Drugs for Gastrointestinal Tract Disorders
Objectives
• Compare the pharmacologic treatment of vomiting, diarrhea, and constipation.
• Differentiate the actions and side effects of antiemetics, emetics, antidiarrheals, and laxatives.
• Apply the nursing process for the patient taking antiemetics, antidiarrheals, and laxatives.
• Differentiate contraindications to the use of antiemetics, emetics, antidiarrheals, and laxatives.
Key Terms
adsorbents, p. 684
antidiarrheals, p. 683
antiemetics, p. 677
cannabinoids, p. 681
cathartics, p. 686
chemoreceptor trigger zone, p. 677
constipation, p. 685
diarrhea, p. 683
emetics, p. 682
emollients, p. 689
laxatives, p. 686
opiates, p. 683
osmotics, p. 686
purgatives, p. 686
selective chloride channel activators, p. 689
vomiting center, p. 677
Drug groups used to correct or control vomiting, diarrhea, and constipation are antiemetics, emetics, antidiarrheals, and laxatives. Each of these drug groups is discussed separately. Drugs used to treat peptic ulcers are discussed in Chapter 48.
Vomiting
Vomiting (emesis), the expulsion of gastric contents, has a multitude of causes, including motion sickness, viral and bacterial infection, food intolerance, surgery, pregnancy, pain, shock, effects of selected drugs (e.g., antineoplastics), radiation, and disturbances of the middle ear that affect equilibrium. Nausea, a queasy sensation, may or may not precede the expulsion. The cause of the vomiting must be identified. Antiemetics can mask the underlying cause of vomiting and should not be used until the cause has been determined, unless the vomiting is so severe as to cause dehydration and electrolyte imbalance.
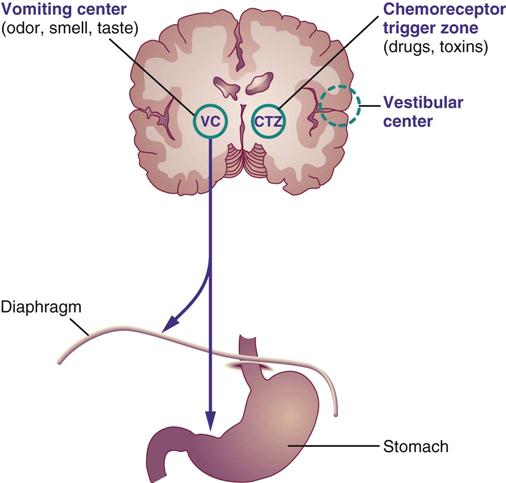
Two major cerebral centers—the chemoreceptor trigger zone (CTZ), which lies near the medulla, and the vomiting center in the medulla—cause vomiting when stimulated (Figure 47-1). The CTZ receives most of the impulses from drugs, toxins, and the vestibular center in the ear and transmits them to the vomiting center. The neurotransmitter dopamine stimulates the CTZ, which in turn stimulates the vomiting center. Levodopa, a drug with dopamine-like properties, can cause vomiting by stimulating the CTZ. Some sensory impulses, such as odor, smell, taste, and gastric mucosal irritation, are transmitted directly to the vomiting center. The neurotransmitter acetylcholine is also a vomiting stimulant. When the vomiting center is stimulated, the motor neuron responds by causing contraction of the diaphragm, the anterior abdominal muscles, and the stomach. The glottis closes, the abdominal wall moves upward, and vomiting occurs.
Nonpharmacologic measures should be used first when nausea and vomiting occur. If the nonpharmacologic measures are not effective, antiemetics are combined with nonpharmacologic measures. The two major groups of antiemetics are nonprescription (antihistamines, bismuth subsalicylate, and phosphorated carbohydrate solution) and prescription (antihistamines, dopamine antagonists, benzodiazepines, serotonin antagonists, glucocorticoids, cannabinoids, and miscellaneous antiemetics).
