Understand the etiology, pathophysiology, and clinical manifestations of attention deficit hyperactivity disorder.
 Understand the etiology, pathophysiology, and clinical manifestations of narcolepsy.
Understand the etiology, pathophysiology, and clinical manifestations of narcolepsy.
 Describe general characteristics of central nervous system stimulants.
Describe general characteristics of central nervous system stimulants.
 Identify the prototypes and discuss the action, use, adverse effects, contraindications, and nursing implications for the stimulants used in the treatment of attention deficit hyperactivity disorder and narcolepsy.
Identify the prototypes and discuss the action, use, adverse effects, contraindications, and nursing implications for the stimulants used in the treatment of attention deficit hyperactivity disorder and narcolepsy.
 Identify sources and effects of caffeine.
Identify sources and effects of caffeine.
 Implement the nursing process in the care of patients who take central nervous stimulants.
Implement the nursing process in the care of patients who take central nervous stimulants.
Clinical Application Case Study
Brian Connor received a diagnosis of attention deficit hyperactivity disorder at 7 years of age. He is now 9 years old. As a result of taking methylphenidate (Ritalin) 15 mg daily and receiving individual counseling, his attention span and school performance have improved. However, his most recent physical examination shows that his height and weight are less than normal for his age and that he has lost weight since his examination last year. The school nurse talks with Brian’s teachers, who report that he seems more restless in class after lunch. He has had more difficulty getting along with his classmates due to his impulsive behaviors.
KEY TERMS
Attention deficit hyperactivity disorder: relatively common disorder of childhood onset characterized by inattention, impulsiveness, and overactivity
Narcolepsy: sleep disorder in which a person goes to sleep at any place or at any time
Introduction
This chapter introduces the pharmacological care of attention deficit hyperactivity disorder (ADHD) and narcolepsy. Clinicians use drugs that stimulate the central nervous system (CNS) to treat these disorders.
Overview of Attention Deficit I Hyperactivity Disorder
To adequately understand the pharmacologic treatment of attention deficit hyperactivity disorder, or ADHD, it is important to understand the causes, pathophysiology, and clinical manifestations of ADHD. This condition is characterized by persistent hyperactivity, short attention span, difficulty completing assigned tasks or schoolwork, restlessness, and impulsiveness.
Etiology and Pathophysiology
ADHD is the most common psychiatric or neurobehavioral disorder in children. Although the cause is not fully understood, evidence suggests that subtle dysfunction in the frontal lobe and functionally related subcortical structures plays an essential role in the core symptoms of ADHD. Research has suggested that ADHD is a highly heritable, neurobiological disorder partially attributed to dopamine and norepinephrine transport dysfunction in the brain.
ADHD is usually diagnosed between 3 and 7 years of age and may affect as many as 8% of school-age children. Children with ADHD find it difficult to get along with others (e.g., family members, peer groups, teachers) and to function in situations requiring controlled behavior (e.g., classrooms). Approximately 10% to 20% of children with ADHD also have a diagnosed learning disability, causing further academic and emotional difficulties.
ADHD continues into adolescence and adulthood in approximately 50% of cases and may affect 4% of adults in the United States. In adolescents and adults, hyperactivity is not prominent, but impulsiveness, inattention, and difficulties in structured settings such as school or work may continue. Some studies indicate that children with ADHD are more likely to have mood disorders and substance abuse disorders as adolescents and adults. A major criterion for diagnosing later ADHD is a previous diagnosis of ADHD by 7 years of age. Some authorities believe this age limit is too restrictive. The diagnosis of ADHD in adults has greatly increased in recent years, with a concomitant increase in the use of prescribed CNS stimulants for its treatment.
Clinical Manifestations
Clinical manifestations of ADHD usually occur in various or multiple environments in a child’s life, including school, home, church, or recreational activities. The level of problems typically varies, but symptoms generally worsen in situations that require sustained attention, such as listening to teacher, performing repetitive tasks, or reading lengthy materials.
