Drugs for Eye and Ear Disorders
Objectives
• Describe the medication groups commonly used for disorders of the eye and ear.
• Develop teaching plans for the drug groups presented.
Key Terms
carbonic anhydrase inhibitors, p. 718
cerumen, p. 725
ceruminolytics, p. 725
conjunctivitis, p. 710
cycloplegics, p. 720
glaucoma, p. 714
intraocular pressure, p. 714
lacrimal duct, p. 710
miosis, p. 715
mydriatics, p. 720
narrow-angle glaucoma, p. 714
ocular, p. 710
open-angle glaucoma, p. 714
ophthalmic, p. 710
osmotics, p. 718
otitis externa, p. 722
prostaglandin analogues, p. 715
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
The authors gratefully acknowledge the work of Jacqueline Rosenjack Burchum, who updated this chapter for the eighth edition.
Drugs for Disorders of the Eye
Problems associated with the eyes may occur as the result of injuries, infections, and specific eye disorders like glaucoma and macular degeneration. Most drugs used to treat these conditions are topical medications in formulations developed specifically for sensitive eyes. Drugs designed to be applied to the eyes are known as ocular or ophthalmic drugs.
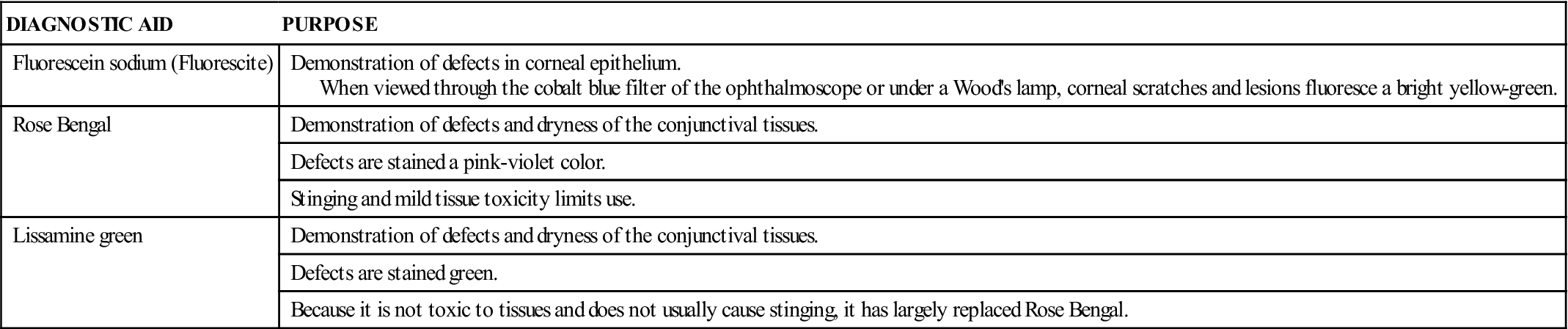
Diagnostic Stains
Diagnostic stains (Table 49-1) are frequently used to locate lesions or foreign objects, evaluate dry eye, or evaluate eye changes from poorly fitting contact lenses. Stains may be combined with local anesthetics to allow more thorough examination when pain is present. Patients should be informed that these drugs may stain nasal secretions if the lacrimal ducts (tear ducts) are patent; they can also discolor soft contact lenses. Contact lenses should be removed before administration. After the procedure, the stain should be flushed out with normal saline; contact lenses can be replaced after 1 hour.
TABLE 49-1
DIAGNOSTIC STAINS FOR EYE DISORDERS
| DIAGNOSTIC AID | PURPOSE |
| Fluorescein sodium (Fluorescite) | Demonstration of defects in corneal epithelium. When viewed through the cobalt blue filter of the ophthalmoscope or under a Wood’s lamp, corneal scratches and lesions fluoresce a bright yellow-green. |
| Rose Bengal | Demonstration of defects and dryness of the conjunctival tissues. |
| Defects are stained a pink-violet color. | |
| Stinging and mild tissue toxicity limits use. | |
| Lissamine green | Demonstration of defects and dryness of the conjunctival tissues. |
| Defects are stained green. | |
| Because it is not toxic to tissues and does not usually cause stinging, it has largely replaced Rose Bengal. |
Topical Anesthetics
Topical anesthetics are used in selected aspects of a comprehensive eye examination and in a variety of ophthalmic procedures. The two most common topical ophthalmic anesthetics are proparacaine HCl and tetracaine HCl (Pontocaine). Both medications are administered as drops.