Nonpharmacologic Measures
The nonpharmacologic methods of decreasing nausea and vomiting include administration of weak tea, flat soda, gelatin, Gatorade, and Pedialyte (for use in children). Crackers and dry toast may be helpful. When dehydration becomes severe, intravenous (IV) fluids are needed to restore body fluid balance.
Nonprescription Antiemetics
Nonprescription antiemetics (antivomiting agents) can be purchased as over-the-counter (OTC) drugs. These drugs are frequently used to prevent motion sickness but have minimal effect on controlling severe vomiting resulting from anticancer agents (antineoplastics), radiation, and toxins. To prevent motion sickness, the antiemetic should be taken 30 minutes before travel. These drugs are not effective in relieving motion sickness if taken after vomiting has occurred.
Selected antihistamine antiemetics, such as dimenhydrinate (Dramamine), cyclizine hydrochloride (Marezine), meclizine hydrochloride (Antivert), and diphenhydramine hydrochloride (Benadryl) can be purchased OTC to prevent nausea, vomiting, and dizziness (vertigo) caused by motion. These drugs inhibit vestibular stimulation in the middle ear. Benadryl is also used to prevent or alleviate allergic reactions to drugs, insects, and food by acting as an antagonist to histamine1 (H1) receptors.
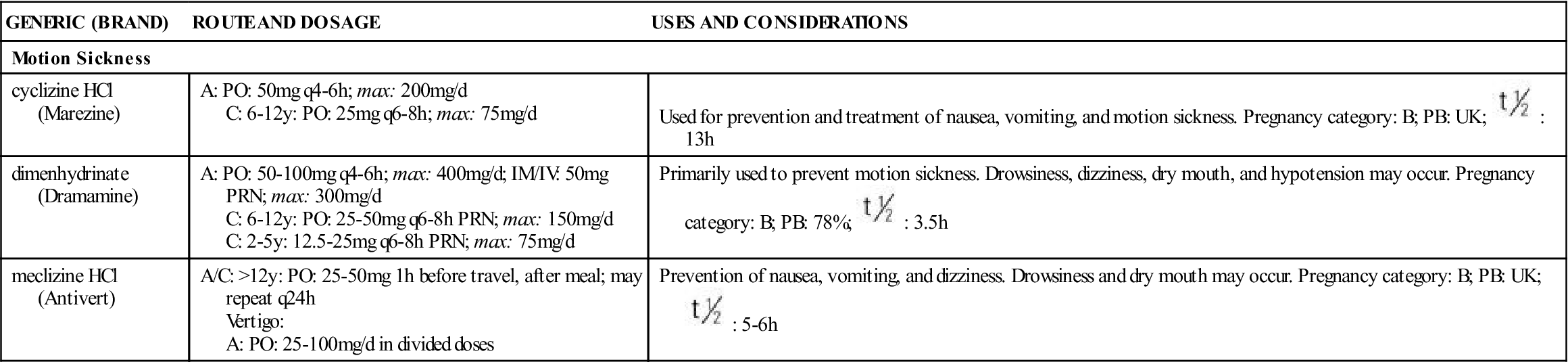
The side effects of antihistamine antiemetics are similar to those of anticholinergics: drowsiness, dryness of the mouth, and constipation. Table 47-1 lists the nonprescription antiemetics used for vomiting caused by motion sickness.
