Understand the pathophysiology and major manifestations of myasthenia gravis.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for indirect-acting cholinergic drugs used in myasthenia gravis.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for indirect-acting cholinergic drugs used in myasthenia gravis.
 Understand the pathophysiology and major manifestations of Alzheimer’s disease.
Understand the pathophysiology and major manifestations of Alzheimer’s disease.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for reversible indirect-acting cholinergic drugs used in Alzheimer’s disease.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for reversible indirect-acting cholinergic drugs used in Alzheimer’s disease.
 Understand the etiology, pathophysiology, and clinical manifestations of urinary retention.
Understand the etiology, pathophysiology, and clinical manifestations of urinary retention.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for direct-acting cholinergic drugs.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for direct-acting cholinergic drugs.
 Describe the pharmacologic care of the patient with toxicity of irreversible anticholinesterase agents.
Describe the pharmacologic care of the patient with toxicity of irreversible anticholinesterase agents.
 Be able to implement the nursing process in the care of patients undergoing cholinergic drug therapy for myasthenia gravis, Alzheimer’s disease, and urinary retention.
Be able to implement the nursing process in the care of patients undergoing cholinergic drug therapy for myasthenia gravis, Alzheimer’s disease, and urinary retention.
Clinical Application Case Study
Mary Collins, a 35-year-old woman, who has recently been diagnosed with myasthenia gravis, arrives in the clinic. She has been quite upset about her diagnosis and has lost interest in everyday life. On assessment, the nurse notes that Ms. Collins has shortness of breath, difficulty swallowing, and a drooping eyelid on the left side. Her physician has ordered sertraline and neostigmine 50-mg extended-release tablets to control her symptoms.
KEY TERMS
Acetylcholine: neurotransmitter in the cholinergic system located in many areas of the brain, with high concentrations in the motor cortex and basal ganglia (also a neurotransmitter in the autonomic nervous system and at peripheral neuromuscular junctions); exerts excitatory effects at synapses and at the nerve-muscle junction and inhibitory effects at some peripheral sites, such as organs supplied by the vagus nerve
Acetylcholinesterase: enzyme that acts on the neurotransmitter acetylcholine, breaking it into choline and an acetate group; found mainly at neuromuscular junctions, its activity serves to terminate synaptic transmission
Alzheimer’s disease: most common type of dementia; characterized by a significant loss of neurons in addition to shrinkage of large cortical neurons, with plaques and neurofibrillary tangles
Anticholinesterase drugs: indirect-acting cholinergic agents that decrease the inactivation of acetylcholine in the synapse by the enzyme acetylcholinesterase
Cholinergic drugs: agents that stimulate the parasympathetic nervous system in the same manner as acetylcholine
Myasthenia gravis: chronic autoimmune neuromuscular disease characterized by varying degrees of weakness of the skeletal (voluntary) muscles of the body
Introduction
The neuromuscular conditions myasthenia gravis and Alzheimer’s disease are characterized by disruptions in neurological and autoimmune processes. This chapter discusses the anticholinesterase medications used for the treatment of myasthenia gravis as well as the medications used to improve memory related to Alzheimer’s disease. It also covers selected drugs used to treat atony of the gastrointestinal (GI) and urinary smooth muscle, which may result in paralytic ileus and urinary retention.
Overview of Myasthenia Gravis
Myasthenia gravis is a chronic autoimmune neuromuscular disease characterized by varying degrees of painless weakness of the skeletal (voluntary) muscles of the body. The hallmark of the disorder is muscle weakness that increases during periods of activity and improves after periods of rest. The name myasthenia gravis, which is Latin and Greek in origin, literally means “grave muscle weakness.” With the therapies currently available, however, most cases of myasthenia gravis are not as “grave” as the name implies. In fact, most people who have myasthenia gravis have a normal life expectancy.
Myasthenia gravis occurs in all ethnic groups and both genders. It most commonly affects young adult women (younger than 40 years of age) and older men (older than 60 years of age), but it can occur at any age.
Etiology
Myasthenia gravis results from a defect in the transmission of nerve impulses to muscles. Normally, when impulses travel down the nerve, the nerve endings release a neurotransmitter called acetylcholine. Acetylcholine travels from the neuromuscular junction and binds to acetylcholine receptors, which are activated and generate a muscle contraction.
