Drugs for Upper Respiratory Disorders
Objectives
• Compare antihistamine, decongestant, antitussive, and expectorant drug groups.
• Differentiate between rhinitis, sinusitis, and pharyngitis.
• Describe the side effects of nasal decongestants and how they can be avoided.
• Apply the nursing process for drugs used to treat the common cold.
Key Terms
acute pharyngitis, p. 581
acute rhinitis, p. 573
allergic rhinitis, p. 574
antihistamines, p. 574
antitussives, p. 578
common cold, p. 573
decongestants, p. 574
expectorants, p. 578
rebound nasal congestion, p. 575
rhinorrhea, p. 574
sinusitis, p. 581
Upper respiratory infections (URIs) include the common cold, acute rhinitis, sinusitis, and acute pharyngitis. The common cold is the most prevalent type of URI. Adults have an average of 2 to 4 colds per year, and children have an average of 4 to 12 colds per year. Incidence is seasonally variable, with approximately 50% of the population experiencing a winter cold and 25% experiencing a summer cold. A cold is not considered a life-threatening illness, but, it causes physical and mental discomfort and loss of time at work and school. The common cold is an expensive illness in the United States—more than $40 billion is spent each year on over-the-counter (OTC) cold and cough preparations.
Common Cold, Acute Rhinitis, and Allergic Rhinitis
The common cold is caused by the rhinovirus and affects primarily the nasopharyngeal tract. Acute rhinitis (acute inflammation of the mucous membranes of the nose) usually accompanies the common cold. Acute rhinitis is not the same as allergic rhinitis, often called hay fever, which is caused by pollen or a foreign substance (e.g., animal dander). Nasal secretions increase in both acute rhinitis and allergic rhinitis.
A cold is most contagious 1 to 4 days before the onset of symptoms (the incubation period) and during the first 3 days of the cold. Transmission occurs more frequently from touching contaminated surfaces and then touching the nose or mouth than it does from viral droplets released by sneezing.
The groups of drugs used to manage cold symptoms include antihistamines (H1 blockers), decongestants (sympathomimetic amines), antitussives, and expectorants. These drugs can be used singly or in combination preparations.
Symptoms of the common cold include rhinorrhea (watery nasal discharge), nasal congestion, cough, and increased mucosal secretions. If a bacterial infection secondary to the cold occurs, infectious rhinitis may result, and nasal discharge becomes tenacious, mucoid, and yellow or yellow-green. The nasal secretions are discolored by white blood cells and cellular debris that are by-products of the fight against the bacterial infection. Antibiotics used to treat bacterial respiratory infections are discussed in Chapters 29, 30, and 31.
Antihistamines
Antihistamines, H1 blockers or H1 antagonists, compete with histamine for receptor sites, preventing a histamine response. The two types of histamine receptors, H1 and H2, cause different responses. When the H1 receptor is stimulated, the extravascular smooth muscles, including those lining the nasal cavity, are constricted. With stimulation of the H2 receptor, an increase in gastric secretions occurs, which is a cause of peptic ulcer (see Chapter 48). These two types of histamine receptors should not be confused. Antihistamines decrease nasopharyngeal secretions by blocking the H1 receptor.
Although antihistamines are commonly used as cold remedies, these agents can also treat allergic rhinitis. However, the antihistamines are not useful in an emergency situation such as anaphylaxis. Most antihistamines are rapidly absorbed in 15 minutes, but they are not potent enough to combat anaphylaxis.
First-Generation Antihistamines
The antihistamine group can be divided into first and second generations. Most first-generation antihistamines cause drowsiness, dry mouth, and other anticholinergic symptoms, whereas second-generation antihistamines have fewer anticholinergic effects and a lower incidence of drowsiness. Many OTC cold remedies contain a first-generation antihistamine, which can cause drowsiness; therefore patients should be alerted not to drive or operate dangerous machinery when taking such medications. The anticholinergic properties of most antihistamines cause dryness of the mouth and decreased secretions, making them useful in treating rhinitis caused by the common cold. Antihistamines also decrease the nasal itching and tickling that cause sneezing.
