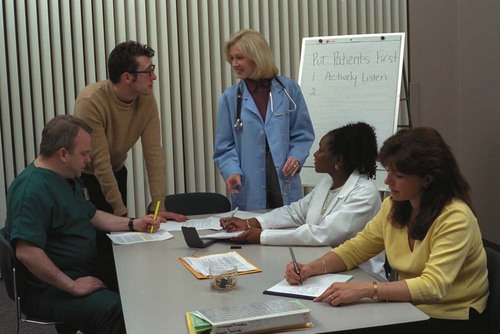
1. Identify key differences between law and ethics. 2. List reasons for medical assistants to study ethics. 3. Identify specific rights that patients have in relation to health care. 4. Correlate the concept of duties to the actions expected of health professionals. 6. Report illegal and/or unsafe activities and behaviors affecting patient care to proper authorities. 7. Describe how certain ethical issues generate ethical conflict in society. 8. Describe ways to separate and prioritize personal and professional ethics. 9. Describe six steps that may be used to make ethical decisions. Law and Professional Liability 10. Identify similarities and differences between public law and private law. 11. Identify the process through which laws are created on the federal and state level. 12. Differentiate between types of crimes, such as felonies and misdemeanors, as well as between violent and nonviolent crimes. 13. Differentiate between criminal law and civil law. 14. List and explain the elements of a valid contract. 15. State the rights and duties of each party in the physician-patient relationship. 16. Incorporate the Patient’s Bill of Rights into personal practice. 17. Define “standard of care,” and describe how this concept affects the behavior of health professionals. 18. Describe the medical assistant’s role in obtaining informed consent. 19. Explain the principles of negligence and professional negligence as they apply to the behavior of health professionals. 20. Explain the purpose and need for professional liability insurance. 21. Describe the process of malpractice litigation. 22. List and explain specific defenses to intentional and unintentional torts. Federal and State Laws Affecting the Medical Office 23. Describe and explain the laws regulating controlled substances and prescription medications. 24. List and explain several laws that protect employees of medical offices. 25. Describe how the provisions of the Health Insurance Portability and Accountability Act (HIPAA) affect the medical office. 26. List and explain the situations where mandatory reporting is required by the medical office. 27. Describe how states regulate the practice of medicine and health occupations. 28. Differentiate between licensing and voluntary accreditation for health care facilities. On the basis of personal beliefs, patients can formalize their decisions about treatment in terminal or end-of-life situations in a number of ways. These include do-not-resuscitate (DNR) orders, living wills, health care proxies, and organ donor cards, all of which fall under the heading of “advance directives” (Box 3-1). An advance directive may specify care to be given or avoided and name a person to make medical decisions for the individual should he or she become incompetent. This is usually a spouse, child older than age 18, member of the clergy, or close friend. Medical advance directives should always name a single individual to make decisions, with an alternate if possible. This is often a difficult choice, especially for an elderly person with several children (Figure 3-1). In addition, the patient may want to provide for donation of any organs that are useful. Organ donation (or donation of one’s entire body) and procedures for determining who may give permission if the patient has not left a directive are outlined in the Uniform Anatomical Gift Act. An individual or medical practice can look to a professional organization for guidance related to ethical questions. Medical associations publish guidelines related to medical ethics. Professional associations for medical assistants can be a source of information and guidelines. For problems affecting the medical office, a discussion by all office staff may assist in decision making (Figure 3-2).
Ethics and Law for the Medical Office
Introduction to Medical Ethics
Ethics and Health Care
Ethical Concepts
Ethical Conflict
Advance Directives
Personal and Professional Ethics
Ethics and Law for the Medical Office
Get Clinical Tree app for offline access