Hyperactivity in children presents as fidgeting or squirming in their seats, excessive running or climbing when it is dangerous or inappropriate, disruptive playing during quiet activities, and demonstrating a driven verbal or motor quality. Impulsivity manifests as impatience, blurting out answers, and frequently interrupting others. Inattention manifests as messy work, careless mistakes, and appearance of daydreaming. Based on the behaviors associated with ADHD, affected people also may have low self-esteem and strained peer relations. Early diagnosis and treatment are essential. Evidence suggests that behavior management combined with pharmacotherapy yields the best outcomes.
Drug Therapy
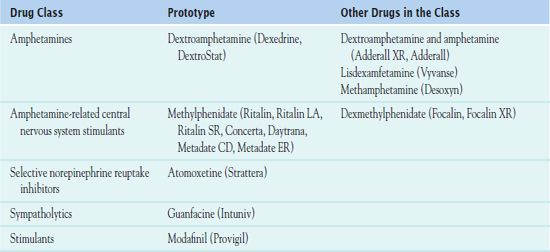
Drug therapy is indicated when symptoms are moderate to severe; are present for several months; and interfere in social, academic, or behavioral functioning. Counseling and psychotherapy (e.g., parental counseling, family therapy) are recommended along with drug therapy for effective treatment and realistic expectations of outcomes. Young children may not require treatment until starting school. Then, the goal of drug therapy is to control symptoms, facilitate learning, and promote social development. Table 56.1 summarizes the drugs used in the treatment of ADHD. Treatment is based on individual signs and symptoms.
Overview of Narcolepsy
To adequately understand the pharmacologic treatment of the chronic sleep disorder narcolepsy, it is important to understand the causes, pathophysiology, and clinical manifestations of narcolepsy. This condition is characterized by excessive sleepiness and sleep attacks at inappropriate times, such as at work.
Etiology and Pathophysiology
Narcolepsy is a neurological sleep disorder, not the result of mental illness or psychological problems. It is most likely due to a number of genetic abnormalities that affect specific biologic factors in the brain, combined with an environment trigger, such as exposure to a virus, during the brain’s development. The exact cause is unknown, and sleep studies are required for an accurate diagnosis. People with narcolepsy often have a reduced number of protein-producing neurons in the brain that are responsible for controlling appetite and sleep patterns.
Narcolepsy affects men and women equally and usually begins during the teenage or young adult years. When people with narcolepsy fall asleep, they generally experience the rapid eye movement (REM) stage of sleep within 10 minutes, whereas most people experience REM sleep after 1 hour of sleep.
Clinical Manifestations
People with narcolepsy often experience disturbed nocturnal sleep and an abnormal daytime sleep pattern; it is important not to confuse this pattern with insomnia. Excessive daytime drowsiness (even after an adequate night’s sleep) and fatigue are characteristic. People are likely to become drowsy or fall asleep or just be very tired. The hazards of drowsiness during normal waking hours and suddenly going to sleep in unsafe environments restrict activities of daily living.
Other signs and symptoms of narcolepsy include cataplexy, hypnagogic hallucinations, disturbances of nighttime sleep patterns, and sleep paralysis. Cataplexy is an episodic condition featuring the loss of muscle function, ranging from slight weakness to complete body collapse. These episodes may be triggered by emotional reactions such as laughter, anger, or fear, lasting from a few seconds to minutes. Hypnagogic hallucinations are vivid, often frightening, dream-like experiences that occur while dozing, falling asleep, or awakening. Sleep paralysis is the temporary inability to move or talk on waking.
Drug Therapy
Treatment of narcolepsy is based on individual symptoms and therapeutic response. In addition to drug therapy, prevention of sleep deprivation, regular sleeping and waking times, avoiding shift work, and short naps may be helpful in reducing daytime sleepiness. However, even adequate amounts of nighttime sleep do not produce full alertness. Table 56.1 summarizes the medications used in the treatment of narcolepsy.