Corneal anesthesia is achieved within 1 minute and generally lasts about 15 minutes. The blink reflex is temporarily lost; therefore, the corneal epithelium may become dry. To protect the eye, a patch is usually worn until the effects of the drug are gone. However, because patching of the eye may impede healing, the patch should be removed once sensation and the blink reflex return.
Ophthalmic anesthetics are not to be self-administered by the patient. Repeated doses are given only under strict medical supervision.
Antiinfectives
Antiinfectives (Table 49-2) are frequently used for eye infections. Conjunctivitis, an inflammation of the delicate membrane covering the eye and inner eyelids, is the most common eye condition requiring antibiotic therapy. Examples of other ocular conditions treated with ophthalmic antiinfective drugs include the following:
• Blepharitis (infection of margins of eyelid)
• Bacterial and fungal endophthalmitis (infection and inflammation of structures of the inner eye)
• Hordeolum (local infection of eyelash follicles and glands on lid margins, also known as a stye)
• Infectious keratitis (corneal infection and inflammation)
• Infectious uveitis (infection of vascular layer of eye [ciliary body, choroid, and iris])
TABLE 49-2
| GENERIC (BRAND) | ROUTE AND DOSAGE* | USES AND CONSIDERATIONS |
| Antibacterials | ||
| chloramphenicol | A/C: Ophthalmic: Instill 1-2 gtt or  -inch ribbon of oint q3-4h for 48 h; increase interval to b.i.d./t.i.d. -inch ribbon of oint q3-4h for 48 h; increase interval to b.i.d./t.i.d. | For severe ophthalmic infections that are unresponsive to other antibiotics. Effective against gram-negative and gram-positive bacteria. Boxed warning: Bone marrow suppression and deaths have resulted from topical administration. Continue treatment for at least 48 h after eye appears normal. Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| ciprofloxacin (Ciloxan) 5 mg/mL sol | Bacterial conjunctivitis: Solution: A/C: >1 y: 1-2 gtt q2h while awake for 2 d, then q4h while awake for 5 d Bacterial conjunctivitis: Ointment: A/C: >2 y:  -inch ribbon t.i.d for 2 d, then -inch ribbon t.i.d for 2 d, then  -inch ribbon b.i.d for 5 d -inch ribbon b.i.d for 5 dCorneal ulcer: A/C: >1 y: Day 1: 2 gtt q15min for 6 h, then 2 gtt q30min for rest of day Day 2: 2 gtt q1h Days 3-14: 2 gtt q4h | For bacterial conjunctivitis and corneal ulceration. Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| erythromycin | Chlamydial conjunctivitis or ophthalmia neonatorum caused by Chlamydia trachomatis: Oral dosage: Neonates/infants: CDC recommends 50 mg/kg/d PO divided q.i.d. for 14 d. Second course may be required. CDC states that topical therapy alone is inadequate and unnecessary when systemic therapy is administered. Ophthalmia neonatorum caused by Neisseria gonorrhoeae or Chlamydia trachomatis: Ophthalmic dosage: A: Instill 1-2 gtt of 0.25% sol into each affected eye b.i.d., or instill 1-2 gtt of 0.5% sol into each affected eye once/d. Greater than 1 gtt of 0.5% preparation b.i.d. generally does not further reduce IOP and is not recommended. Neonates: Apply a ribbon of 0.5% ophthalmic ointment into each lower conjunctival sac no later than 1 hour after birth | For chlamydial conjunctivitis caused by C. trachomatis and ophthalmia neonatorum caused by C. trachomatis or N. gonorrhoeae. Prolonged use can lead to acquired sensitivity. Contact lenses should not be worn for duration of treatment. Pregnancy category: B |
| gentamicin sulfate (Garamycin Ophthalmic, Gentak) | A/C: Sol 0.3%: 1-2 gtt q4h; may increase to 2 gtt q1h for severe infections Oint 0.3%:  -inch ribbon b.i.d./t.i.d. -inch ribbon b.i.d./t.i.d. | For blepharitis, blepharo-conjunctivitis, bacterial conjunctivitis, corneal ulcer, dacryocystitis, keratitis, kerato-conjunctivitis, and acute meibomianitis. Ophthalmia neonatorum secondary to N. gonorrhoeae May cause ototoxicity (toxic effect on eighth cranial nerve), which may be permanent. Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| levofloxacin | A: 1-2 gtts q2h; max: 8 doses/d for 1-2 d; then q4h; max: 4 doses/d for 5 d | For bacterial conjunctivitis and corneal ulcers (Systemic therapy is required for treatment of hordeolum, dacryocystitis, and meibomianitis). Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| silver nitrate 1% (Dey-Drop) | Neonate: Instill 2 gtt in each eye within 1 h of birth | For prophylaxis of ophthalmia neonatorum caused by N. gonorrhoeae Pregnancy category: C |
| sulfacetamide (Bleph-10) | A/C: >12 y: Sol: 1 gtt q1-3h while awake; then q3-4h while sleeping | For conjunctivitis, corneal ulcer, and adjunctive therapy for chlamydial conjunctivitis. Effectiveness of sulfonamides decreased in presence of PABA and purulent drainage; hence, remove exudates before instilling drops. Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| tobramycin (Tobrex) | A/C: >12 y: Oint 0.3%:  -inch ribbon b.i.d./t.i.d -inch ribbon b.i.d./t.i.dSol 0.3%: 1-2 gtt q4h For severe infections: Oint:  -inch ribbon q3-4h -inch ribbon q3-4hSol: 2 gtt q30-60min until improvement, then decrease frequency | For external ocular infections. Contact lenses should not be worn for duration of treatment. Pregnancy category: D |
