Donald L. Taylor abstinence, p. 43 addiction, p. 42 brain reward system, p. 42 chemical impairment, p. 58 craving, p. 43 cross-tolerance, p. 52 cue-induced craving, p. 43 dependence, p. 42 detoxification, p. 43 drug abuse, p. 42 drug addiction, p. 42 drug misuse, p. 42 intoxication, p. 43 Korsakoff’s psychosis, p. 52 opioids, p. 54 physical dependence, p. 42 potentiation, p. 52 psychological dependence, p. 44 relapse, p. 43 tolerance, p. 43 Wernicke’s encephalopathy, p. 52 withdrawal syndrome, p. 43 Most drugs are used safely and within prescribed guidelines, but it is possible for all drugs to be misused or abused. Drug abuse and addiction are serious and complex social and health problems that nurses address in all areas of practice. However, this chapter focuses primarily on the physiologic effects of abused drugs and the pharmacologic treatment of abuse. Cultural and social expectations influence the definitions and perception of drug abuse versus acceptable usage. In Moslem Middle Eastern populations, any use of alcohol or mind-altering drugs may be considered abuse. The same might be true in the United States among conservative religious groups. Yet in many European cultures, alcohol use is expected and present at all family and social gatherings. For many people in the United States, occasional use of marijuana and alcohol is not considered abuse, nor is the use of psychedelic agents in some Native American religious rites. Cigarette smoking, which was glamorized in the past, is now less socially acceptable than moderate alcohol use in the United States. Sociocultural factors arising from unemployment, poverty, or adverse social conditions affect the incidence of substance abuse. Individual factors, such as age, educational status, and geographic region, also affect rates of use. Metropolitan and urban areas have higher rates of substance abuse than rural areas in the United States. Additionally, the West Coast has a higher rate of use (11.0%) than the Northeast, Midwest, or South (9.4%, 8.2%, and 7.8%, respectively). A major responsibility of nurses in addressing drug abuse in ethnic and cultural groups is to assess and treat patients within their cultural perspectives, as described in Chapter 3. Although small differences exist in their definitions, the terms drug, substance, and chemical are often used interchangeably within the context of drug abuse. Drug misuse generally refers to indiscriminate or recreational use of a chemical substance or its use for purposes other than those for which it is intended. Drug abuse is culturally defined and may be considered drug use inconsistent with medical or social norms. It generally refers to an overindulgence of a chemical substance that results in a negative impact on the psychological, physical, or social functioning of an individual. Chronic abuse of a drug may lead to addiction. Drug addiction should be considered a complex disease of the central nervous system (CNS) characterized by a compulsive, uncontrolled craving for and dependence on a substance to such a degree that cessation causes severe emotional, mental, and/or physiologic reactions. Physical dependence is not necessary or sufficient for addiction to occur. Terms used in describing drug abuse are presented in Table 5-1. TABLE 5-1 Drugs abused most often are psychoactive agents that result in pleasure or modify thinking and perception. They include legal substances such as alcohol, tobacco, and prescription drugs such as analgesics, sedative-hypnotics, tranquilizers, and amphetamines. Common illegal substances that are abused include marijuana and hashish, cocaine, MDMA, and heroin. Most addictive drugs increase the availability of dopamine and other neurotransmitters in the mesolimbic system of the brain. This area has been identified as the “pleasure center” or brain reward system, an ancient system that creates the sensation of pleasure for certain behaviors necessary for survival, such as eating and sexual behavior. Normally dopamine is released at a stable rate in the mesolimbic system, maintaining a normative mood. Certain drugs such as opioids and cocaine increase the release of dopamine or decrease its reuptake at the synapse. Nicotine, alcohol, marijuana, amphetamines, and caffeine are also believed to increase dopamine activity at the synapse. The resulting increase in dopamine in the system leads to mood elevation or euphoria, factors that provide strong motivation to repeat the experience. Many addictive drugs also increase the availability of other neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), but dopamine’s effect on the reward system appears to be pivotal to the addictive process. Addiction (a compulsive, uncontrollable craving for and dependence on a substance to such a degree that