Clinical Application 56-1
Brian has been disrupting class, most notably after lunch. The teachers have contacted his parents regarding this situation. His parents have made an appointment with his health care provider, who has changed his medication to methylphenidate (Ritalin ER 18 mg). This new medication comes in capsule form, and Brian and his parents are afraid that he cannot swallow the large capsule.
 Is this an appropriate medication change?
Is this an appropriate medication change?
 Brian’s mother asks if she can empty the contents of the capsule in applesauce. What patient teaching should the nurse implement?
Brian’s mother asks if she can empty the contents of the capsule in applesauce. What patient teaching should the nurse implement?
 What strategies might the nurse suggest to Brian and his parents to help him with taking this new medication?
What strategies might the nurse suggest to Brian and his parents to help him with taking this new medication?
NCLEX Success
1. A child with attention deficit hyperactivity disorder would most likely exhibit which of the following symptoms?
A. anxiety
B. positive peer relationships
C. hostility
D. restlessness
2. A 7-year-old boy takes methylphenidate every morning. Which of the following behaviors would a nurse expect the child to engage in?
A. to sit and play with his toys for 90 minutes
B. to get along better with his peers
C. to express his anger in an appropriate manner
D. not to throw his toys across the room
Stimulants
CNS stimulants act by facilitating initiation and transmission of nerve impulses that excite other cells. The drugs are somewhat selective in their actions at lower doses but tend to involve the entire CNS at higher doses. In ADHD, the drugs improve academic performance, behavior, and interpersonal relationships. In narcolepsy, stimulants improve the performance of daily activities by 70% to 80% of normal (Burgess & Scammell, 2012). Major groups of stimulants are amphetamines, amphetamine-related drugs, and xanthines.
The main goal of therapy with CNS stimulants is to relieve symptoms of the disorders for which they are given. A secondary goal is to have patients use the drugs appropriately. Misuse and abuse of stimulants often occurs when people who want to combat fatigue and delay sleep, such as long-distance drivers, students, and athletes, take the drugs. College students reportedly use stimulants as study aids; this is not justified. These drugs are dangerous for drivers and those involved in similar activities, and they have no legitimate use in athletics.
When a prescriber orders a CNS stimulant, the dose starts low and then increases as necessary, usually at weekly intervals, until the drug becomes effective or the dose reaches a maximum. It is also necessary to limit the number of doses that can be obtained with one prescription. This action reduces the likelihood of drug dependence or diversion (use by people for whom the drug is not prescribed).
Overdoses may occur with acute or chronic ingestion of large amounts of a single stimulant, combinations of stimulants, or concurrent ingestion of a stimulant and another drug that slows the metabolism of the stimulant. Signs of toxicity may include severe agitation, cardiac dysrhythmias, combativeness, confusion, delirium, hallucinations, high body temperature, hyperactivity, hypertension, insomnia, irritability, nervousness, panic states, restlessness, tremors, seizures, coma, circulatory collapse, and death.
AMPHETAMINES
Amphetamines produce mood elevation or euphoria, increasing mental alertness and capacity for work, decreasing fatigue and drowsiness, and prolonging wakefulness. Large doses can lead to signs of excessive CNS stimulation (e.g., agitation, confusion, hyperactivity, difficulty concentrating on tasks, hyperactivity, nervousness, restlessness) and sympathetic nervous system stimulation (e.g., increased heart rate and blood pressure, pupil dilation, slowed gastrointestinal [GI] motility, and other symptoms). Overdoses can result in psychosis, convulsions, stroke, cardiac arrest, and death. Amphetamines are schedule II drugs under the Controlled Substances Act; they have a high potential for drug abuse and dependence. Widely sold on the street, they are commonly abused.  Dextroamphetamine (Dexedrine, DextroStat) is the prototype amphetamine.
Dextroamphetamine (Dexedrine, DextroStat) is the prototype amphetamine.