TABLE 47-1
NONPRESCRIPTION ANTIEMETICS: ANTIHISTAMINE
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Motion Sickness | ||
| cyclizine HCl (Marezine) | A: PO: 50 mg q4-6 h; max: 200 mg/d C: 6-12 y: PO: 25 mg q6-8h; max: 75 mg/d | Used for prevention and treatment of nausea, vomiting, and motion sickness. Pregnancy category: B; PB: UK;  : 13 h : 13 h |
| dimenhydrinate (Dramamine) | A: PO: 50-100 mg q4-6h; max: 400 mg/d; IM/IV: 50 mg PRN; max: 300 mg/d C: 6-12 y: PO: 25-50 mg q6-8h PRN; max: 150 mg/d C: 2-5 y: 12.5-25 mg q6-8h PRN; max: 75 mg/d | Primarily used to prevent motion sickness. Drowsiness, dizziness, dry mouth, and hypotension may occur. Pregnancy category: B; PB: 78%;  : 3.5 h : 3.5 h |
| meclizine HCl (Antivert) | A/C: >12 y: PO: 25-50 mg 1 h before travel, after meal; may repeat q24h Vertigo: A: PO: 25-100 mg/d in divided doses | Prevention of nausea, vomiting, and dizziness. Drowsiness and dry mouth may occur. Pregnancy category: B; PB: UK;  : 5-6 h : 5-6 h |
Several nonprescription drugs such as bismuth subsalicylate (Pepto-Bismol) act directly on the gastric mucosa to suppress vomiting. They are marketed in liquid and chewable tablet forms and can be taken for gastric discomfort or diarrhea. Phosphorated carbohydrate solution (Emetrol), a hyperosmolar carbohydrate, decreases nausea and vomiting by changing the gastric pH; it may also decrease smooth-muscle contraction of the stomach. Its effectiveness as an antiemetic has not been verified. Patients with diabetes mellitus should avoid this drug because of its high sugar content.
Antiemetics were once frequently used for the treatment of nausea and vomiting during the first trimester of pregnancy, but they are no longer recommended because they may cause harm to the fetus. Instead, nonpharmacologic methods should be used to alleviate nausea and vomiting during pregnancy, and OTC antiemetics should be avoided. If vomiting becomes severe and threatens the well-being of the mother and fetus, an antiemetic such as trimethobenzamide (Tigan) can be administered, although this drug is classified as pregnancy category C. Other antiemetics may be prescribed cautiously.
Prescription Antiemetics
Common prescription antiemetics are classified into the following groups: (1) antihistamines, (2) anticholinergics, (3) dopamine antagonists, (4) benzodiazepines, (5) serotonin antagonists, (6) glucocorticoids, (7) cannabinoids (for patients with cancer), and (8) miscellaneous. Many of these drugs act as antagonists to dopamine, histamine, serotonin, and acetylcholine, which are associated with vomiting. Antihistamines and anticholinergics act primarily on the vomiting center; they also act by decreasing stimulation of the CTZ and vestibular pathways. The cannabinoids act on the cerebral cortex. Phenothiazines, the miscellaneous antiemetics (e.g., metoclopramide), and trimethobenzamide act on the CTZ center. Drug combination therapy is commonly used to manage chemotherapy-induced nausea and vomiting. Lorazepam (Ativan), glucocorticoids, and serotonin (5-HT3) receptor antagonists are quite effective in combination therapy. Lorazepam, haloperidol, and glucocorticoids are not approved by the U.S. Food and Drug Administration (FDA) as antiemetics but are extremely effective when combined for this unlabeled use.
Antihistamines and Anticholinergics
Only a few prescription antihistamines and anticholinergics are used in the treatment of nausea and vomiting. Table 47-2 lists these drugs and their dosages, uses, and considerations.