cessation causes severe reactions) results from the prolonged effects of addictive drugs on the brain. Repeated use of drugs remodels the neural circuitry of the brain cells and reduces the responsiveness of receptors. This decreased responsiveness leads to tolerance—the need for a larger dose of a drug to obtain the original euphoria. As drugs of abuse result in levels of dopamine that do not naturally occur, tolerance also reduces the sense of pleasure from experiences that previously resulted in positive feelings, such as food, sex, or relationships. Without the drug, the individual may experience depression, anxiety, and/or irritability. Craving is another characteristic of addiction; one type of craving is cue-induced craving, which occurs in the presence of people, places, or things patients have previously associated with drug use. These encounters produce surges in dopamine levels, and these surges push the individual toward active drug seeking and drug taking. Cue-induced craving may occur after long periods of abstinence and is a common cause of relapse. Continued research into the biologic and genetic basis of addiction is crucial to the development of drugs to treat addiction. Increasing evidence shows that genetics play a significant role in alcoholism and nicotine use and that there are significant gender differences in drug abuse risk. A natural genetic mutation that inhibits nicotine metabolism in the brain has been identified. Men with the mutation are less likely to become addicted to nicotine and find it easier to quit smoking. However, the presence or absence of the defective gene does not affect women’s smoking. Women also have less stomach metabolism of alcohol, resulting in higher blood alcohol levels than men after the same amount of alcohol intake. A genetic difference in the activity of a liver enzyme in African Americans results in slower metabolism of nicotine, potentially resulting in the consumption of fewer cigarettes per day than Caucasian people may consume. Biologic and genetic research has led to the development of drugs to treat opioid, nicotine, and alcohol addiction. However, currently no medications are approved by the U.S Food and Drug Administration (FDA) for treating addiction to cocaine, lysergic acid diethylamide (LSD), phencyclidine hydrochloride (PCP), marijuana, methamphetamine and other stimulants, or inhalants. Intoxication is a state of being influenced, or affected by a drug or other toxic substance. This may be a very small amount of drug in the drug-naïve person, or a potentially lethal amount in the chronic user. The signs and symptoms seen for either are the toxic effects of the drug when taken in excessive amounts. Detoxification involves treating an intoxicated patient to diminish or remove drugs or their effects from the body. Treatments may involve administration of antagonistic drugs, promotion of metabolism and elimination of the drug, or intensive supportive care until the drug is naturally eliminated. Withdrawal syndrome is a group of signs and symptoms that occurs in physically dependent persons when drug use is stopped. The symptoms are often opposite the effects the drug produced before it was withdrawn. Opioids, alcohol, barbiturates, and anxiolytics cause relatively strong physical dependence and withdrawal syndrome. Cannabinoids and amphetamines cause weaker physical dependence. Hallucinogens such as LSD do not cause physical dependence or abstinence signs. Withdrawal syndrome is treated by slow weaning of the drugs, or use of “cross-tolerant” drugs to control symptoms, and supportive care. To promote cessation and abstinence of the abused drug, treatment with other drugs may be used to decrease craving and prevent withdrawal syndrome. Specific receptor blockers, less potent drugs of the same class, or nonaddicting substitutes are treatment options. In addition to the use of drugs to maintain abstinence, cognitive-behavioral therapies enhance the effectiveness of medications and are recommended for treatment of all drug abuse and addiction. Nicotine is the alkaloid in tobacco that causes dependence and is the most rapidly addicting of the drugs of abuse. Smoking cigarettes is the most damaging method of nicotine use. Cigarette smoke contains more than 4000 chemicals and gases, including at least 45 cancer-causing or tumor-promoting agents and a number of hydrocarbons or solvents. Although nicotine is not believed to be carcinogenic, it is the addictive substance and has no therapeutic value. Nicotine is rapidly absorbed into the blood through the lungs in smoking and more slowly through the buccal mucosa in chewing and the nasal mucosa in snuffing. It crosses membranes easily and is widely distributed throughout the body. Nicotine passes freely into breast milk and