Pharmacokinetics
Dextroamphetamine has a rapid absorption and onset of action. The drug reaches its peak in 1 to 5 hours, and the duration is between 8 and 10 hours. It is metabolized by the liver and excreted in the urine. Dextroamphetamine may cross the placenta and has been found in breast milk.
Action
Dextroamphetamine acts in the CNS to release norepinephrine from nerve terminals and increases the amounts of norepinephrine, dopamine, and possibly serotonin in the brain. Dopamine is released in higher doses. Dextroamphetamine suppresses appetite, increases alertness, elevates mood, and improves physical performance. The drug’s effectiveness and efficacy in ADHD is paradoxical, and its action is not well understood.
Use
The clinical indications for use of dextroamphetamine include the management of ADHD and narcolepsy. Amphetamines are useful in both acute and chronic conditions. Table 56.2 summarizes the route and dosage information for dextroamphetamine and other amphetamines.
 TABLE 56.2
TABLE 56.2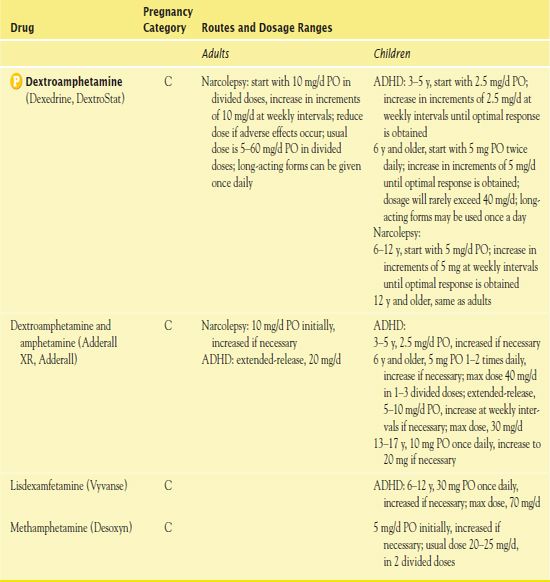
ADHD, attention deficit hyperactivity disorder.
Use in Children
Parents need to monitor their children’s use of medications for ADHD, and it is necessary to titrate the dosage carefully to avoid excessive CNS stimulation, anorexia, and insomnia. Suppression of weight and height (e.g., less than the estimated average of 2 inches per year) may occur, and the nurse ensures that growth is monitored during drug therapy. In children with psychosis or Tourette’s syndrome, CNS stimulants may exacerbate symptoms. In children and adolescents with preexisting heart disease, usual doses of dextroamphetamine may cause sudden death.
In ADHD, careful documentation of baseline symptoms over approximately 1 month is necessary to establish the diagnosis and evaluate outcomes of treatment. This may involve videotapes of behavior; observations and ratings by clinicians familiar with the condition; and by interviewing the child, parents, or caretakers. Some authorities believe that ADHD is overdiagnosed and that stimulant drugs are prescribed unnecessarily.
Use in Older Adults
The use of dextroamphetamine warrants caution in older adults. As with most other drugs, slowed metabolism and excretion increase the risks of accumulation and toxicity. Older adults are likely to experience anxiety, confusion, insomnia, and nervousness from excessive CNS stimulation. In addition, older adults often have cardiovascular disorders (e.g., angina, dysrhythmias, hypertension) that may be aggravated by the cardiac-stimulating effects of the drug. In general, reduced doses are safer in older adults.
Use in Patients With Renal or Hepatic Impairment
Dextroamphetamine is excreted in the urine after being metabolized in the liver. Thus, caution is necessary in patients with renal and/or hepatic impairment. The nurse monitors such patients for adverse effects and helps ensure that lower doses are used.
Adverse Effects
Dextroamphetamine has several adverse effects.
• Cardiovascular effects: tachycardia, other dysrhythmias, and hypertension. A BLACK BOX WARNING ♦ makes users aware of the drug’s high abuse potential; misuse may cause sudden death or serious cardiovascular events. It is essential to obtain a baseline electrocardiogram (ECG) and blood pressure reading.
