Drugs for Urinary Tract Disorders
Objectives
• Compare the groups of drugs that are urinary antiseptics and antiinfectives.
• Describe the side effects and adverse reactions to urinary antiseptics and antiinfectives.
• Differentiate the uses for a urinary analgesic, a urinary stimulant, and a urinary antispasmodic.
Key Terms
acute cystitis, p. 460
acute pyelonephritis, p. 461
antimuscarinics, p. 465
antispasmodics, p. 465
bactericidal, p. 460
bacteriostatic, p. 460
micturition, p. 463
urinary analgesic, p. 460
urinary antiseptics/antiinfectives, p. 460
urinary stimulant, p. 460
urinary tract infection, p. 460
The largest number of urinary tract disorders are caused by urinary tract infections (UTIs), microbial infections of any part of the urinary tract. UTIs may result from an upper UTI, such as pyelonephritis, or a lower UTI, such as cystitis, urethritis, or prostatitis. A group of drugs called urinary antiseptics/antiinfectives prevents bacterial growth in the kidneys and bladder, but is not effective for systemic infections. Urinary antiseptics/antiinfectives have a bacteriostatic (inhibit bacterial growth) effect when given in lower dosages. They also have a bactericidal (kill bacteria) effect when given in higher dosages.
Urinary antiseptics/antiinfectives, urinary analgesics (relieve pain and burning in the urinary tract), urinary stimulants (agents that increase muscle tone of urinary muscles), and urinary antispasmodics/antimuscarinics are presented in this chapter. Chapters 29, 30, and 31 present further discussions of antibiotics, fluoroquinolones, and sulfonamides used to treat UTIs. Diuretics are discussed in Chapter 43.
Acute cystitis, a lower UTI, frequently occurs in female patients because of their shorter urethra. It is more common in women of childbearing age, older women, and young girls. Acute cystitis is commonly caused by Escherichia coli. Other bacterial causes include the gram-positive Staphylococcus saprophyticus and gram-negative Klebsiella, Proteus, and Pseudomonas. Symptoms of cystitis include pain and burning on urination and urinary frequency and urgency. A urine culture is usually obtained before the start of any antiinfective/antibiotic drug therapy. In male patients, a lower UTI is most likely prostatitis with symptoms similar to cystitis.
Acute pyelonephritis, an upper UTI, is commonly seen in women of childbearing age, older women, and young girls. E. coli is the most common organism causing pyelonephritis. Symptoms include chills, high fever, flank pain, pain during urination, urinary frequency and urgency, and pyuria. The bacterial count in the urine is greater than 100,000 bacteria/mL. In severe cases, the patient may be hospitalized and receive intravenous (IV) antibiotics (e.g., an aminoglycoside, ticarcillin/clavulanic acid, or piperacillin/tazobactam).
The most commonly used agents for treating UTIs are nitrofurantoin (Macrodantin); trimethoprim-sulfamethoxazole (Bactrim, Septra); and fluoroquinolones such as nalidixic acid (NegGram), norfloxacin (Noroxin), and ciprofloxacin (Cipro). Treatment may consist of a single double-strength dose of the chosen drug, a 3-day course, or the traditional method of 7 to 14 days of drug dosing. Fosfomycin tromethamine (Monurol), a nitrofurantoin prototype drug, is effective for UTIs as a single-dose treatment. Other agents used to treat UTIs include oral amoxicillin/clavulanic acid (Augmentin) and oral third-generation cephalosporins (cefixime, cefpodoxime proxetil, or ceftibuten). With severe UTIs, IV drug therapy followed by oral drug therapy is usually recommended.
Urinary Antiseptics/Antiinfectives and Antibiotics
Urinary antiseptics/antiinfectives are limited to the treatment of UTIs. Drug action occurs in the renal tubule and bladder, where it is effective in reducing bacterial growth. A urinalysis, as well as a culture and sensitivity test, is usually performed before the initiation of drug therapy. The groups of urinary antiseptics/antiinfectives are nitrofurantoin, methenamine, trimethoprim, and the fluoroquinolones.
Nitrofurantoin
Nitrofurantoin (Macrodantin) was first prescribed to treat UTIs in 1953. Nitrofurantoin is bacteriostatic or bactericidal, depending on the drug dosage, and is effective against many gram-positive and gram-negative organisms, especially E. coli. It is used to treat acute and chronic UTIs. The drug data for nitrofurantoin are given in Prototype Drug Chart 34-1.
Pharmacokinetics
Nitrofurantoin is well absorbed from the gastrointestinal (GI) tract. The drug is usually taken with food to decrease GI distress. Decreased absorption occurs when the drug is taken with antacids. Nitrofurantoin is moderately protein-bound. With normal renal function, the drug is rapidly eliminated because of its short half-life of 20 minutes; however, it accumulates in the serum with urinary dysfunction.