may be toxic to the nursing infant. Plasma protein binding of nicotine is less than 5%. The liver is the major site of nicotine metabolism. Nicotine and its more than 20 metabolites are eliminated in the urine. The elimination half-life of nicotine is 1 to 2 hours. In low doses, such as those obtained through cigarettes, nicotine activates nicotinic receptors. Most effects occur from activated receptors in autonomic ganglia and the adrenal medulla. In the CNS, nicotine rapidly acts on the mesolimbic reward system of the brain, promoting the release of dopamine and mimicking the effects of cocaine and other highly addictive substances. Stimulation of nicotinic receptors in the sympathetic ganglia and the adrenal medulla result in marked cardiovascular stimulation and increased myocardial oxygen consumption. In the brain, the action of nicotine causes general CNS stimulation. Physical effects include increased respiratory rate and tremors. Psychological effects include increased alertness and arousal. In the gastrointestinal (GI) tract, nicotine increases GI secretions and smooth-muscle tone. Many abusers of nicotine report that nicotine has a depressant effect, promoting relaxation and relief of anxiety. However, it is thought that these effects actually occur when periodic nicotine withdrawal is relieved by further nicotine. Nicotine causes a very strong psychological dependence. In addition, physiologic dependence occurs with regular heavy use. Withdrawal symptoms may occur within the first few hours after stopping smoking, peak in 24 to 48 hours, and last from a few weeks to several months. After withdrawal subsides, cue-induced craving may cause smoking relapse. The effects of nicotine and symptoms of withdrawal are presented in Table 5-2. TABLE 5-2 EFFECTS OF FREQUENTLY ABUSED DRUGS Treatment of nicotine addiction has received considerable attention in the past few years because of its association with preventable illness and death. Chronic smoking can affect nearly every organ of the body. In addition to cardiovascular disease, chronic lung disease, and cancers of the larynx, lung, esophagus, oral cavity, and bladder, smoking is now associated with leukemia, cataracts, abdominal aortic aneurysm, and cancers of the cervix, kidney, pancreas, and stomach. To help end thousands of these unnecessary health problems, nurses must be proactive in identifying and talking with tobacco users and providing them with information on ways to stop the use of tobacco. Several drug products are available to aid smoking cessation. Except in special circumstances, nicotine replacement therapy (NRT) or other smoking cessation agents are recommended for all tobacco users in addition to behavioral and support therapies. Five NRTs in the form of gum, lozenges, transdermal patches, nasal spray, and inhalers have been approved by the FDA to reduce the craving and withdrawal symptoms associated with tobacco cessation. These agents enable a smoker to reduce nicotine previously obtained from cigarettes with a system that provides slower delivery of the drug and eliminates the carcinogens and gases associated with tobacco smoke. Table 5-3 describes various nicotine replacement products. TABLE 5-3 Bupropion is an atypical (heterocyclic) antidepressant unrelated to nicotine that has been approved by the FDA for smoking cessation. The exact mechanism of action of bupropion is unknown. It is thought to inhibit neuronal reuptake of dopamine, and to a lesser degree norepinephrine, and this reduces the urge to smoke and minimizes some symptoms of nicotine withdrawal. Bupropion may be combined with NRT to provide additional benefit. Bupropion is marketed as Zyban for smoking cessation. Serious negative effects of bupropion use include agitation, hostility, increased depression or other psychiatric symptoms, and suicidality. Varenicline (Chantix) is a novel drug approved for smoking cessation that is an alternative to NRT and bupropion. It is a nicotinic receptor partial agonist that reduces cravings for nicotine and decreases the pleasurable effects of cigarettes and other tobacco products if tobacco is used. The approved course of varenicline treatment is 12 weeks, and those who successfully quit smoking during treatment may continue with an additional 12 weeks to increase long-term cessation. In clinical trials, the most common adverse effects were nausea, headache, vomiting, flatulence, insomnia, abnormal dreams, and a change in taste perception; serious negative effects are similar to those for bupropion. Nortriptyline (Aventyl, Pamelor) and clonidine (Catapres) are used as second-line drugs to reduce nicotine withdrawal symptoms and promote cessation. These drugs are not approved by the FDA for this purpose, and their action in nicotine addiction is not clearly