Define general anesthesia.
 Describe the three phases of general anesthesia.
Describe the three phases of general anesthesia.
 Describe the fundamental principles of balanced anesthesia.
Describe the fundamental principles of balanced anesthesia.
 Describe how inhalation anesthetics are delivered and describe how this process is different from intravenous anesthetics.
Describe how inhalation anesthetics are delivered and describe how this process is different from intravenous anesthetics.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the inhalation and intravenous general anesthetic agents.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the inhalation and intravenous general anesthetic agents.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the neuromuscular blocking agents.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the neuromuscular blocking agents.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the adjuvant medications administered to patients receiving general anesthesia.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the adjuvant medications administered to patients receiving general anesthesia.
 Implement the nursing process in the care of patients receiving general anesthesia.
Implement the nursing process in the care of patients receiving general anesthesia.
Clinical Application Case Study
Harriet Wilberson is a mildly obese 60-year-old woman with chronic cholecystitis and a history of allergic asthma. Despite dietary modification, she continues to have right abdomen pain, nausea, and bloating sensation. Ms. Wilberson believes that her numerous food allergies are the cause of these symptoms. She is scheduled for a laparoscopic cholecystectomy in an ambulatory surgical facility. Because Ms. Wilberson has an anaphylactic penicillin allergy, the surgeon has ordered preoperative intravenous gentamicin and clindamycin. The anesthesia provider has completed a preanesthetic evaluation and plans to administer a general endotracheal anesthetic. You are the nurse assigned to her care.
KEY TERMS
Amnesia: memory loss (of limited duration in anesthesia)
Balanced anesthesia: four elements of general anesthesia (amnesia, analgesia, hypnosis, and muscle relaxation) achieved by a combination of medications to produce a state of physiologic and pharmacologic equilibrium
Emergence: return to consciousness from general anesthesia
Fasciculation: transitory muscle contractions that occur after the administration of a depolarizing muscle relaxant
General anesthesia: medication-induced reversible unconsciousness with loss of protective reflexes
Hypnosis: unconsciousness
Induction: rendering the patient unconscious by using inhalation anesthetics, intravenous anesthetics, or both
Maintenance anesthesia: administering a continuous level of inhalation and/or intravenous anesthetic to sustain general anesthesia until the procedure is complete
Malignant hyperthermia: potentially fatal hypermetabolic response after exposure to volatile inhalation anesthetics or the drug succinylcholine
Minimum alveolar concentration: quantitative measure of the potency of inhalation anesthetics
Monitored anesthesia care: sedation administered by an anesthesia provider
Recurarization: residual weakness after assumed recovery from the effects of nondepolarizing muscle relaxants
Total intravenous anesthesia: a method of general anesthesia that replaces the inhalation agent with an intravenous anesthetic for the induction and maintenance of anesthesia
Introduction
In this chapter, you are introduced to the fundamentals of general anesthesia and the implementation of nursing care during the administration of general anesthesia. The administration of general anesthesia is a complex task that requires the expertise of a certified registered nurse anesthetist (CRNA), anesthesiologist (physician), or both. The CRNA and anesthesiologist may practice independently or as a team. They are physically present and actively providing care during the entire anesthetic process.
The goal of this chapter is to learn the basic aspects of anesthesia and anesthetic medications. With knowledge of anesthesia drug classes and their actions, the nurse is able to recognize adverse consequences and intervene to avoid detrimental outcomes. In some circumstances, complications arising from anesthesia can be immediately life threatening. For this reason, the operating room and postanesthesia care unit (PACU) must be a controlled environment to promote patient safety. The nurse must have an organized differential approach to clinical problems. It is necessary to provide life-saving interventions and then seek the cause of the difficulty. Airway, breathing, circulation, and supplemental oxygen, or ABC+O, is an important approach to all clinical problems. Fortunately, present-day anesthetic medications are generally safe with rapid onset and recovery. Because this chapter is not about medication therapy for a disease process, the content focuses on understanding the medications, adverse effects (or after effects), and nursing care.