The first-generation antihistamine diphenhydramine (Benadryl) has been available for years and is frequently combined with other ingredients in cold remedy preparations. Its primary use is to treat rhinitis. Prototype Drug Chart 40-1 lists the pharmacologic behavior of diphenhydramine.
Pharmacokinetics
Diphenhydramine can be administered orally, intramuscularly (IM), or intravenously (IV). It is well absorbed from the gastrointestinal (GI) tract, but systemic absorption from topical use is minimal. It is highly protein-bound (98%) and has an average half-life of 2 to 7 hours. Diphenhydramine is metabolized by the liver and excreted as metabolites in the urine.
Pharmacodynamics
Diphenhydramine blocks the effects of histamine by competing for and occupying H1 receptor sites. It has anticholinergic effects and should not be used by patients with narrow-angle glaucoma. Drowsiness is a major side effect of the drug; in fact, it is sometimes used in sleep-aid products. Diphenhydramine is also used as an antitussive (i.e., it alleviates cough). Its onset of action can occur in as few as 15 minutes when taken orally and IM. IV administration results in an immediate onset of action. The duration of action is 4 to 6 hours.
Diphenhydramine can cause CNS depression if taken with alcohol, narcotics, hypnotics, or barbiturates.
Side Effects of Most First-Generation Antihistamines.
The most common side effects of first-generation antihistamines are drowsiness, dizziness, fatigue, and disturbed coordination. Skin rashes and anticholinergic symptoms (e.g., dry mouth, urine retention, blurred vision, wheezing) may also occur.
Second-Generation Antihistamines
The second-generation antihistamines are frequently called nonsedating antihistamines because they have little to no effect on sedation. In addition, these antihistamines cause fewer anticholinergic symptoms. Although a moderate amount of alcohol and other central nervous system (CNS) depressants may be taken with second-generation antihistamines, many clinicians advise against such use.
The second-generation antihistamines cetirizine (Zyrtec), fexofenadine (Allegra), and loratadine (Claritin) have half-lives between 7 and 15 hours. Azelastine (Astelin) is a second-generation antihistamine that has a half-life of 22 hours and is administered by nasal spray. Table 40-1 lists the first- and second-generation antihistamines used to treat allergic rhinitis.