understood. Nortriptyline is a tricyclic antidepressant (see Chapter 28). Clonidine is a centrally acting alpha2 agonist used to treat hypertension (see Chapter 44). Research related to the development of new agents and new uses of approved drugs in smoking cessation is a priority of the National Institute for Drug Abuse. Clinical trials are currently in progress to examine the effects of various combinations of nicotine-replacement agents, combinations of nicotine-replacement agents with antidepressants, neurotransmitter modulators, nicotine vaccines that produce antibodies that bind in the blood with nicotine, and nicotine receptor–blocking agents. More information on nicotine abuse and its effects can be found in the discussion of lower respiratory disorders in Chapter 41. Cocaine is a naturally occurring potent stimulant, an alkaloid that was originally obtained from the leaves of the coca plant but today can be prepared synthetically. Historically, cocaine was used as a local anesthetic, but it has been largely replaced by synthetic agents with no abuse potential. Cocaine is a Schedule II drug under the Controlled Substances Act. Illicit cocaine is available as white powder (cocaine hydrochloride) and as cocaine base (alkaloidal cocaine, freebase), a crystalline substance. “Crack,” a cocaine base that gets its name from the popping sound the crystals make when heated, is popular because it is less expensive, readily available, and easy to use, and has increased purity over cocaine hydrochloride. Absorption rates of cocaine depend on the route of administration. Cocaine hydrochloride is usually “snorted” intranasally. Cocaine can also be smoked as crack cocaine or in “freebase” form, injected intravenously (IV), taken orally, or absorbed through the mucous membranes. Smoking and IV methods result in the fastest absorption and the highest “rush.” Peak blood levels develop within 5 to 30 minutes with most methods of administration. The longest effects occur following intranasal use because absorption is delayed by vasoconstriction of the nasal vessels. Cocaine is rapidly metabolized by the liver. Elimination half-lives by oral, intranasal, and IV routes are 50, 80, and 60 minutes, respectively. Tolerance appears to occur with long-term use, but users can also become more sensitive to the drug’s anesthetic and convulsant effects. Cocaine readily crosses the placenta in pregnant patients and accumulates in the fetal circulation. Conflicting research exists about the effect of prenatal cocaine exposure on the development of the child. Cocaine inhibits the neuronal uptake of dopamine in the brain and increases the activation of dopamine receptors in the brain reward system. This action magnifies pleasures and leads to rapid dependence. Cocaine also increases norepinephrine at postsynaptic receptor sites, producing intense vasoconstriction and cardiovascular stimulation. Drug interactions with cocaine are identified in Table 5-4. TABLE 5-4 DRUG INTERACTIONS: DRUGS OF ABUSE
Drugs of Abuse
Objectives
Key Terms
Context of Drug Abuse
Cultural Considerations
Definitions
TERM
DEFINITION
Abstinence
Sustained avoidance of substance use.
Addiction
A compulsive, uncontrollable craving for and dependence on a substance to such a degree that cessation causes severe emotional, mental, or physiologic reactions.
Chemical impairment
A term used by health professionals to describe behaviors related to the effects of drugs or substances on performance.
Craving
Subjective need for a substance, usually experienced after decreased use or abstinence. Cue-induced craving is stimulated in the presence of situations previously associated with drug taking.
Dependence
Reliance on a substance that has reached the level that its absence will cause impairment in function.
Psychological
Compulsive need to experience pleasurable response from the substance.
Physical
Altered physiologic state from prolonged substance use; regular use is necessary to prevent withdrawal syndrome.
Drug abuse
Overindulgence in and dependence on a substance that has a negative impact on psychological, physiologic, and social functioning of an individual; synonymous with chemical dependence.
Drug misuse
Indiscriminate use of a drug for purposes other than those for which it is intended.
Relapse
Return to substance use during abstinence.
Substance
Drug, chemical, or biologic entity.
Tolerance
Decreased effect of a substance that results from repeated exposure. It is possible to develop cross-tolerance to other substances in the same category.
Withdrawal syndrome
Constellation of physiologic and psychological responses that occur when there is abrupt cessation or reduced intake of a substance on which an individual is dependent or when the effect is counteracted by a specific antagonist.