| tetracycline HCl | A: Instill 1-2 gtt b.i.d./q.i.d. A: Instill  -inch ribbon q2-12h -inch ribbon q2-12h | Bacteriostatic action; alternative to silver nitrate for prevention of ophthalmia neonatorum. Contact lenses should not be worn for duration of treatment. Pregnancy category: D |
| triple antibiotic ophthalmic ointment (neomycin, polymyxin B Sulfate, bacitracin ophthalmic) | A/C: >12 y: 1 cm applied in conjunctival sac q3-4h | Combination antibiotic effective against many gram-positive and gram-negative organisms. Do not use longer than 10 d. Contact lenses should not be worn for duration of treatment. Pregnancy category: C |
| Antifungals | ||
| natamycin (Natacyn Ophthalmic) | A/C: Sol 5%: 1 gt q2h for 3-4 d; then 1 gt q3h for 14-21 d | May cause transient stinging or temporary blurring of vision. Pregnancy category: C |
| Antivirals | ||
| idoxuridine (IDU, Herplex Liquifilm) | A/C: Sol 1%: Initially: 1 gt q1h during day and q2h at night; when definite improvement occurs, use 1 gt q2h during day and q4h at night; continue 3-7 d after healing occurs Oint 0.5%: Place  -inch ribbon q4h while awake -inch ribbon q4h while awake | For cytomegalovirus and herpes simplex keratitis. Store in refrigerator; do not mix with boric acid. Discontinue if no response in 1 wk. Pregnancy category: C |
| trifluridine (Viroptic) | A: Sol 1%: Instill 1 gt into infected eye q2h while awake; max: 9 gtt/d until corneal ulcer reepithelialized; then 1 gt q4h for 7 d; max: 21 d of treatment | For herpetic ophthalmic infections and keratoconjunctivitis caused by HSV-1 and HSV-2. Pregnancy category: C |
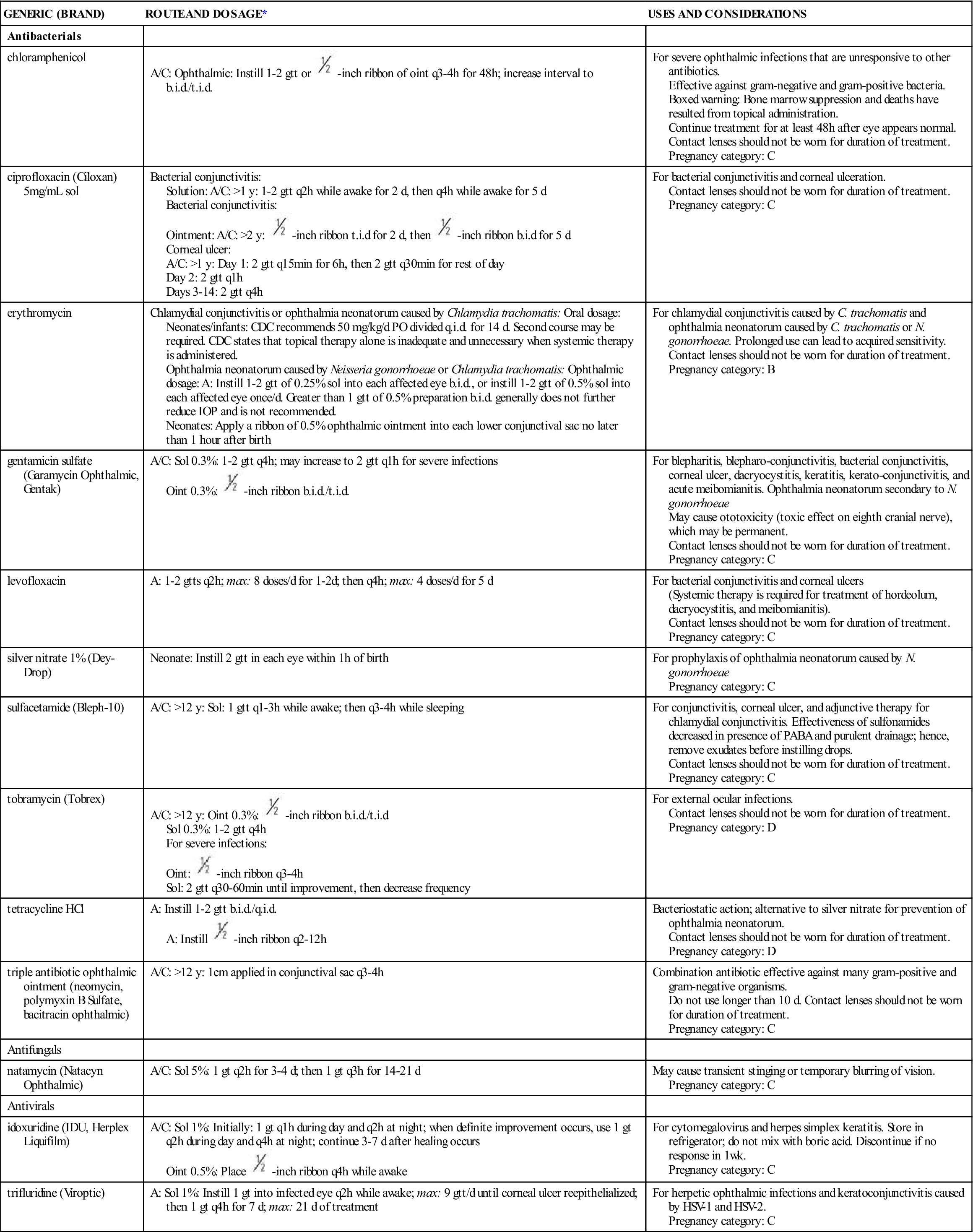
*To minimize systemic absorption, gently apply pressure on inner canthus.
Before administering ophthalmic antiinfectives, the nurse should screen the patient for previous allergic reactions. Noninfectious conjunctivitis and local skin and eye irritation are possible side effects of topical antiinfective drugs.
Antiinflammatories
Inflammatory conditions of the eye often require treatment with antiinflammatory drugs (Table 49-3) such as NSAIDs and corticosteroids. If the inflammation is secondary to a bacterial or fungal infection, an antibiotic or antifungal agent is included in the medication regimen. Antiinflammatories should not be given if the patient has a viral infection.