• CNS effects: excessive CNS stimulation; possible anxiety, hyperactivity, nervousness, insomnia, tremors, convulsion, and psychotic behavior may occur. These reactions are more likely with larger doses.
• GI effects: gastritis, nausea, diarrhea, and constipation
• Other effects: anorexia and weight loss
Contraindications
Contraindications to dextroamphetamine include cardiovascular disorders (e.g., angina, dysrhythmias, hypertension), which are likely to be aggravated by the drug. Other contraindications include anxiety or agitation, glaucoma, and hyperthyroidism, as well as a history of drug abuse, pregnancy, or lactation.
Nursing Implications
Preventing Interactions
Many medications and herbs interact with dextroamphetamine, increasing or decreasing its effects (Boxes 56.1 and 56.2).
BOX 56.1  Drug Interactions: Dextroamphetamine
Drug Interactions: Dextroamphetamine
Drugs That Increase the Effects of Dextroamphetamine
 Albuterol, pseudoephedrine, tricyclic antidepressants
Albuterol, pseudoephedrine, tricyclic antidepressants
Increase stimulant effects of dextroamphetamine
 Antacids
Antacids
Decrease the excretion of amphetamines
 Monoamine oxidase inhibitors
Monoamine oxidase inhibitors
Enhance the hypertensive effects of amphetamines
Drugs That Decrease the Effects of Dextroamphetamine
 Ammonium chloride
Ammonium chloride
Decreases the serum concentration of dextroamphetamine
 Antipsychotics, lithium, alcohol
Antipsychotics, lithium, alcohol
Diminish the stimulant effect of dextroamphetamine
 Gastrointestinal acidifying agents
Gastrointestinal acidifying agents
Decrease the serum concentration of dextroamphetamine
BOX 56.2  Herbs and Dietary Interactions: Dextroamphetamine
Herbs and Dietary Interactions: Dextroamphetamine
Herbs and Foods That Increase the Effects of Dextroamphetamine
 Ephedra
Ephedra
Herbs and Foods That Decrease the Effects of Dextroamphetamine
 Acidic foods and juices, caffeine
Acidic foods and juices, caffeine
Administering the Medication
People should take the first dose of dextroamphetamine on awakening or early in the day and the last dose at least 6 hours before bedtime. Children with ADHD should take the drug 30 to 45 minutes before meals to minimize the appetite suppressing effects. It is important not to crush, chew, or bite the long-acting form; this destroys the extended-release feature and may result in an overdose. For young children who have difficulty swallowing pills, the capsules may be opened and taken with pudding or ice cream.
Dextroamphetamine often causes loss of appetite, and the health care provider may stop the medication during the months when the child is not in school. A drug holiday, as this is called, helps decrease weight loss and growth suppression. It may not be appropriate for every child.
Assessing for Therapeutic Effects
For patients with ADHD, the nurse assesses for improved behavior and performance of cognitive and psychomotor tasks. For patients with narcolepsy, the nurse assesses for fewer sleep attacks, increased mental alertness, and decreased mental fatigue.
Assessing for Adverse Effects
The nurse assesses for signs and symptoms of excessive CNS stimulation as evidenced by an inability to complete tasks due to nervousness and hyperactivity. It is necessary to check the patient’s cardiovascular status for tachycardia and elevation in blood pressure. The nurse assesses the patient’s diet for inability to eat and the patient for loss of weight. It is also important to assess the GI system for constipation or diarrhea.
Patient Teaching
Box 56.3 identifies patient teaching guidelines for drugs used in ADHD or narcolepsy.
BOX 56.3  Patient Teaching Guidelines for Drugs Used in Attention Deficit Hyperactivity Disorder and Narcolepsy
Patient Teaching Guidelines for Drugs Used in Attention Deficit Hyperactivity Disorder and Narcolepsy