Neurobiology of Addictive Drugs
Overview of Addictive States
Intoxication
Detoxification
Withdrawal Syndrome
Cessation and Maintenance of Abstinence
Stimulants
Nicotine
Pharmacokinetics
Pharmacodynamics
Side Effects and Adverse Reactions
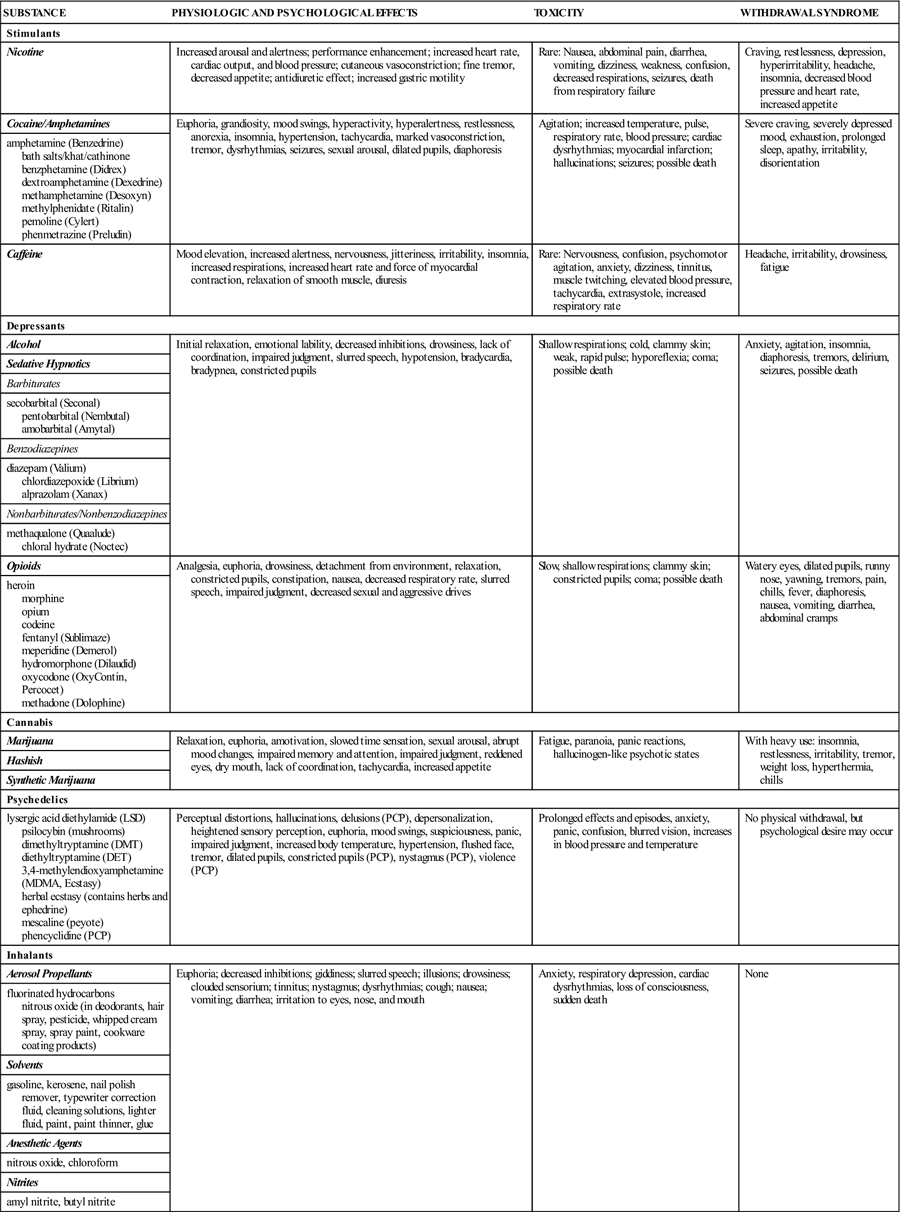
SUBSTANCE
PHYSIOLOGIC AND PSYCHOLOGICAL EFFECTS
TOXICITY
WITHDRAWAL SYNDROME
Stimulants
Nicotine
Increased arousal and alertness; performance enhancement; increased heart rate, cardiac output, and blood pressure; cutaneous vasoconstriction; fine tremor, decreased appetite; antidiuretic effect; increased gastric motility
Rare: Nausea, abdominal pain, diarrhea, vomiting, dizziness, weakness, confusion, decreased respirations, seizures, death from respiratory failure
Craving, restlessness, depression, hyperirritability, headache, insomnia, decreased blood pressure and heart rate, increased appetite
Cocaine/Amphetamines
Euphoria, grandiosity, mood swings, hyperactivity, hyperalertness, restlessness, anorexia, insomnia, hypertension, tachycardia, marked vasoconstriction, tremor, dysrhythmias, seizures, sexual arousal, dilated pupils, diaphoresis
Agitation; increased temperature, pulse, respiratory rate, blood pressure; cardiac dysrhythmias; myocardial infarction; hallucinations; seizures; possible death
Severe craving, severely depressed mood, exhaustion, prolonged sleep, apathy, irritability, disorientation
amphetamine (Benzedrine)
bath salts/khat/cathinone
benzphetamine (Didrex)
dextroamphetamine (Dexedrine)
methamphetamine (Desoxyn)
methylphenidate (Ritalin)
pemoline (Cylert)
phenmetrazine (Preludin)
Caffeine
Mood elevation, increased alertness, nervousness, jitteriness, irritability, insomnia, increased respirations, increased heart rate and force of myocardial contraction, relaxation of smooth muscle, diuresis