TABLE 49-3
| GENERIC (BRAND) | ROUTE AND DOSAGE* | USES AND CONSIDERATIONS |
| Nonsteroidal Antiinflammatory Drugs (NSAIDs) | ||
| diclofenac sodium (Voltaren Ophthalmic) | A: 1 gt to affected eye q.i.d. for 2 wk; start 24 h after cataract surgery | For postoperative inflammation and photophobia after cataract surgery. May increase bleeding and delay healing. Increased risk for keratitis and elevated IOP. Pregnancy category: C |
| flurbiprofen sodium (Ocufen) | A: Instill 1 gt q30min starting 2 h before surgery; total dose is 4 gtt | For prevention of intraoperative miosis. May increase bleeding and delay healing. Pregnancy category: C |
| ketorolac tromethamine (Acular) | Allergic conjunctivitis: A/C >2 y: Sol 0.5%: Instill 1 gt q.i.d. Following cataract surgery: A: Begin q.i.d 24 h postop, and continue for 2 weeks | For relief of itching due to allergic conjunctivitis and management of inflammation post–cataract surgery. May increase bleeding and delay healing. Pregnancy category: C |
| suprofen (Profenal) (Maple Leaf) | Preoperative: A: Instill 2 gtt in sac q4h while awake on day preceding surgery; instill 2 gtt in conjunctival sac at 3, 2, and 1 h before surgery | For prevention of intraoperative miosis. May increase bleeding and delay healing. Pregnancy category: C |
| Corticosteroids | ||
| dexamethasone ( Maxidex) | A/C: Oint: Apply into conjunctival sac t.i.d./q.i.d.; gradually decrease to discontinue Susp: Instill 2 gtt q1h while awake and q2h during night; taper to q3-4h; then t.i.d./q.i.d. | For uveitis; allergic conditions; and inflammation of conjunctiva, cornea, and lids. Not recommended for minor abrasions and wounds. May delay healing. Avoid use with viral infections. Pregnancy category: C |
| medrysone (HMS Liquifilm) | A/C: Susp: Initially: Instill 1 gt in conjunctival sac q1-2h (1-2 d); then 1 gt b.i.d./q.i.d. | For allergic conditions, burns, and inflammation of conjunctiva, cornea, and lids. May delay healing. Avoid use with viral infections. Pregnancy category: C |
| prednisolone acetate (Econopred Plus) | A: Initially instill 1-2 gtt in conjunctival sac q1h while awake, q2h during night until desired effect; maint: 1 gt q4-6h Susp: 0.125% and 1% | For uveitis; allergic conditions; burns; and inflammation of conjunctiva, cornea, and lids. May delay healing. Avoid use with viral infections. Pregnancy category: C |