Pathophysiology
Myasthenia gravis occurs when normal communication between the nerve and muscle is interrupted at the neuromuscular junction—the place where nerve cells connect with the muscles they control. Antibodies produced by the body’s own immune system block, alter, or destroy the receptors for acetylcholine at the neuromuscular junction, which prevents muscle contraction from occurring. Because the immune system, which normally protects the body from foreign organisms, mistakenly attacks itself, myasthenia gravis is known as an autoimmune disease.
Clinical Manifestations
Although myasthenia gravis may affect any voluntary muscle, muscles that control eye and eyelid movement, facial expression, and swallowing are most frequently affected. The onset of the disorder may be sudden, and symptoms often are not immediately recognized as myasthenia gravis. In most cases, the first noticeable symptom is weakness of the eye muscles. In others, difficulty in swallowing and slurred speech may be the first signs. The degree of muscle weakness involved in myasthenia gravis varies greatly among people, ranging from a localized form limited to eye muscles (ocular myasthenia) to a severe or generalized form in which many muscles—sometimes including those that control breathing—are affected.
Symptoms, which vary in type and severity, may include a drooping of one or both eyelids (ptosis), blurred or double vision (diplopia) due to weakness of the muscles that control eye movements, unstable or waddling gait, a change in facial expression, difficulty in swallowing, shortness of breath, impaired speech (dysarthria), and weakness in the arms, hands, fingers, legs, and neck.
Drug Therapy
Cholinergic drugs stimulate the parasympathetic nervous system in the same manner as acetylcholine. The cholinergic drugs described in this chapter act indirectly by inhibiting the enzyme acetylcholinesterase, thereby slowing acetylcholine metabolism at autonomic nerve synapses. Other drugs act directly to stimulate cholinergic receptors (Fig. 46.1).
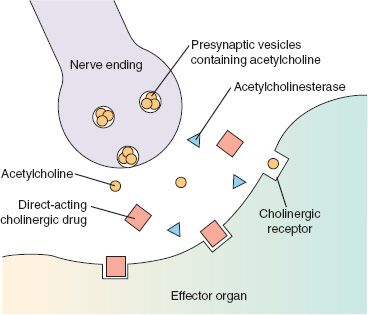
Figure 46.1 Mechanism of direct cholinergic drug action. Direct-acting cholinergic drugs interact with postsynaptic cholinergic receptors on target effector organs, activating the organ in a similar fashion as the neurotransmitter acetylcholine.
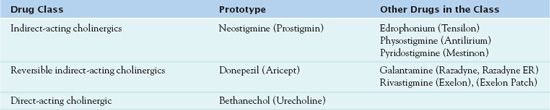
Anticholinesterase drugs are classified as either reversible or irreversible inhibitors of acetylcholinesterase. The reversible inhibitors exhibit a moderate duration of action and have several therapeutic uses—in myasthenia gravis and, as described later in this chapter, in Alzheimer’s disease. Table 46.1 lists medications used to treat myasthenia gravis.
Clinical Application 46-1
 What does the nurse teach Ms. Collins about the pathophysiology of myasthenia gravis?
What does the nurse teach Ms. Collins about the pathophysiology of myasthenia gravis?
 What information does the nurse provide to Ms. Collins about the signs and symptoms she is experiencing?
What information does the nurse provide to Ms. Collins about the signs and symptoms she is experiencing?
Indirect-Acting Cholinergics
The anticholinesterase drug  neostigmine (Prostigmin) is the prototype drug in this class. Health care providers use this drug for the long-term treatment of myasthenia gravis and as an antidote for tubocurarine and other nondepolarizing skeletal muscle relaxants used in surgery.
neostigmine (Prostigmin) is the prototype drug in this class. Health care providers use this drug for the long-term treatment of myasthenia gravis and as an antidote for tubocurarine and other nondepolarizing skeletal muscle relaxants used in surgery.
Pharmacokinetics
Neostigmine is available in an oral preparation, and absorption in the GI tract is poor. An intravenous (IV) form is available (for muscle spasms). The onset of action is 20 to 30 minutes for the oral form and 15 minutes for the IV form. The half-life is 50 to 90 minutes. Metabolism occurs in the liver, and the drug does not appear to cross the placenta easily. Excretion occurs in the kidneys.
Action
Neostigmine decreases the inactivation of acetylcholine in the synapse by the enzyme acetylcholinesterase. Thus, acetylcholine accumulates in the synapse and enhances the activation of postsynaptic muscarinic as well as nicotinic receptors (Fig. 46.2). In addition to the cholinergic drug effects described above, the added effect of indirect-acting cholinergic drugs on nicotinic receptors in skeletal muscles results in improved skeletal muscle tone and strength.