Rare: Nervousness, confusion, psychomotor agitation, anxiety, dizziness, tinnitus, muscle twitching, elevated blood pressure, tachycardia, extrasystole, increased respiratory rate
Headache, irritability, drowsiness, fatigue
Depressants
Alcohol
Initial relaxation, emotional lability, decreased inhibitions, drowsiness, lack of coordination, impaired judgment, slurred speech, hypotension, bradycardia, bradypnea, constricted pupils
Shallow respirations; cold, clammy skin; weak, rapid pulse; hyporeflexia; coma; possible death
Anxiety, agitation, insomnia, diaphoresis, tremors, delirium, seizures, possible death
Sedative Hypnotics
Barbiturates
secobarbital (Seconal)
pentobarbital (Nembutal)
amobarbital (Amytal)
Benzodiazepines
diazepam (Valium)
chlordiazepoxide (Librium)
alprazolam (Xanax)
Nonbarbiturates/Nonbenzodiazepines
methaqualone (Quaalude)
chloral hydrate (Noctec)
Opioids
Analgesia, euphoria, drowsiness, detachment from environment, relaxation, constricted pupils, constipation, nausea, decreased respiratory rate, slurred speech, impaired judgment, decreased sexual and aggressive drives
Slow, shallow respirations; clammy skin; constricted pupils; coma; possible death
Watery eyes, dilated pupils, runny nose, yawning, tremors, pain, chills, fever, diaphoresis, nausea, vomiting, diarrhea, abdominal cramps
heroin
morphine
opium
codeine
fentanyl (Sublimaze)
meperidine (Demerol)
hydromorphone (Dilaudid)
oxycodone (OxyContin, Percocet)
methadone (Dolophine)
Cannabis
Marijuana
Relaxation, euphoria, amotivation, slowed time sensation, sexual arousal, abrupt mood changes, impaired memory and attention, impaired judgment, reddened eyes, dry mouth, lack of coordination, tachycardia, increased appetite
Fatigue, paranoia, panic reactions, hallucinogen-like psychotic states
With heavy use: insomnia, restlessness, irritability, tremor, weight loss, hyperthermia, chills