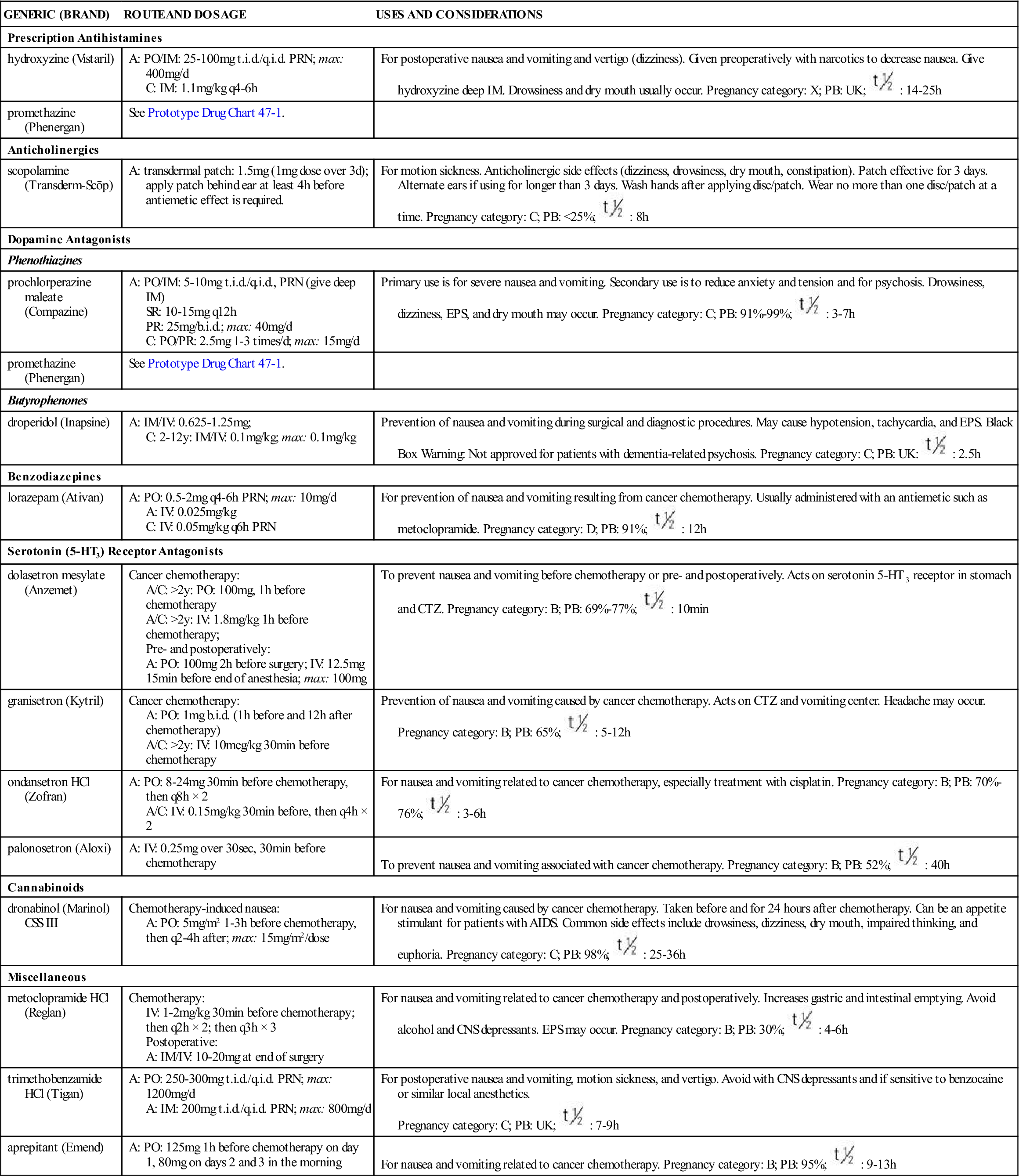
TABLE 47-2
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Prescription Antihistamines | ||
| hydroxyzine (Vistaril) | A: PO/IM: 25-100 mg t.i.d./q.i.d. PRN; max: 400 mg/d C: IM: 1.1 mg/kg q4-6h | For postoperative nausea and vomiting and vertigo (dizziness). Given preoperatively with narcotics to decrease nausea. Give hydroxyzine deep IM. Drowsiness and dry mouth usually occur. Pregnancy category: X; PB: UK;  : 14-25 h : 14-25 h |
| promethazine (Phenergan) | See Prototype Drug Chart 47-1. | |
| Anticholinergics | ||
| scopolamine (Transderm-Scōp) | A: transdermal patch: 1.5 mg (1 mg dose over 3 d); apply patch behind ear at least 4 h before antiemetic effect is required. | For motion sickness. Anticholinergic side effects (dizziness, drowsiness, dry mouth, constipation). Patch effective for 3 days. Alternate ears if using for longer than 3 days. Wash hands after applying disc/patch. Wear no more than one disc/patch at a time. Pregnancy category: C; PB: <25%;  : 8 h : 8 h |
| Dopamine Antagonists | ||
| Phenothiazines | ||
| prochlorperazine maleate (Compazine) | A: PO/IM: 5-10 mg t.i.d./q.i.d., PRN (give deep IM) SR: 10-15 mg q12h PR: 25 mg/b.i.d.; max: 40 mg/d C: PO/PR: 2.5 mg 1-3 times/d; max: 15 mg/d | Primary use is for severe nausea and vomiting. Secondary use is to reduce anxiety and tension and for psychosis. Drowsiness, dizziness, EPS, and dry mouth may occur. Pregnancy category: C; PB: 91%-99%;  : 3-7 h : 3-7 h |
| promethazine (Phenergan) | See Prototype Drug Chart 47-1. | |
| Butyrophenones | ||
| droperidol (Inapsine) | A: IM/IV: 0.625-1.25 mg; C: 2-12 y: IM/IV: 0.1 mg/kg; max: 0.1 mg/kg | Prevention of nausea and vomiting during surgical and diagnostic procedures. May cause hypotension, tachycardia, and EPS. Black Box Warning: Not approved for patients with dementia-related psychosis. Pregnancy category: C; PB: UK:  : 2.5 h : 2.5 h |
| Benzodiazepines | ||
| lorazepam (Ativan) | A: PO: 0.5-2 mg q4-6h PRN; max: 10 mg/d A: IV: 0.025 mg/kg C: IV: 0.05 mg/kg q6h PRN | For prevention of nausea and vomiting resulting from cancer chemotherapy. Usually administered with an antiemetic such as metoclopramide. Pregnancy category: D; PB: 91%;  : 12 h : 12 h |
| Serotonin (5-HT3) Receptor Antagonists | ||
| dolasetron mesylate (Anzemet) | Cancer chemotherapy: A/C: >2 y: PO: 100 mg, 1 h before chemotherapy A/C: >2 y: IV: 1.8 mg/kg 1 h before chemotherapy; Pre- and postoperatively: A: PO: 100 mg 2 h before surgery; IV: 12.5 mg 15 min before end of anesthesia; max: 100 mg | To prevent nausea and vomiting before chemotherapy or pre- and postoperatively. Acts on serotonin 5-HT3 receptor in stomach and CTZ. Pregnancy category: B; PB: 69%-77%;  : 10 min : 10 min |