Overview of General Anesthesia
General anesthesia is defined as a medication-induced reversible unconsciousness with loss of protective reflexes. There is the misconception that general anesthesia is a deep sleep. It is much deeper and more like a drug-induced coma. Arousal, even to painful stimuli, cannot occur. Therefore, it is possible to perform surgery or other unpleasant therapeutic or diagnostic procedures such as endoscopy or interventional radiology that would be unreasonable or impossible to accomplish in a conscious person.
Clinical Manifestations
The concept of using several drugs to achieve a state of physiologic and pharmacologic equilibrium under general anesthesia is called balanced anesthesia. Balanced anesthesia refers to the following four elements of general anesthesia designed to work collectively to produce a superior outcome:
1. Amnesia, or memory loss (of limited duration in anesthesia)
2. Analgesia, or a reduction or absence of pain
3. Hypnosis, or unconsciousness
4. Muscle relaxation, or immobility
Depending on the procedure, the anesthesia provider combines one or more of these elements by selecting appropriate medications. Generally, a major surgical procedure that requires tracheal intubation requires all of these elements to some degree.
Drug Therapy
Selection of anesthesia and adjuvant medications depends on a variety of conditions. This includes the requirements of the procedure, the patient’s age and health status, medical conditions, weight, drug allergies, the results of laboratory or diagnostic tests, and the patient’s preferences (if relevant). Using this information, the anesthesia provider develops a plan of care that maintains the patient’s; health and physiologic homeostasis.
The administration of a general anesthetic can be divided into three phases. The first phase is induction, which is rendering the patient unconscious by using inhalation anesthetics, intravenous anesthetics, or both. Adult patients usually receive a rapid-acting intravenous anesthetic medication. Pediatric patients more often breathe an inhalation anesthetic through a face mask. Called a mask induction, this allows an anesthesia provider or a nurse to perform the venipuncture for intravenous solutions after the patient is under general anesthesia. Before induction, the patient, whether adult or child, may receive a benzodiazepine that provides rapid anxiolytic and amnestic effects. The induction phase also includes securing and maintaining a patent airway.
The next phase is maintenance or maintenance anesthesia, which is administering a continuous level of inhalation and/or intravenous anesthetics until the procedure is complete. Adjunctive medications may be used at this time, such as antiemetics (see Chap. 36), opioids (see Chap. 48), and neuromuscular blocking agents.
The concluding phase is emergence. As the procedure ends, the general anesthetic medications are stopped, and the patient is permitted to wake up. As the patient emerges from the anesthetic, the anesthesia provider may use medications to reverse the effects of neuromuscular blocking agents. The patient is then transported to the PACU or perhaps the intensive care unit (ICU) for close observation, monitoring of vital signs and neurological status, and additional nursing or medical care.
Five drug classes are used to achieve balanced anesthesia: benzodiazepines, analgesics, inhalation anesthetics, intravenous anesthetics, and neuromuscular blocking agents. Benzodiazepines or inhalation anesthetics are used to achieve amnesia. Opioid or nonopioid medications are used to achieve analgesia. Inhalation or intravenous anesthetics are used to achieve hypnosis. Neuromuscular blocking agents and, to some extent, inhalation anesthetics are used to achieve muscle relaxation. Within each class, every medication has unique properties that determine onset, duration, elimination, and other characteristics. The anesthesia provider can select from several medications in each class to achieve balanced anesthesia. Knowledge of the synergistic, additive, or antagonistic effects of anesthetic medications helps decide the appropriate dose and combination.
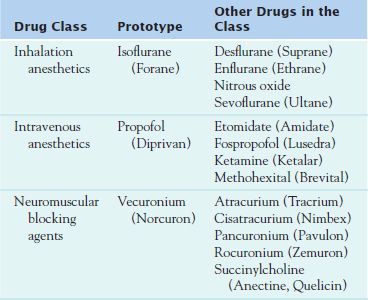
Table 50.1 lists the general anesthetics and neuromuscular blocking agents discussed in this chapter.