Pharmacodynamics
When nitrofurantoin is given in low doses for prophylactic use, the drug has a bacteriostatic effect. High concentration of nitrofurantoin causes a bactericidal effect. Nitrofurantoin is effective against many gram-positive and gram-negative organisms such as E. coli, Neisseria, streptococci, Staphylococcus aureus, and others. It is not as effective against Pseudomonas aeruginosa, Proteus species, and some species of Klebsiella. The onset and duration of action are unknown. Peak action occurs 30 minutes after absorption. If sudden onset of dyspnea, chest pain, cough, fever, and chills develops, the patient should contact the health care provider. Symptoms resolve after discontinuing the drug.
The nursing process for nitrofurantoin is applicable to the other urinary antiseptics/antiinfectives.
Methenamine
Methenamine (Hiprex) produces a bactericidal effect when the urine pH is less than 5.5. Methenamine is available as hippurate salt. It is effective against gram-positive and gram-negative organisms, especially E. coli and P. aeruginosa. It is used for chronic UTIs. Methenamine should not be taken with sulfonamides, because crystalluria is likely to occur. It is absorbed readily from the GI tract, and approximately 90% of the drug is excreted in the urine unchanged. Methenamine forms ammonia and formaldehyde in acid urine; therefore the urine needs to be acidified to exert a bactericidal action. Cranberry juice (several 8-ounce glasses per day), ascorbic acid, and ammonium chloride can be taken to decrease the urine pH.
 : 20 min
: 20 min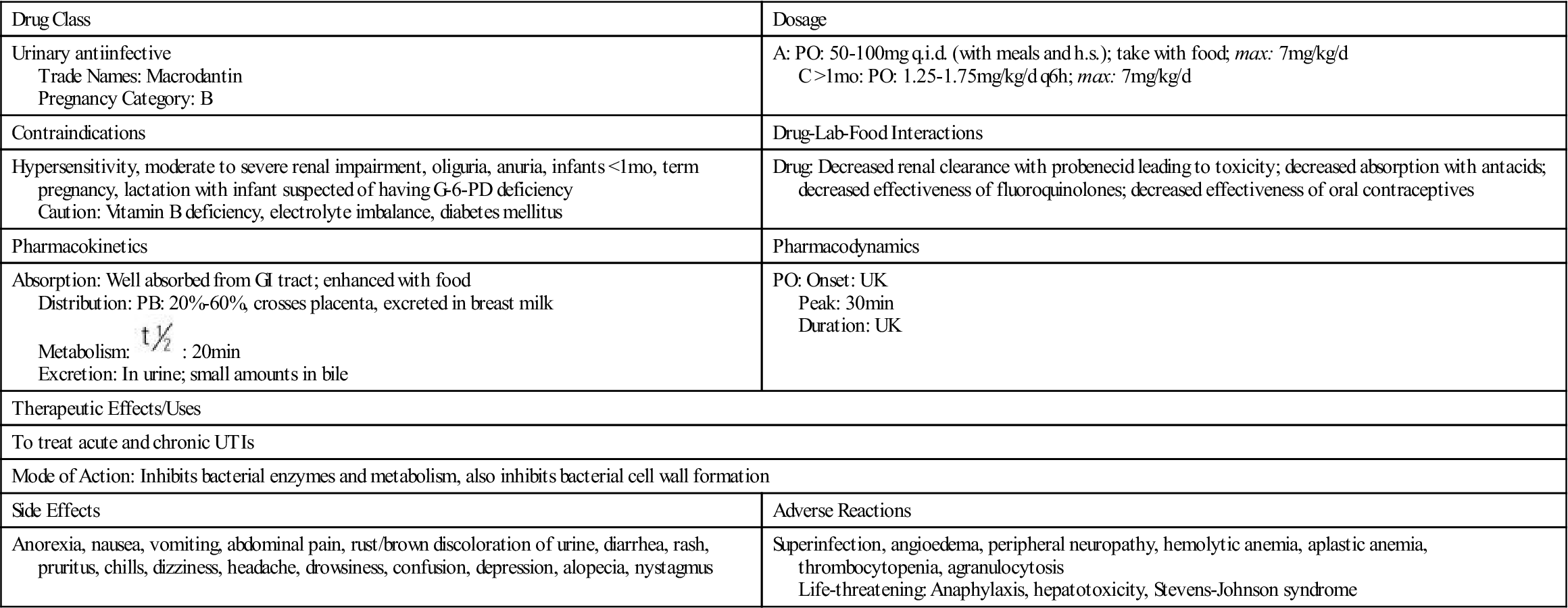
 , half-life; UK, unknown; UTI, urinary tract infection; y, year; <, less than.
, half-life; UK, unknown; UTI, urinary tract infection; y, year; <, less than.