| granisetron (Kytril) | Cancer chemotherapy: A: PO: 1 mg b.i.d. (1 h before and 12 h after chemotherapy) A/C: >2 y: IV: 10 mcg/kg 30 min before chemotherapy | Prevention of nausea and vomiting caused by cancer chemotherapy. Acts on CTZ and vomiting center. Headache may occur. Pregnancy category: B; PB: 65%;  : 5-12 h : 5-12 h |
| ondansetron HCl (Zofran) | A: PO: 8-24 mg 30 min before chemotherapy, then q8h × 2 A/C: IV: 0.15 mg/kg 30 min before, then q4h × 2 | For nausea and vomiting related to cancer chemotherapy, especially treatment with cisplatin. Pregnancy category: B; PB: 70%-76%;  : 3-6 h : 3-6 h |
| palonosetron (Aloxi) | A: IV: 0.25 mg over 30 sec, 30 min before chemotherapy | To prevent nausea and vomiting associated with cancer chemotherapy. Pregnancy category: B; PB: 52%;  : 40 h : 40 h |
| Cannabinoids | ||
| dronabinol (Marinol) CSS III | Chemotherapy-induced nausea: A: PO: 5 mg/m2 1-3 h before chemotherapy, then q2-4h after; max: 15 mg/m2/dose | For nausea and vomiting caused by cancer chemotherapy. Taken before and for 24 hours after chemotherapy. Can be an appetite stimulant for patients with AIDS. Common side effects include drowsiness, dizziness, dry mouth, impaired thinking, and euphoria. Pregnancy category: C; PB: 98%;  : 25-36 h : 25-36 h |
| Miscellaneous | ||
| metoclopramide HCl (Reglan) | Chemotherapy: IV: 1-2 mg/kg 30 min before chemotherapy; then q2h × 2; then q3h × 3 Postoperative: A: IM/IV: 10-20 mg at end of surgery | For nausea and vomiting related to cancer chemotherapy and postoperatively. Increases gastric and intestinal emptying. Avoid alcohol and CNS depressants. EPS may occur. Pregnancy category: B; PB: 30%;  : 4-6 h : 4-6 h |
| trimethobenzamide HCl (Tigan) | A: PO: 250-300 mg t.i.d./q.i.d. PRN; max: 1200 mg/d A: IM: 200 mg t.i.d./q.i.d. PRN; max: 800 mg/d | For postoperative nausea and vomiting, motion sickness, and vertigo. Avoid with CNS depressants and if sensitive to benzocaine or similar local anesthetics. Pregnancy category: C; PB: UK;  : 7-9 h : 7-9 h |
| aprepitant (Emend) | A: PO: 125 mg 1 h before chemotherapy on day 1, 80 mg on days 2 and 3 in the morning | For nausea and vomiting related to cancer chemotherapy. Pregnancy category: B; PB: 95%;  : 9-13 h : 9-13 h |
Side Effects and Adverse Reactions.
Side effects include drowsiness, which can be a major problem, dry mouth, blurred vision caused by pupillary dilation, tachycardia (with anticholinergic use), and constipation. These drugs should not be used by patients with glaucoma.
Dopamine Antagonists
These agents suppress emesis by blocking dopamine2 receptors in the CTZ. The categories of dopamine antagonists include phenothiazines, butyrophenones, and benzodiazepines. Common side effects of dopamine antagonists are extrapyramidal symptoms (EPS), which are caused by blocking dopamine receptors, and hypotension. See Chapter 27 for a more detailed description of EPS and phenothiazines.