Inhalation Anesthetics
Inhalation anesthetics are volatile organic liquids administered by inhalation for induction and maintenance of general anesthesia. Volatile means having the ability to evaporate readily and release a gas. Today’s volatile inhalation anesthetics are halogenated ethers, which contain fluorine. The stability of the fluorine carbon bond helps reduce solubility, decreasing metabolism and organ toxicity.  Isoflurane (Forane), an extremely physically stable methyl ethyl ether, is the prototype inhalation anesthetic. Although not the first inhalation anesthetic introduced for clinical use, it deserves recognition for its wide acceptance. Its improved potency, low tissue solubility and metabolism, and chemical stability earned isoflurane the gold standard. Currently, it is the most potent inhalation anesthetic available. Isoflurane has a mild pungent or ethereal odor and can irritate the airways when concentration increases. Therefore, it does not lend itself to inhalation mask inductions. However, it makes an excellent maintenance anesthetic after using an intravenous induction medication.
Isoflurane (Forane), an extremely physically stable methyl ethyl ether, is the prototype inhalation anesthetic. Although not the first inhalation anesthetic introduced for clinical use, it deserves recognition for its wide acceptance. Its improved potency, low tissue solubility and metabolism, and chemical stability earned isoflurane the gold standard. Currently, it is the most potent inhalation anesthetic available. Isoflurane has a mild pungent or ethereal odor and can irritate the airways when concentration increases. Therefore, it does not lend itself to inhalation mask inductions. However, it makes an excellent maintenance anesthetic after using an intravenous induction medication.
Pharmacokinetics
Inhalation of isoflurane results in its delivery as a gas to the lungs. From there it diffuses rapidly into the arterial vascular system, travels throughout the vascular system, and crosses the blood–brain barrier. As the inhaled concentration of the anesthetic increases or decreases, the depth of anesthesia also changes. Several factors determine the speed of onset, but the desired level of anesthesia can be obtained in just a few minutes. The characteristics of intermediate solubility and high potency of isoflurane allow for easy regulation of the depth of anesthesia, and it is possible to sustain its effect on the brain without significant absorption into blood or body tissues. This means that induction and emergence are rapid.
Metabolism of isoflurane principally occurs in the liver, although some metabolism takes place in the kidney. Approximately 0.2% of the anesthetic undergoes complete metabolism. Therefore, absorption (uptake) and excretion are primarily through the alveoli and involve ventilation of the lungs. At the conclusion of the anesthesia, the patient receives 100% oxygen. This creates a reverse gradient, and the lungs eliminate the anesthetic. Awakening usually takes place within 10 minutes, and the patient is coherent within 15 to 30 minutes.
Action
Isoflurane produces amnesia, skeletal muscle relaxation, and hypnosis. It therefore blocks the perception of pain. Its ability to provide analgesia is unclear. The exact mechanism of action of inhalation anesthetics has not been established. However, the drug may amplify the effect of inhibitory neurotransmitter targets such as the gamma-aminobutyric acid (GABA) and glycine receptors. Activation of brain GABA receptors results in a loss of consciousness and amnesia, and the spinal cord glycine receptors cause immobility or absence of response to noxious stimuli. The action of inhalation anesthetics also involves the antagonism of excitatory N-methyl-D-aspartate (NMDA) receptors and possibly other unidentified molecular sites.
Isoflurane produces a dose-dependent change in several organ systems. As the isoflurane concentration increases, the blood pressure decreases and the heart rate may increase. The respiratory rate increases, but the tidal volume diminishes. If necessary, this is reversed by the anesthesia provider with assisted ventilation. There is minimal bronchodilation. Once the patient emerges from general anesthesia, the depressant effects normally resolve within 30 minutes. Therefore, residual effects may be observed in the PACU. In addition, as concentration increases, there is progressive skeletal muscle relaxation likely due to the effect on spinal cord glycine receptors. This enhances the action of neuromuscular blocking agents.
Use
Isoflurane is indicated for the induction and maintenance of general anesthesia in people of all ages, in those who are healthy, and in those who are critically ill. It can be used alone to maintain general anesthesia or more commonly in combination with other agents to produce balanced anesthesia. Table 50.2 summarizes the use of the inhalation anesthetic agents.
