relief in first and second stages of labor.
Neuritis, epidural hematoma, high/spinal block, catheter complications, intravascular injection, direct spinal cord injury, bloody tap.
Vaginal delivery: bupivacaine (Marcaine) 0.125% to 0.25%, lidocaine (Xylocaine) 1.5%, with 1 : 200,000 epinephrine followed by 0.1%-0.2% ropivacaine (Naropin) with fentanyl (Sublimaze) 2 mcg/mL.
Cesarean delivery: 5 mL boluses of 2% lidocaine with 1 : 400,000 epinephrine, alternatively, 5 mL boluses of 0.5% bupivacaine or 0.5% ropivacaine or 3% 2-chloroprocaine (boluses of lidocaine or 2-chloroprocaine every 1-2 minutes, boluses of bupivacaine or ropivacaine every 2-5 minutes)
Of particular importance is the assessment of bilateral analgesia for pain relief during labor. If unilateral analgesia occurs, patient is turned to opposite side and more anesthetic is injected. Contraindications: Same as spinal block.
Continuous lumbar epidural block using indwelling catheter in epidural space
Pain relief during first and second stages. The most widely used anesthesia method for labor pain management. Useful for prolonged labor.
Pruritus, catheter complications, intravascular injection, direct spinal cord injury, bloody tap.
Continuous infusion options (rate is 12-15 mL/h): 0.1% or 0.15% ropivacaine or bupivacaine (Marcaine) with 1-2 mcg/mL fentanyl (Sublimaze)
Breakthrough pain is treated by increased infusion rate of rescue dose of anesthetic.
Patient-controlled epidural administration
Pain relief during first and second stages. Useful for prolonged labor.
Same as above.
Same as above.
Combined spinal-epidural
Pain relief during first and second stages. Spinal can help with early labor pain and epidural with pain management during active labor.
Same as above.
Spinal: 10-25 mcg fentanyl (Sublimaze) or 2.5-10 mcg sufentanil (Sufenta) alone or in combination with 1 mL bupivacaine (Marcaine) 0.25% epidural is initiated with bupivacaine 0.03%-0.0625% with fentanyl 1-2 mcg/mL or sufentanil 0.1-0.3 mcg/mL.
Same as above.
Local infiltration
For episiotomy and perineal laceration repair. When given: Just before delivery or repair. Area blocked: Local area adjacent to injection. Injection site: Perineal subcutaneous tissue.
Mild discomfort and/or burning during injection. Fetus or neonate: None.
May not obtain complete pain relief, and may need additional injections; requires large amount of local anesthetic agent.
OPIOID
DOSAGE
ANALGESIC EFFECT BEGINS
PEAK ANALGESIC EFFECT
DURATION OF ACTION
meperidine (Demerol)
IM: 50-100 mg
IV: 25-50 mg
IM: 10-45 min
IV: <5 min
IM: 30-50 min
IV: 5-10 min
IM: 2-4 h
IV: 2-3 h
fentanyl (Sublimaze)
IM: 50-100 mcg
IV: 50-100 mcg
IM: 7-15 min
IV: Almost immediately
IM: 30 min
IV: 3-5 min
IV: 30-60 min
IM: 1-2 h
morphine sulfate (Duramorph)
IM: 10 mg
IV: 2-5 mg
IM: 15-60 min
IV: 5-10 min
IM: 1-2 h
IV: 20 min
IM: 3-5 h
IV: 3-5 h
nalbuphine
subQ: 5-10 mg
IV: 5-10 mg
subQ: <15 min
IV: <1-3 min
subQ: N/A
IV: 30 min
subQ: 3-6 h
IV: 3-4 h
butorphanol
IM: 1-2 mg
IV: 1-2 mg
IM: 5-10 min
IV: <10 min
IM: 30-60 min
IV: 4-5 min
IM: 3-4 h
IV: 2-4 h![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Female Reproductive Cycle II: Labor, Delivery, and Preterm Neonatal Drugs
Get Clinical Tree app for offline access

 , half-life; UK, unknown; <, less than, >, greater than.
, half-life; UK, unknown; <, less than, >, greater than.