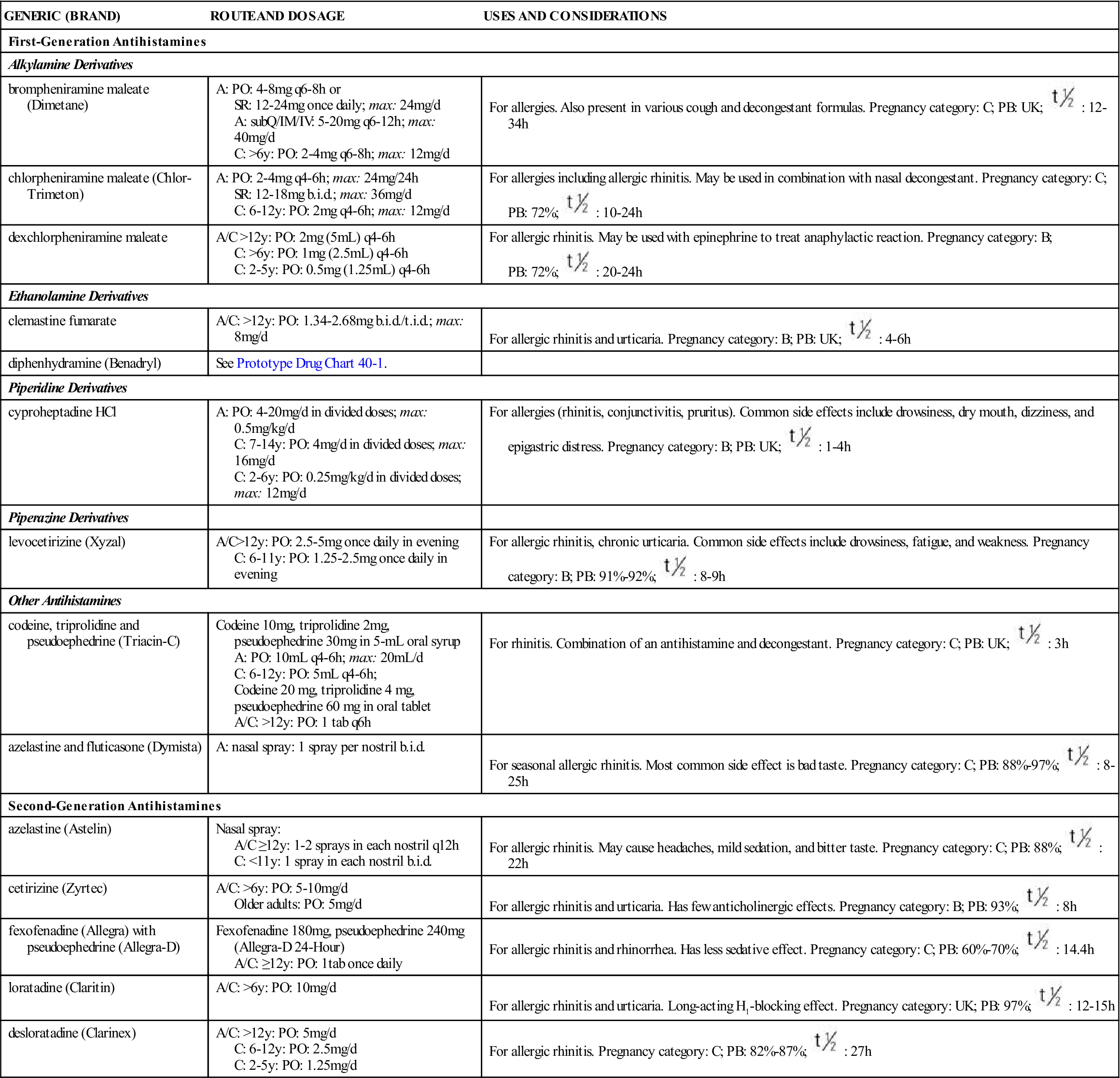
TABLE 40-1
ANTIHISTAMINES FOR TREATMENT OF ALLERGIC RHINITIS
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| First-Generation Antihistamines | ||
| Alkylamine Derivatives | ||
| brompheniramine maleate (Dimetane) | A: PO: 4-8 mg q6-8h or SR: 12-24 mg once daily; max: 24 mg/d A: subQ/IM/IV: 5-20 mg q6-12h; max: 40 mg/d C: >6 y: PO: 2-4 mg q6-8h; max: 12 mg/d | For allergies. Also present in various cough and decongestant formulas. Pregnancy category: C; PB: UK;  : 12-34 h : 12-34 h |
| chlorpheniramine maleate (Chlor-Trimeton) | A: PO: 2-4 mg q4-6h; max: 24 mg/24 h SR: 12-18 mg b.i.d.; max: 36 mg/d C: 6-12 y: PO: 2 mg q4-6h; max: 12 mg/d | For allergies including allergic rhinitis. May be used in combination with nasal decongestant. Pregnancy category: C; PB: 72%;  : 10-24 h : 10-24 h |
| dexchlorpheniramine maleate | A/C >12 y: PO: 2 mg (5 mL) q4-6h C: >6 y: PO: 1 mg (2.5 mL) q4-6h C: 2-5 y: PO: 0.5 mg (1.25 mL) q4-6h | For allergic rhinitis. May be used with epinephrine to treat anaphylactic reaction. Pregnancy category: B; PB: 72%;  : 20-24 h : 20-24 h |
| Ethanolamine Derivatives | ||
| clemastine fumarate | A/C: >12 y: PO: 1.34-2.68 mg b.i.d./t.i.d.; max: 8 mg/d | For allergic rhinitis and urticaria. Pregnancy category: B; PB: UK;  : 4-6 h : 4-6 h |
| diphenhydramine (Benadryl) | See Prototype Drug Chart 40-1. | |
| Piperidine Derivatives | ||
| cyproheptadine HCl | A: PO: 4-20 mg/d in divided doses; max: 0.5 mg/kg/d C: 7-14 y: PO: 4 mg/d in divided doses; max: 16 mg/d C: 2-6 y: PO: 0.25 mg/kg/d in divided doses; max: 12 mg/d | For allergies (rhinitis, conjunctivitis, pruritus). Common side effects include drowsiness, dry mouth, dizziness, and epigastric distress. Pregnancy category: B; PB: UK;  : 1-4 h : 1-4 h |
| Piperazine Derivatives | ||
| levocetirizine (Xyzal) | A/C>12 y: PO: 2.5-5 mg once daily in evening C: 6-11 y: PO: 1.25-2.5 mg once daily in evening | For allergic rhinitis, chronic urticaria. Common side effects include drowsiness, fatigue, and weakness. Pregnancy category: B; PB: 91%-92%;  : 8-9 h : 8-9 h |
| Other Antihistamines | ||
| codeine, triprolidine and pseudoephedrine (Triacin-C) | Codeine 10 mg, triprolidine 2 mg, pseudoephedrine 30 mg in 5-mL oral syrup A: PO: 10 mL q4-6h; max: 20 mL/d C: 6-12 y: PO: 5 mL q4-6h; Codeine 20 mg, triprolidine 4 mg, pseudoephedrine 60 mg in oral tablet A/C: >12y: PO: 1 tab q6h | For rhinitis. Combination of an antihistamine and decongestant. Pregnancy category: C; PB: UK;  : 3 h : 3 h |