 TABLE 50.2
TABLE 50.2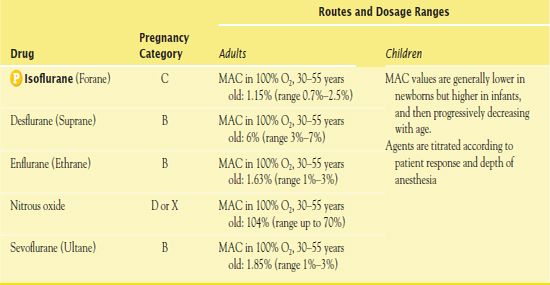
MAC, minimum alveolar concentration.
Use in Patients With Renal Impairment
Isoflurane reduces renal blood flow and urine output. Adequate hydration during the perioperative period maintains normal renal function. Therefore, administration of isoflurane to patients with renal impairment or insufficiency is considered safe.
Use in Patients With Hepatic Impairment
Isoflurane is associated with very mild and brief postoperative hepatic dysfunction. Any disease that impairs liver function such as hepatic cirrhosis may place the patient at risk. The incidence of hepatotoxicity is rare. Therefore, isoflurane can be administered to patients with hepatic disease.
Adverse Effects
Inhalation anesthetics such as isoflurane are associated with cardiovascular and respiratory depression. They can also cause airway irritation and progress to coughing, laryngospasm, or bronchospasm in susceptible patients such as smokers or asthmatics. In addition, inhalation anesthetics are known to cause vomiting, especially after 2 or more hours of exposure.
There is also a very rare possibility of immune-mediated hepatotoxicity that can result in death. Although all halogenated inhalation anesthetics can produce hepatic injury, this phenomenon was usually associated with halothane, which has been discontinued. In the obstetrical patient, all volatile inhalation anesthetics, including isoflurane, decrease the tone of uterine smooth muscle, making it susceptible to bleeding during surgery such as caesarean section. Additionally, an alteration in the thermoregulatory system with or without hypothermia may cause shivering after emergence.
Malignant hyperthermia, a genetic disorder, is a potentially fatal hypermetabolic response after exposure to volatile inhalation anesthetics or to the neuromuscular blocking agent succinylcholine. Several myopathies such as muscular dystrophy have a predisposition to malignant hyperthermia. The presentation of malignant hyperthermia may be highly variable, and the response time may be immediate or delayed. The signs include tachycardia, elevated temperature, body rigidity, mixed metabolic and respiratory acidosis, mottling and sweating, masseter spasm (rigid jaw), hyperkalemia, elevated creatine kinase (CK), myoglobinuria, and renal failure. The treatment consists of intravenous dantrolene sodium (Dantrium) (see Chap. 52), oxygenation and hyperventilation, hydration, and body cooling. Additional medications are necessary to treat the acidosis, hyperkalemia, and dysrhythmias and to prevent renal failure. After recognition, therapy must begin immediately to avoid poor outcome.
Contraindications
If there is an actual or suggestive family history of malignant hyperthermia, or disease processes associated with malignant hyperthermia, the anesthesia provider will not use a volatile anesthetic. Patients with a history of hepatic dysfunction after exposure to halogenated inhalation anesthetics or those at risk for developing a sensitivity reaction should not receive isoflurane. If a patient reports that he or she is allergic to general anesthesia, the anesthesia provider will attempt to determine the specific reaction. The avoidance of inhalation anesthetics may be necessary. In patients who have history of severe postoperative nausea and vomiting, the anesthetist may substitute the inhalation anesthetic with a technique called total intravenous anesthesia (TIVA). TIVA replaces the inhalation agent with a less emetic and nonmalignant hyperthermia triggering intravenous anesthetic for the induction and maintenance of anesthesia.
QSEN Safety Alert 
With the exception of cesarean section, surgery while pregnant would be performed to save life, limb, or eyesight. The benefits of surgery (e.g., to save life, limb, or sight) must outweigh the risks. Therefore, a preoperative pregnancy test is routinely ordered in women of childbearing age. The anesthesia provider designs effective strategies and tailors the anesthetic to avoid the possibility of patient harm and fetal teratogenicity.