| prednisolone sodium phosphate | A/older adults: Sol 0.125% and 1%: 1-2 gtt q1h during day; q2h at night; with response, give 1 gt q4-6h Oint: thin coat t.i.d./q.i.d.; with response, decrease to b.i.d., then daily | To prevent or decrease tissue response to inflammatory process. May delay healing. Avoid use with viral infections. Pregnancy category: C |
| Ophthalmic Antihistamines | ||
| emedastine (Emadine) | A/C ≥3 y: 1 gtt up to 4 times/d | For allergic conjunctivitis. Wait 10 minutes after administration before inserting contact lenses. Pregnancy category: B |
| epinastine (Elestat) | A/C ≥3 y: 1 gtt b.i.d. | For allergic conjunctivitis Wait 10 minutes after administration before inserting contact lenses. Pregnancy category: C |
| Ophthalmic Mast Cell Stabilizers | ||
| cromolyn (Crolom) | A/C >4 y: 1-2 gtt in each eye 4-6 times/d | For allergic conjunctivitis Contact lenses should not be worn for duration of therapy Pregnancy category: B |
| nedrocromil ophthalmic (Alocril) | A/C ≥3 y: 1-2 gtt b.i.d. | For allergic conjunctivitis About 40% experience headache; 10%-30% experience burning sensation Contact lenses should not be worn for duration of therapy Pregnancy category: B |
| Ophthalmic Drugs with Both Antihistamines and Mast Cell Stabilizer Properties | ||
| azelastine (Optivar) | A/C ≥3 y: 1 gtt in each eye b.i.d. | For allergic conjunctivitis. Has both antihistamine and mast-cell stabilizing actions. 11.5% experience drowsiness; enhances CNS depressants Wait 10 minutes after administration before inserting contact lenses. Pregnancy category: C |
| epinastine (Elestat) | A/C ≥3 y: 1 gtt each eye b.i.d. | For allergic conjunctivitis. Has both antihistamine and mast-cell stabilizer actions 1%-10% develop coldlike symptoms. Wait 10 minutes after administration before inserting contact lenses. Pregnancy category: C |
| ketotifen (Zaditor) | A/C ≥3 y: 1 gtt in each eye q8-12h | For allergic conjunctivitis. 10%-25% experience mild hyperemia and headache. Wait 10 minutes after administration before inserting contact lenses. Pregnancy category: C |
| olopatadine (Patanol) | A/C ≥3 y: 0.1% sol: 1 drop in each affected eye b.i.d. at an interval of 6-8 h | For allergic conjunctivitis. May potentiate CNS depressants if systemically absorbed. Wait 10 minutes after administration before inserting contact lenses. If eyes turn red, do not wear contact lenses. Pregnancy category: C |
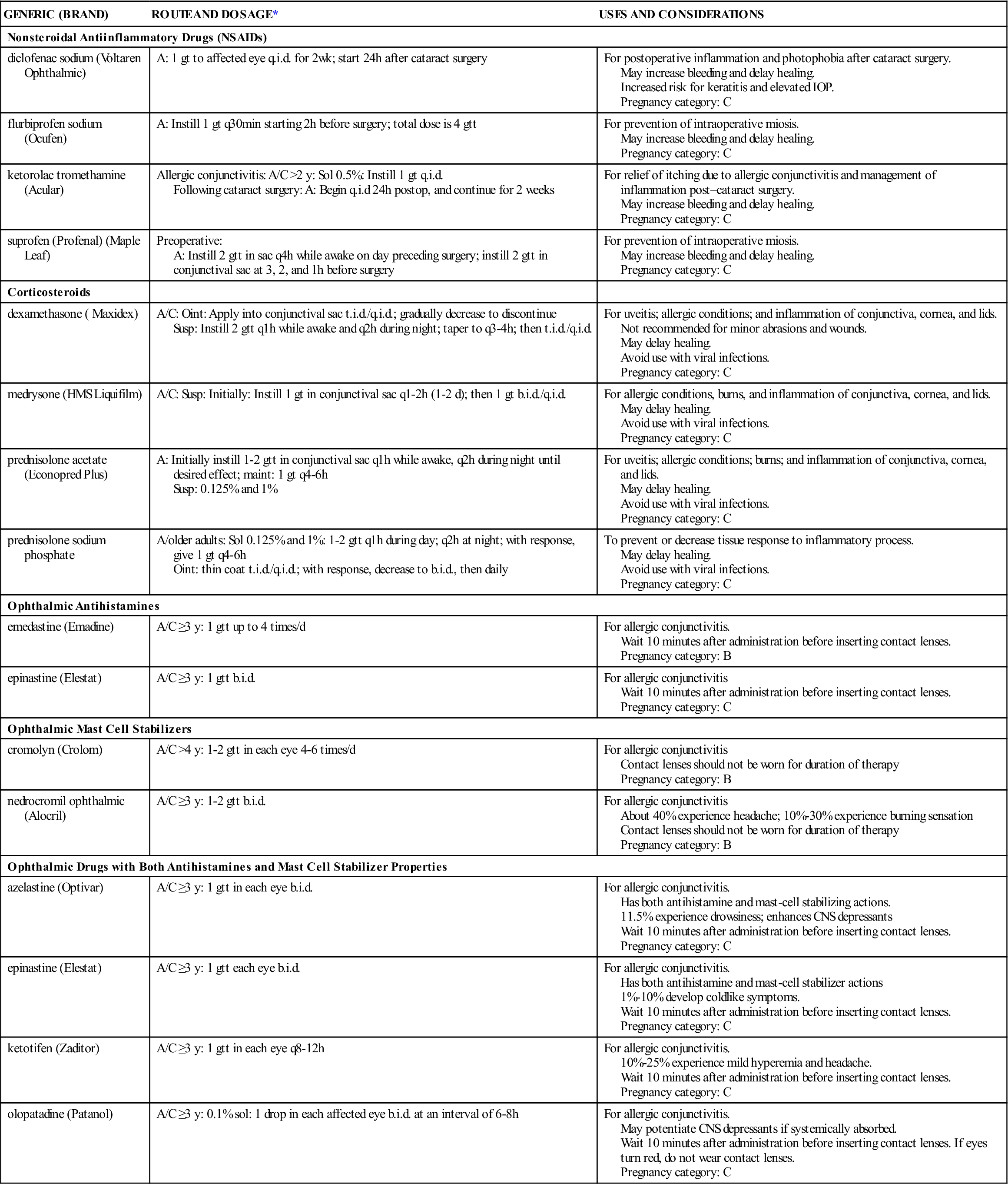
*To minimize systemic absorption, gently apply pressure on inner canthus.