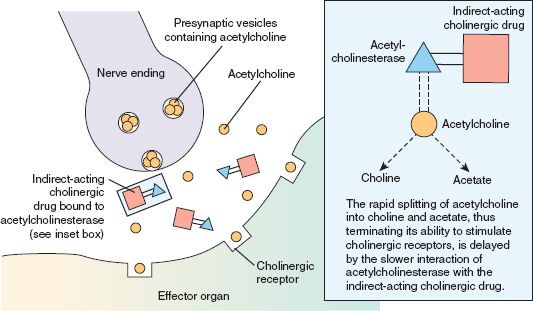
Figure 46.2 Mechanism of indirect cholinergic drug action. Indirect-acting cholinergic drugs prevent the enzymatic breakdown of the neurotransmitter acetylcholine. The acetylcholine remains in the synapse and continues to interact with cholinergic receptors on target effector organs, producing a cholinergic response.
In a patient with myasthenia gravis, specific effects of neostigmine include decreasing the heart rate, increasing the tone of GI smooth muscle, and stimulating the salivary glands to increase secretions. In addition, this drug increases tone and contractility of smooth muscle (detrusor) in the urinary bladder and relaxes the sphincter and bronchial smooth muscles (see Fig. 46.2).
Use
The major use of neostigmine is in the diagnosis and treatment of myasthenia gravis. In addition, prescribers order it to reverse the action of nondepolarizing neuromuscular blocking agents, such as tubocurarine, which is used in surgery. Neostigmine does not reverse the neuromuscular blockade produced by depolarizing neuromuscular blocking agents such as succinylcholine.
Table 46.2 presents dosage information for neostigmine and related drugs.
 TABLE 46.2
TABLE 46.2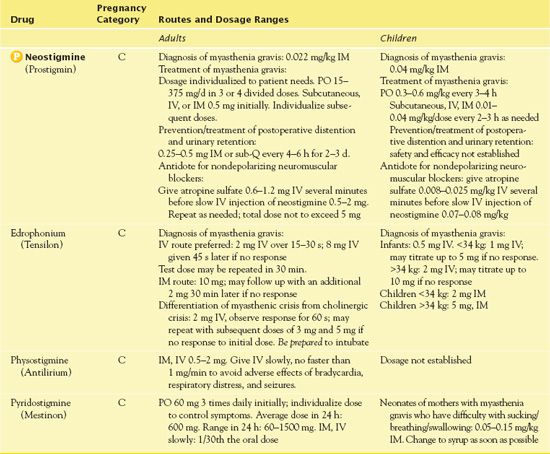
Use in Older Adults
Older adults are more likely to experience adverse drug effects because of age-related physiologic changes and superimposed pathologic conditions.
Use in Patients With Renal Impairment
Neostigmine undergoes tubular excretion in the kidneys. Therefore, renal impairment may result in accumulation and increased adverse effects, especially with chronic use. It is necessary to monitor patients with renal impairment and urinary obstruction carefully and give the drug at the lowest possible loading dose.
Use in Patients With Hepatic Impairment
Neostigmine undergoes metabolism in the liver, and hepatic disease may interfere with this, resulting in increased adverse effects. However, no dosage adjustments are necessary in patients with hepatic impairment.
Use in Patients With Critical Illness
Neostigmine has specific uses in critical illness. These include reversal of skeletal muscle paralysis caused by nondepolarizing muscle relaxants, improvement of muscle strength, and use as an antidote to anticholinergic poisoning. In this last case, drugs such as atropine or tricyclic antidepressants are also required.
Use in Patients Receiving Home Care
Use of neostigmine in the home involves the treatment of long-term conditions such as myasthenia gravis. Self-administration may be a problem for the patient, who may have diplopia or diminished muscle strength. Strict adherence to timely medication administration promotes optimal blood levels of drugs and optimal symptom control. In the event the patient develops muscle weakness, it is essential that the primary care provider be notified immediately.
Adverse Effects
Specific Effects
Neostigmine has several adverse effects. Cardiovascular adverse effects of neostigmine are cardiac dysrhythmias, diminished cardiac output, hypotension, syncope, and cardiac arrest. Development of respiratory depression indicates cholinergic crisis. Other respiratory adverse effects include increased pharyngeal and tracheobronchial secretions, laryngospasm, bronchospasm, bronchiolar constriction, shortness of breath, and respiratory paralysis. (IV atropine sulfate is the specific antidote for cholinergic agents.) Conditions such as excessive salivation, nausea, emesis, frequent urination, or diarrhea require a reduction in dosage.