Phenothiazine Antiemetics
Selected piperazine phenothiazines are used to treat nausea and vomiting resulting from surgery, anesthetics, chemotherapy, and radiation sickness. They act by inhibiting the CTZ. When used in patients with cancer, these drugs are commonly given the night before treatment, the day of treatment, and for 24 hours after treatment. Not all phenothiazines are effective antiemetic agents. When prescribed for vomiting, the drug dosage is usually smaller than when used for psychiatric disorders.
Chlorpromazine (Thorazine) and prochlorperazine edisylate (Compazine) were the first phenothiazines used for both psychosis and vomiting. Promethazine (Phenergan), a phenothiazine introduced as an antihistamine in the 1940s, has a sedative effect and can also be used for motion sickness and management of nausea and vomiting. Promethazine is the most frequently prescribed antiemetic drug. Prototype Drug Chart 47-1 lists the pharmacologic data for promethazine.
Pharmacokinetics
Promethazine is readily absorbed in the gastrointestinal (GI) tract. It has 93% protein-binding capacity. Promethazine is metabolized by the liver and excreted in urine and feces.
Pharmacodynamics
Promethazine blocks H1-receptor sites on effector cells and impedes histamine-mediated responses. The onset of action of oral and intramuscular (IM) administration is 20 minutes, and the duration of action is from 4 to 6 hours. The onset of action of intravenous (IV) promethazine is 3 to 5 minutes; the duration of action is the same as for the oral preparation.
Drug and Laboratory Interactions.
Central nervous system (CNS) depression increases when promethazine is taken with alcohol, narcotics, sedative-hypnotics, and general anesthetics. Anticholinergic effects increase when promethazine is combined with antihistamines, anticholinergics such as atropine, and other phenothiazines. Promethazine may interfere with urinary pregnancy tests, producing false results.
Side Effects and Adverse Reactions.
Phenothiazines have antihistamine and anticholinergic properties. The side effects of phenothiazine antiemetics are moderate sedation, hypotension, EPS, CNS effects (restlessness, weakness, dystonic reactions, agitation), and mild anticholinergic symptoms (dry mouth, urinary retention, and constipation). Because the dose is lower for vomiting than for psychosis, the side effects are not so severe. Promethazine is relatively free of EPS at antiemetic doses. Table 47-2 lists the pharmacologic data for phenothiazines and other prescription antiemetics.