| azelastine and fluticasone (Dymista) | A: nasal spray: 1 spray per nostril b.i.d. | For seasonal allergic rhinitis. Most common side effect is bad taste. Pregnancy category: C; PB: 88%-97%;  : 8-25 h : 8-25 h |
| Second-Generation Antihistamines | ||
| azelastine (Astelin) | Nasal spray: A/C ≥12 y: 1-2 sprays in each nostril q12h C: <11 y: 1 spray in each nostril b.i.d. | For allergic rhinitis. May cause headaches, mild sedation, and bitter taste. Pregnancy category: C; PB: 88%;  : 22 h : 22 h |
| cetirizine (Zyrtec) | A/C: >6 y: PO: 5-10 mg/d Older adults: PO: 5 mg/d | For allergic rhinitis and urticaria. Has few anticholinergic effects. Pregnancy category: B; PB: 93%;  : 8 h : 8 h |
| fexofenadine (Allegra) with pseudoephedrine (Allegra-D) | Fexofenadine 180 mg, pseudoephedrine 240 mg (Allegra-D 24-Hour) A/C: ≥12 y: PO: 1 tab once daily | For allergic rhinitis and rhinorrhea. Has less sedative effect. Pregnancy category: C; PB: 60%-70%;  : 14.4 h : 14.4 h |
| loratadine (Claritin) | A/C: >6 y: PO: 10 mg/d | For allergic rhinitis and urticaria. Long-acting H1-blocking effect. Pregnancy category: UK; PB: 97%;  : 12-15 h : 12-15 h |
| desloratadine (Clarinex) | A/C: >12 y: PO: 5 mg/d C: 6-12 y: PO: 2.5 mg/d C: 2-5 y: PO: 1.25 mg/d | For allergic rhinitis. Pregnancy category: C; PB: 82%-87%;  : 27 h : 27 h |
Nasal and Systemic Decongestants
Nasal congestion results from dilation of nasal blood vessels caused by infection, inflammation, or allergy. With this dilation, there is a transudation of fluid into the tissue spaces, resulting in swelling of the nasal cavity. Nasal decongestants (sympathomimetic amines) stimulate the alpha-adrenergic receptors, producing vascular constriction (vasoconstriction) of the capillaries within the nasal mucosa. The result is shrinking of the nasal mucous membranes and a reduction in fluid secretion (runny nose).
Nasal decongestants are administered by nasal spray or drops or in tablet, capsule, or liquid form. Frequent use of decongestants, especially nasal spray or drops, can result in tolerance and rebound nasal congestion (rebound vasodilation instead of vasoconstriction). Rebound nasal congestion is caused by irritation of the nasal mucosa.