Hashish
Synthetic Marijuana
Psychedelics
lysergic acid diethylamide (LSD)
psilocybin (mushrooms)
dimethyltryptamine (DMT)
diethyltryptamine (DET)
3,4-methylendioxyamphetamine
(MDMA, Ecstasy)
herbal ecstasy (contains herbs and ephedrine)
mescaline (peyote)
phencyclidine (PCP)
Perceptual distortions, hallucinations, delusions (PCP), depersonalization, heightened sensory perception, euphoria, mood swings, suspiciousness, panic, impaired judgment, increased body temperature, hypertension, flushed face, tremor, dilated pupils, constricted pupils (PCP), nystagmus (PCP), violence (PCP)
Prolonged effects and episodes, anxiety, panic, confusion, blurred vision, increases in blood pressure and temperature
No physical withdrawal, but psychological desire may occur
Inhalants
Aerosol Propellants
Euphoria; decreased inhibitions; giddiness; slurred speech; illusions; drowsiness; clouded sensorium; tinnitus; nystagmus; dysrhythmias; cough; nausea; vomiting; diarrhea; irritation to eyes, nose, and mouth
Anxiety, respiratory depression, cardiac dysrhythmias, loss of consciousness, sudden death
None
fluorinated hydrocarbons
nitrous oxide (in deodorants, hair spray, pesticide, whipped cream spray, spray paint, cookware coating products)
Solvents
gasoline, kerosene, nail polish remover, typewriter correction fluid, cleaning solutions, lighter fluid, paint, paint thinner, glue
Anesthetic Agents
nitrous oxide, chloroform
Nitrites
amyl nitrite, butyl nitrite
Treatment
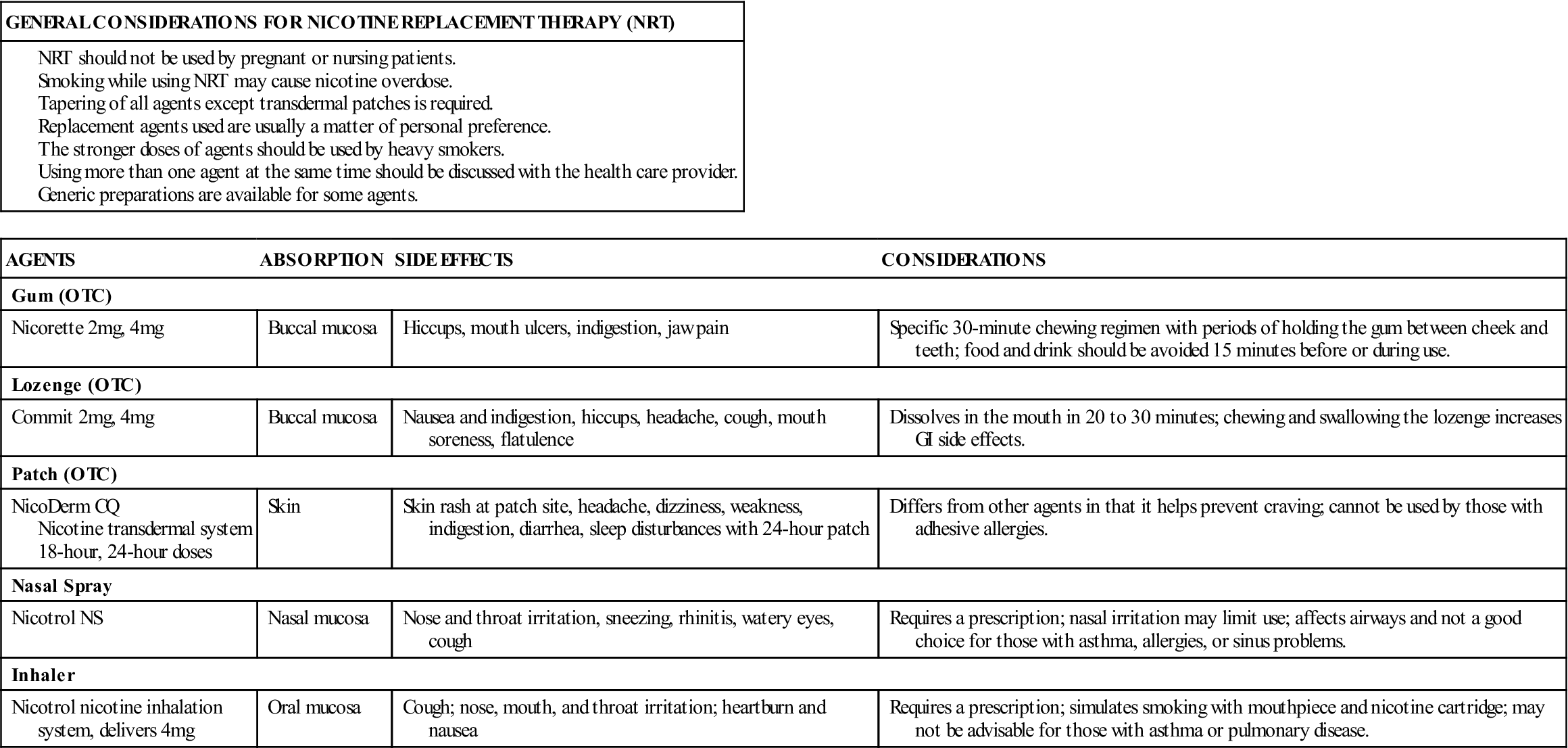
AGENTS
ABSORPTION
SIDE EFFECTS
CONSIDERATIONS
Gum (OTC)
Nicorette 2 mg, 4 mg
Buccal mucosa
Hiccups, mouth ulcers, indigestion, jaw pain
Specific 30-minute chewing regimen with periods of holding the gum between cheek and teeth; food and drink should be avoided 15 minutes before or during use.