Butyrophenones
Haloperidol (Haldol) and droperidol (Inapsine), like phenothiazines, block the dopamine2 receptors in the CTZ. They are used to treat postoperative nausea and the vomiting and emesis associated with toxins, cancer chemotherapy, and radiation therapy. Antiemetic doses of haloperidol are smaller than those required for antipsychotic effects. Like phenothiazines, haloperidol and droperidol are likely to cause EPS if used for an extended time. Hypotension may result; therefore blood pressure should be monitored.
Benzodiazepines
Selected benzodiazepines indirectly control nausea and vomiting that may occur with cancer chemotherapy. Lorazepam (Ativan) is the drug of choice. Previously diazepam (Valium) was the preferred benzodiazepine. Lorazepam effectively provides emesis control, sedation, anxiety reduction, and amnesia when used in combination with a glucocorticoid and serotonin 5-HT3 receptor antagonist.
Serotonin (5-HT3) Receptor Antagonists
Serotonin antagonists suppress nausea and vomiting by blocking the serotonin receptors (5-HT3) in the CTZ and the afferent vagal nerve terminals in the upper GI tract.
Serotonin antagonists—ondansetron (Zofran), granisetron (Kytril), dolasetron (Anzemet), and palonosetron (Aloxi)—are the most effective of all antiemetics in suppressing nausea and vomiting caused by cancer chemotherapy–induced emesis or emetogenic anticancer drugs. Ondansetron (the first serotonin antagonist), granisetron, and dolasetron do not block the dopamine receptors; therefore, they do not cause EPS as do the phenothiazine antiemetics. These drugs can be administered orally and IV. They are also effective in preventing nausea and vomiting before and after surgery. Common side effects include headache, diarrhea, dizziness, and fatigue.
Glucocorticoids (Corticosteroids)
Dexamethasone (Decadron) and methylprednisolone (Solu-Medrol) are two agents that are effective in suppressing emesis associated with cancer chemotherapy. Because these glucocorticoids are administered IV and for only a short while, side effects normally associated with glucocorticoids are minimized. Glucocorticoids are discussed in Chapter 51.
Cannabinoids
Cannabinoids, the active ingredients in marijuana, were approved for clinical use in 1985 to alleviate nausea and vomiting resulting from cancer treatment. These agents may be prescribed for patients receiving chemotherapy who do not respond to or are unable to take other antiemetics. They are contraindicated for patients with psychiatric disorders. Cannabinoids can be used as an appetite stimulant for patients with acquired immunodeficiency syndrome (AIDS). The cannabinoid dronabinol (Marinol) is described in Table 47-2.
Side Effects and Adverse Reactions.
Side effects occurring as a result of cannabinoid use include mood changes, euphoria, drowsiness, dizziness, headaches, depersonalization, nightmares, confusion, incoordination, memory lapse, dry mouth, orthostatic hypotension or hypertension, and tachycardia. Less common symptoms are depression, anxiety, and manic psychosis.
Miscellaneous Antiemetics
Diphenidol (Vontrol) and trimethobenzamide (Tigan) are in the class of miscellaneous antiemetics, because they do not act strictly as antihistamines, anticholinergics, or phenothiazines. These drugs suppress impulses to the CTZ. Diphenidol also prevents vertigo by inhibiting impulses to the vestibular area.
Side Effects and Adverse Reactions.
The side effects and adverse reactions of the miscellaneous antiemetics are drowsiness and anticholinergic symptoms (dry mouth, increased heart rate, urine retention, constipation, and blurred vision). Trimethobenzamide can cause hypotension, diarrhea, and EPS (abnormal involuntary movements, postural disturbances, and alteration in muscle tone).
 , half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than.
, half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than. , half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than.