The more advanced the pregnancy, the smaller the chance that the medications and inhalation anesthetics affect the unborn child. Authorities generally agree that anesthesia and surgery after the first trimester can be conducted in a safe manner and that the risk of fetal teratogenicity is minimal to nonexistent. Both the nurse and anesthesia provider serve as an advocate and minimize the possibility of harm to the patient and unborn child.
Nursing Implications
Anesthesia providers use inhalation anesthetics widely in their daily practice. The choice of inhalation anesthetic is based on several factors such as the pharmacokinetic profile, preexisting medical conditions, and history of previous reactions.
Preventing Interactions
Isoflurane combined with dopamine, ephedrine, epinephrine, isoproterenol, or norepinephrine may be capable of producing cardiac dysrhythmias. Alcohol and some herbs may increase the effect of isoflurane (Box 50.1).
BOX 50.1  Herb Interactions and Dietary Interactions: Isoflurane and Propofol
Herb Interactions and Dietary Interactions: Isoflurane and Propofol
Herbs and Foods That May Increase the Effect of Isoflurane and Propofol
 Alcohol
Alcohol
 Kava
Kava
 St. John’s Wort
St. John’s Wort
 Valerian Root
Valerian Root
Administering the Medication
The administration of inhalation anesthetics requires the use of an anesthesia machine. These devices vary in features and sophistication. It only takes a very small amount of anesthetic (1%–3%) to produce general anesthesia. The mixture of agents is delivered to the patient’s lungs through a plastic breathing circuit that connects to a mask, endotracheal tube, or supraglottic airway device such as the laryngeal mask airway.
The term minimum alveolar concentration (MAC) is a quantitative measure of the potency of an anesthetic. It is the concentration of anesthetic necessary to suppress a response to pain in 50% of patients who receive a noxious stimulus such as a surgical incision. The MAC values vary with the age of the patient. Furthermore, MAC values are additive. With the addition of other medications such as opioids, intravenous anesthetics, or nitrous oxide, the MAC values decrease. For example, the MAC of isoflurane is 1.15% in adults when it is administered alone. However, when in combination with 70% nitrous oxide, the MAC of isoflurane decreases to 0.5%.
Assessing for Therapeutic Effects
Assessing the patient for the therapeutic effects of inhalation anesthetics is the responsibility of the anesthesia provider.
Assessing for Adverse Effects
Because inhalation anesthetics may lead to low blood pressure and respiratory depression, it is prudent to provide oxygen and frequently assess the blood pressure and quality of breathing or ventilation early in the postoperative period. Monitoring oxygen saturation as measured by pulse oximetry helps guide therapy. The nurse may treat postoperative shivering with warm blankets or forced-air warming devices. Nausea and vomiting may occur after surgery using isoflurane. Treatment involves antiemetics (see Chap. 36). If there are symptoms suspicious of malignant hyperthermia, it is imperative that the nurse notify the anesthesia provider immediately.
Patient Teaching
Box 50.2 identifies patient teaching guidelines for the inhalation anesthetics, including isoflurane.
BOX 50.2  Patient Teaching Guidelines for General Anesthetics
Patient Teaching Guidelines for General Anesthetics
 Ask your health care provider for information about the administration and effects of the general anesthetic agent(s) you may receive. Feel free to ask questions. Learn about the postoperative/postprocedural recovery phase.
Ask your health care provider for information about the administration and effects of the general anesthetic agent(s) you may receive. Feel free to ask questions. Learn about the postoperative/postprocedural recovery phase.
 If you will be receiving an intravenous anesthetics such as propofol, be aware that there may be pain, burning, or stinging when the medication is injected into the intravenous catheter and flows into the vein. (Preinduction narcotics and simultaneous administration of intravenous lidocaine also help relieve the discomfort.)
If you will be receiving an intravenous anesthetics such as propofol, be aware that there may be pain, burning, or stinging when the medication is injected into the intravenous catheter and flows into the vein. (Preinduction narcotics and simultaneous administration of intravenous lidocaine also help relieve the discomfort.)