Lozenge (OTC)
Commit 2 mg, 4 mg
Buccal mucosa
Nausea and indigestion, hiccups, headache, cough, mouth soreness, flatulence
Dissolves in the mouth in 20 to 30 minutes; chewing and swallowing the lozenge increases GI side effects.
Patch (OTC)
NicoDerm CQ
Nicotine transdermal system 18-hour, 24-hour doses
Skin
Skin rash at patch site, headache, dizziness, weakness, indigestion, diarrhea, sleep disturbances with 24-hour patch
Differs from other agents in that it helps prevent craving; cannot be used by those with adhesive allergies.
Nasal Spray
Nicotrol NS
Nasal mucosa
Nose and throat irritation, sneezing, rhinitis, watery eyes, cough
Requires a prescription; nasal irritation may limit use; affects airways and not a good choice for those with asthma, allergies, or sinus problems.
Inhaler
Nicotrol nicotine inhalation system, delivers 4 mg
Oral mucosa
Cough; nose, mouth, and throat irritation; heartburn and nausea
Requires a prescription; simulates smoking with mouthpiece and nicotine cartridge; may not be advisable for those with asthma or pulmonary disease.
Cocaine
Pharmacokinetics
Pharmacodynamics
DRUG OF ABUSE
INTERACTING DRUGS/DRUG CATEGORIES
EFFECTS
Nicotine/Smoking*
isoproterenol (Isuprel)
phenylephrine (Neo-Synephrine)
pentazocine (Talwin NX)
propoxyphene (Darvon)
Benzodiazepines (diazepam [Valium])
Tricyclic antidepressants
propranolol (Inderal)
theophylline (Theo-Dur, others)
heparin
insulin
Increased effects with use of nicotine/smoking (After smoking cessation, dosages may need to be increased.)
Decreased effects with use of nicotine/smoking (After smoking cessation, dosages may need to be reduced.)
Cocaine
Sympathomimetics/adrenomimetics
Central nervous system (CNS) stimulants
Cholinesterase inhibitors (neostigmine)
May increase CNS and cardiac effects of cocaine
Tricyclic antidepressants, digoxin, methyldopa (Aldomet)
May increase cocaine-induced dysrhythmias
Beta-adrenergic blockers
Cocaine may decrease effects
Amphetamines
Tricyclic antidepressants
Sympathomimetics/adrenomimetics
CNS stimulants
Increased effect of tricyclic antidepressants and sympathomimetics; increased effect of amphetamines
GI antacids/urinary alkalinizing agents
Monoamine oxidase inhibitors (MAOIs)
Increased effect of amphetamine
meperidine (Demerol)
Amphetamines increase analgesic effect; meperidine increases risk of seizures and vascular collapse.
Thyroid hormone
Adrenergic blockers
Antihistamines
Antihypertensives
Reciprocal increase in effects
Amphetamines may decrease effects.
Alcohol
Other CNS depressants:
Increased CNS depression with increased risk of death from respiratory depression
Sedative-hypnotics
Opioids
General anesthetics
Nonsteroidal antiinflammatory drugs
Combined effect increases risk of gastric bleeding
acetaminophen (Tylenol)
Increased risk for liver injury
Antihypertensives
Decreased effect of antihypertensives
Barbiturates
Other CNS depressants:
Increased CNS depression
Alcohol
Opioids
General anesthetics
Other sedative/hypnotics
MAOIs
valproic acid (Depakene)
Oral anticoagulants
Corticosteroids and other steroid hormones
griseofulvin (Fluvicin)
doxycycline
Effect decreased by barbiturates
Benzodiazepines
Other CNS depressants:
Increased CNS depression
Alcohol
Opioids
General anesthetics
Other sedative/hypnotics
Herbs:
Kava kava, valerian
Opioids
Other CNS depressants:
Increased CNS depression
Alcohol
General anesthetics
Sedative/hypnotics
Phenothiazines
Antiemetics
Mixed agonist/antagonist opioids
Reduces the effect of pure opioid agonists and may precipitate withdrawal syndrome
MAOIs
May cause severe fatal reaction
Diuretics
Opioids may decrease effect
Marijuana/Hashish
CNS stimulants/sympathomimetics
Anticholinergic agents
Tricyclic antidepressants
Additive hypertension, tachycardia, drowsiness
CNS depressants
Additive drowsiness and CNS depression
theophylline
Decreased effect of theophylline ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs of Abuse
Get Clinical Tree app for offline access