When allergies are the cause of eye inflammation, ophthalmic antihistamines and mast cell stabilizers are commonly prescribed to treat the underlying cause. Antihistamines block histamine from activating histamine receptors in the tissues. Examples of ophthalmic antihistamines include emedastine (Emadine) and epinastine (Elestat). Mast cell stabilizers prevent mast cells from breaking open and releasing histamine and other inflammatory mediators. Ophthalmic mast cell stabilizers include cromolyn (Crolom) and nedrocromil ophthalmic (Alocril). Some drugs, such as azelastine (Optivar), epinastine, ketotifen (Zaditor) and olopatadine (Patanol), have both antihistamine and mast cell stabilizer effects. Burning, headache, and stinging may occur in some patients and are the most frequent adverse effects of these drugs.
Decongestants
Eye inflammation typically presents with redness due to vascular congestion of the conjunctiva. Ophthalmic decongestants are vasoconstrictors that manage these effects by narrowing these blood vessels. Examples of ophthalmic decongestants are phenylephrine (Neo-Synephrine Ophthalmic), naphazoline (Clear Eyes), tetrahydrozoline (Opti-Clear), and oxymetazoline (Ocuclear). If these are absorbed in significant amounts, their sympathetic nervous system effects may pose problems for patients with hypertension. Patients who have narrow-angle glaucoma should not use these drugs because they may contribute to acute angle-closure, which is a medical emergency.
Lubricants
Eye lubricants replace tears to alleviate discomfort associated with eye dryness. They are also used to moisten contact lenses and artificial eyes. During anesthesia and in acute or chronic central nervous system (CNS) disorders that result in unconsciousness or decreased blinking, lubricants keep eyes moist and maintain the integrity of the epithelial surface of the eye.
Most lubricants are available over the counter (OTC) in both liquid and ointment form. Popular lubricants include Isopto Tears, Tearisol, Ultra Tears, Tears Naturale, Tears Plus, Lens Mate, and Lacri-Lube. While these agents typically are safe, the nurse must be alert to potential allergic reactions to preservatives in lubricants.
Immunosuppressants
Cyclosporine ophthalmic emulsion (Restasis) relieves dry eyes by a mechanism that is different from lubricants. It is prescribed for patients who have decreased tear production due to inflammation. Cyclosporine suppresses the immune response that leads to inflammation, allowing tear production to resume.
Ophthalmic corticosteroids are another type of immunosuppressant. Corticosteroids are used to treat a number of conditions that manifest as significant eye inflammation. Examples include prednisolone (Pred Forte), dexamethasone (Maxidex), loteprednol (Lotemax), rimexolone (Vexol), and fluorometholone (FML). Refer to Chapter 25 for more information on corticosteroids.
Because they suppress the immune response, ophthalmic immunosuppressants should not be given to patients with bacterial infections of the eye unless accompanied by an antibiotic that treats the underlying infection. Ophthalmic immunosuppressants are contraindicated for viral eye infections such as herpes.
Antiglaucoma Agents
Glaucoma is an eye condition in which optic nerve damage occurs as a result of increased intraocular pressure (IOP), which is a buildup of pressure within the eye that occurs when there is too much aqueous humor. Without treatment, permanent loss of vision can occur.
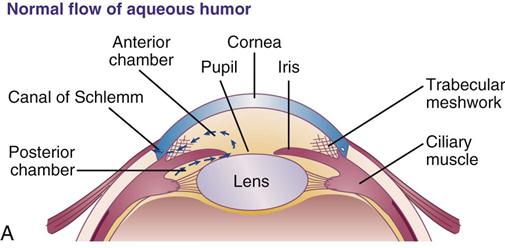
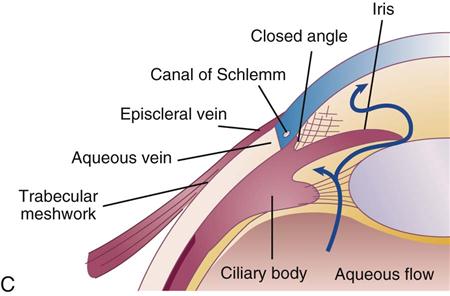
Typically, as aqueous humor is formed, excess fluid drains though the trabecular meshwork structure of the eye and out the canal of Schlemm, with a much smaller fraction of the fluid exiting through the uveoscleral structure at the root of the iris (Figure 49-1, A). In glaucoma, excess fluid is prevented from draining through the trabecular structure.