, half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than; <, less than. : 10-14 h
: 10-14 h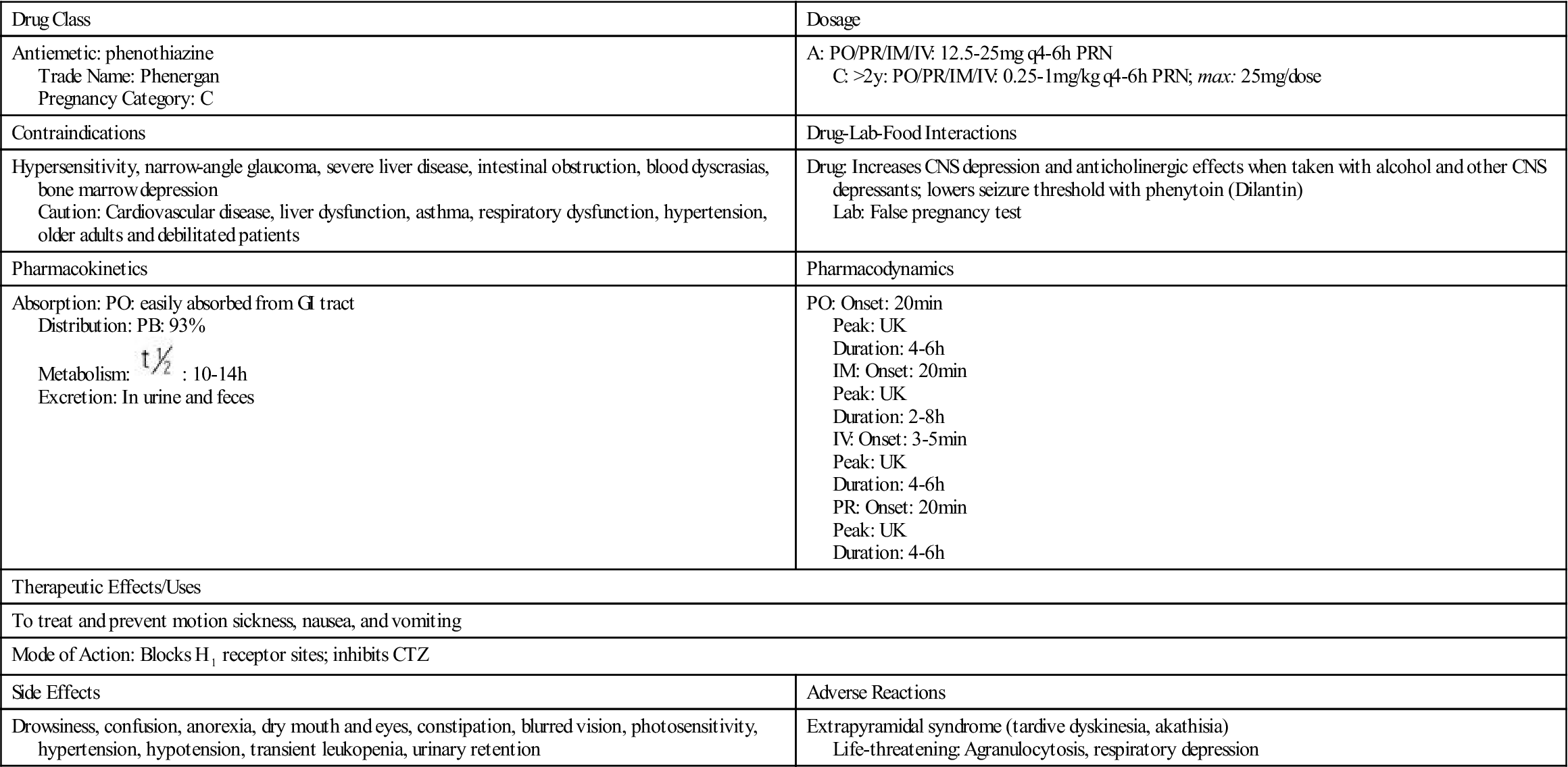
 , half-life; UK, unknown; y, year.
, half-life; UK, unknown; y, year.


