 : 2-7 h
: 2-7 h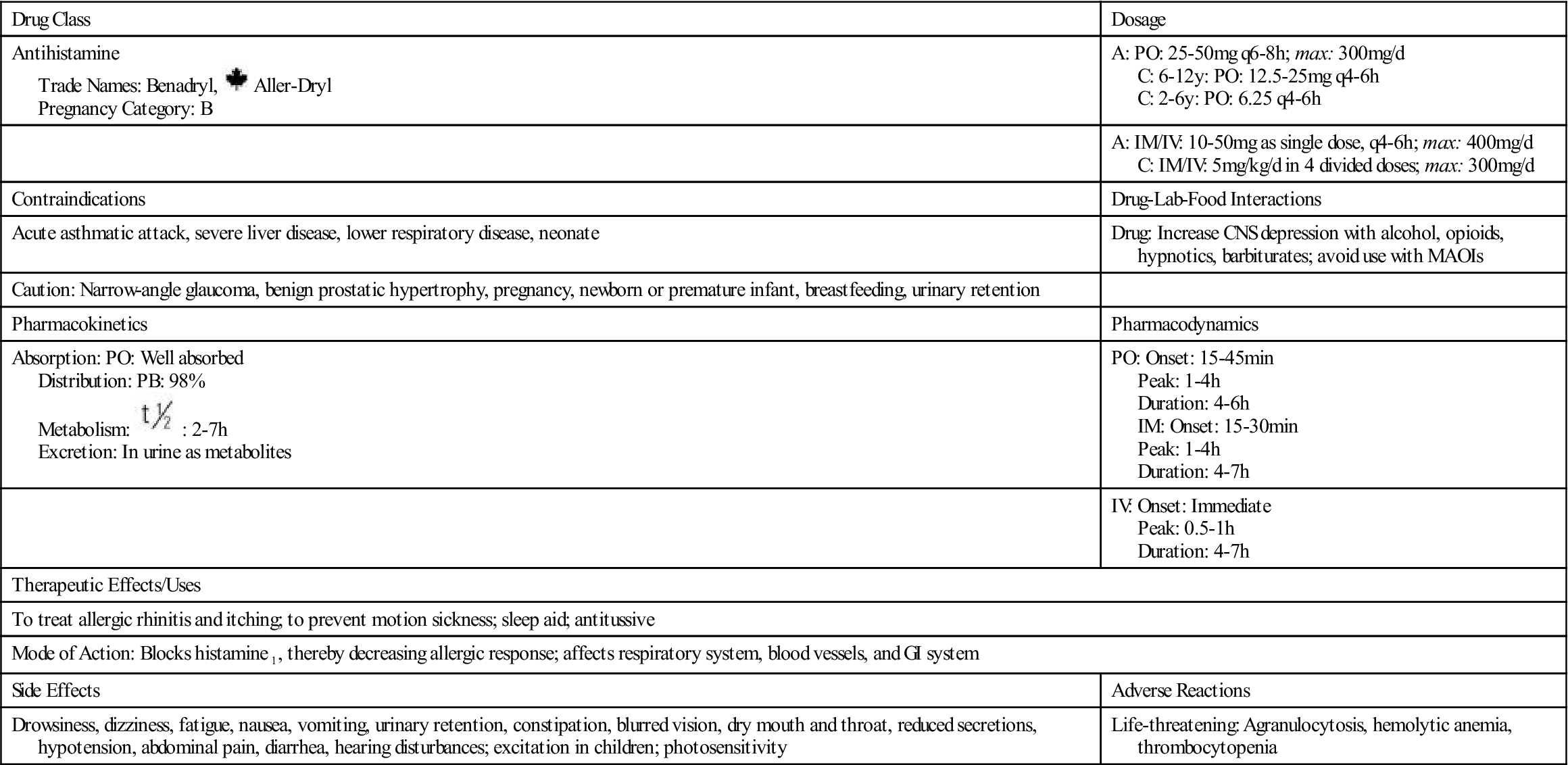
 , half-life;
, half-life;  , half-life; tab, tablet; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than.
, half-life; tab, tablet; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than.