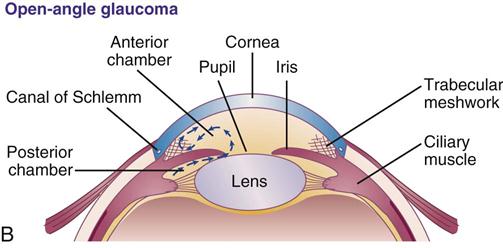
There are two types of glaucoma. In open-angle glaucoma, the trabecular network becomes clogged (Figure 49-1, B). Over time, as blockage of the trabecular network worsens, the IOP gradually increases.
In narrow-angle glaucoma, also known as closed-angle or angle-closure glaucoma, the iris bows and blocks the trabecular network by narrowing or closing the angle where fluid typically exits the eye (Figure 49-1, C). Because the excess aqueous humor cannot drain, it builds up within the eye, increasing IOP. Management of narrow-angle glaucoma is often surgical; however, pharmacologic management is sometimes indicated.
Glaucoma is further classified as either primary or secondary. Primary glaucoma occurs due to a pathologic change within the eye that happens without a known cause. Primary open-angle glaucoma (POAG), the most common type of glaucoma, is a chronic condition that develops slowly over time as the trabecular meshwork becomes clogged for unknown reasons. Secondary glaucoma occurs in response to a known cause such as injury, disease, or medication. While a number of drugs can increase the risk of secondary glaucoma, those that cause pupillary dilation are particularly problematic because they give the iris more flexibility to move in a way that blocks the trabecular meshwork. Certain herbal preparations can also create problems when given to patients who have glaucoma (Herbal Alert 49-1).
Antiglaucoma drugs belong to one of the following categories: prostaglandin analogues, beta-adrenergic blockers, alpha-adrenergic agonists, cholinergic agents, carbonic anhydrase inhibitors, or systemic hyperosmotic drugs. Prostaglandin analogues and beta-adrenergic blockers are typically first-line therapy, followed by alpha-adrenergic agonists. Each category acts in different ways to decrease IOP.
Prostaglandin Analogues
Prostaglandin analogues (Table 49-4) are first-line drugs used primarily in the treatment of open-angle glaucoma; however, studies suggest a role in management of narrow-angle glaucoma, as well. These drugs decrease IOP by improving trabecular outflow and by increasing the uveoscleral pathway, which is an alternate pathway of aqueous humor outflow. Examples of prostaglandin analogues include bimatoprost (Lumigan), latanoprost (Xalatan) (Prototype Drug Chart 49-1), tafluprost (Zioptan), and travoprost (Travatan).
TABLE 49-4
PROSTAGLANDIN ANALOGUES USED TO TREAT GLAUCOMA
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| latanoprost (Xalatan) | A: 1 gt 0.005% sol h.s. | Decreases IOP in open-angle glaucoma; may have a role in narrow-angle glaucoma, but more studies needed. Few adverse effects. Not recommended for patients with torn or absent lens or with eye trauma. Do not insert contact lenses for 15 minutes after administration. Pregnancy category: C |
| bimatoprost (Lumigan) | A: 1 gt 0.03% sol h.s. | Decreases IOP in open-angle glaucoma; may have a role in narrow-angle glaucoma, but more studies are needed. Few adverse effects. Not recommended for patients with torn or absent lens or with eye trauma. May worsen intraocular inflammation. Onset is 4 h, and peak action occurs in 4-12 h. Pregnancy category: C |
| travoprost (Travatan Z) | A: 1 gt 0.004% sol h.s. | Decreases IOP in open-angle glaucoma; may have a role in narrow-angle glaucoma, but more studies needed. Few adverse effects. Avoid use in patients with torn or absent lens or with eye trauma. More effective in African Americans than in non–African Americans. Onset is 2 h, with peak action occurring in 12 h. |
| tafluprost (Zioptan) | A: 1 gt every evening | Decreases IOP in open-angle glaucoma; may have a role in narrow-angle glaucoma, but more studies needed. Few adverse effects. Avoid use in patients with torn or absent lens or with eye trauma. Information on contact lenses not available in prescribing information/package insert. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 , half-life; t.i.d., three times a day; wk, week; y, year; >, greater than.
, half-life; t.i.d., three times a day; wk, week; y, year; >, greater than. , half-life; t.i.d., three times a day; q.i.d., four times a day; wk, week.
, half-life; t.i.d., three times a day; q.i.d., four times a day; wk, week.