 Refrain from smoking prior to surgery.
Refrain from smoking prior to surgery.
 Discontinue complementary and alternative medicine products, including herbal supplements, for 2 weeks prior to surgery.
Discontinue complementary and alternative medicine products, including herbal supplements, for 2 weeks prior to surgery.
 Do not ingest alcohol for 24 hours prior to their scheduled surgery or procedure.
Do not ingest alcohol for 24 hours prior to their scheduled surgery or procedure.
 Ask your health care provider about diagnostic testing to screen for malignant hyperthermia or atypical plasma cholinesterase if you have a family history.
Ask your health care provider about diagnostic testing to screen for malignant hyperthermia or atypical plasma cholinesterase if you have a family history.
Other Drugs in the Class
Several other inhaled anesthetic agents are available. The introduction of desflurane (Suprane) in 1992 and sevoflurane (Ultane) in 1994 represented a new era of completely fluorinated ethers. These inhalation anesthetics further reduce body tissue solubility and allow rapid induction and emergence from anesthesia. They are valuable adjuncts in today’s extensive practice of ambulatory surgery.
Desflurane (Suprane) is a completely fluorinated methyl ethyl ether. Of the currently available inhalation anesthetics, it is the least soluble and least potent. These characteristics favor rapid induction and emergence, return of protective airway reflexes, and negligible metabolism. Patients benefit from faster recovery and return of normal cognition. However, desflurane is very pungent, making mask inhalation induction impractical. Moreover, desflurane produces airway irritation and increases the incidence of coughing, breath holding, or laryngospasm. Unlike other inhalation anesthetics, desflurane may cause mild bronchoconstriction.
Enflurane (Ethrane) is a potent methyl ethyl ether that has a profile similar to isoflurane. It is slightly more soluble, and therefore the induction and emergence is somewhat slower. Unfortunately, enflurane has two limitations. First, it may promote seizures at high concentrations. Second, its metabolism to fluoride carries a risk of nephrotoxicity. Therefore, it is contraindicated in patients with epilepsy or diminished renal function.
Sevoflurane (Ultane) is a completely fluorinated methyl isopropyl ether that has about half the potency of isoflurane. Its solubility is extremely low. Therefore, induction, emergence, and recovery are fast. In addition, sevoflurane is nonpungent and results in the least amount of airway irritation. It provides a pleasant inhalation mask induction in both adults and children without the need of an initial intravenous anesthetic. Furthermore, it produces bronchodilation similar or perhaps greater than isoflurane. These properties make sevoflurane a popular choice for patients with reactive airway disease or chronic obstructive pulmonary disease. In young children, sevoflurane is associated with emergence or postoperative agitation but does not seem to have long-term implications.
In addition to the volatile anesthetics, the inorganic inhalation agent nitrous oxide is commonly used in combination with other anesthetic medications. Also known as laughing gas, it is not a volatile agent like isoflurane because it is a gas at room temperature. Unfortunately, the potency of nitrous oxide is low, and it cannot produce general anesthesia by itself. However, its additive effect will permit a lower concentration or dose of the volatile or intravenous anesthetics. Nitrous oxide produces amnesia, analgesia, and euphoria. Because it has a greater solubility in blood than nitrogen, it diffuses into closed body cavities and expands. This can place undue pressure in the bowels, middle ear, and other spaces created by surgery or disease. As a result, it is contraindicated in many types of surgeries and preexisting medical conditions. Nitrous oxide is also implicated in exacerbating postoperative nausea and vomiting, possibly due to gas expansion in the bowel.
NCLEX Success
1. The nurse is circulating in the operating room when the anesthesia provider declares a malignant hyper thermia emergency. Which of the following symptoms are indicative of malignant hyperthermia?
A. muscle rigidity
B. bradycardia
C. hypokalemia
D. increased serum creatinine
2. A 32-year-old woman is admitted to the hospital with right lower quadrant abdominal pain. She has a history of absence seizures. Which of the following inhalation anesthetic agents is contraindicated?
A. isoflurane
B. sevoflurane
C. desflurane
D. enflurane