Toxicity of Neostigmine and Other Indirect-Acting Anticholinergics
Cholinergic crisis is a drug-induced overstimulation of the parasympathetic nervous system, requiring discontinuation of any anticholinesterase drug that the patient has been receiving. Atropine sulfate should be readily available whenever cholinergic drugs are given. It is important to note that atropine reverses only the muscarinic effects of cholinergic drugs, primarily in the heart, smooth muscle, and glands. Atropine does not interact with nicotinic receptors and therefore cannot reverse the nicotinic effects of skeletal muscle weakness due to overdose of indirect anticholinergic drugs.
Atropine sulfate is also administered for the management of mushroom poisoning. Muscarine, an alkaloid that is found in small quantities in the Amanita muscaria mushroom, is the source of the name for the muscarinic receptors in the parasympathetic nervous system; muscarine can stimulate these receptors. Some mushrooms found in North America, such as Clitocybe and lnocybe mushrooms, however, contain much larger quantities of muscarine. Accidental or intentional ingestion of these mushrooms results in cholinergic crisis and is potentially fatal.
Contraindications
Contraindications to neostigmine include known hypersensitivity. Patients with lung disease, such as bronchial asthma, or heart disease, such as sick sinus syndrome, should not take the drug. In addition, it is necessary to use caution with patients with benign prostatic hypertrophy and other urinary retention problems.
Nursing Implications
Preventing Interactions
Several drugs interact with neostigmine (Box 46.1), increasing or decreasing its effects.
BOX 46.1  Drug Interactions: Neostigmine
Drug Interactions: Neostigmine
Drugs That Increase the Effects of Neostigmine
 Aminoglycoside antibiotics (e.g., gentamicin)
Aminoglycoside antibiotics (e.g., gentamicin)
Increase neuromuscular blocking
Drugs That Decrease the Effects of Neostigmine
 Atropine
Atropine
Decreases the effects of neostigmine by unknown
 mechanism
mechanism
 Corticosteroids
Corticosteroids
May result in muscular depression
Administering the Medication
When administering neostigmine, it is necessary to give the drug with food or fluid and not to crush extended-release forms. It is important to administer IV neostigmine slowly and have atropine available as an antidote in the event of a cholinergic crisis or hypersensitivity to neostigmine.
QSEN Safety Alert 
When administering neostigmine to older patients, it is essential to observe for signs of cholinergic reactions, particularly when the drug is given IV. Treatment for myasthenic crisis includes administration of additional anticholinesterase medications and measures to maintain respirations until the medications are effective in improving muscle strength.
Assessing for Therapeutic Effects
The nurse assesses the patient’s response to the medication. When neostigmine is given to patients with myasthenia gravis, it is necessary to observe for increased muscle strength; decreased difficulty with chewing, swallowing, and speech; and decreased or absent ptosis of eyelids.
Assessing for Adverse Effects
The nurse assesses for increased central nervous system (CNS) effects such as convulsions, dizziness, and drowsiness. He or she assesses for increased secretions, bronchospasm, laryngospasm, and respiratory failure. It is necessary to assess for nausea and vomiting, which are common GI effects. In addition, the nurse observes neonates of mothers with myasthenia gravis who have received neostigmine for difficulty breathing, swallowing, or sucking.
Patient Teaching
Box 46.2 identifies patient teaching guidelines for neostigmine.
BOX 46.2  Patient Teaching Guidelines for Neostigmine
Patient Teaching Guidelines for Neostigmine
 Wear a medical alert identification device if you are taking long-term cholinergic drug therapy for myasthenia gravis.
Wear a medical alert identification device if you are taking long-term cholinergic drug therapy for myasthenia gravis.
 Record symptoms of myasthenia gravis and effects of drug therapy, especially when drug therapy is initiated and medication doses are being titrated. The amount of medication required to control symptoms of myasthenia gravis varies greatly, and the physician needs this information to adjust the dosage correctly.
Record symptoms of myasthenia gravis and effects of drug therapy, especially when drug therapy is initiated and medication doses are being titrated. The amount of medication required to control symptoms of myasthenia gravis varies greatly, and the physician needs this information to adjust the dosage correctly.
 Do not overexert yourself if you have myasthenia gravis. Rest between activities. Although the dose of medication may be increased during periods of increased activity, it is desirable to space activities to obtain optimal benefit from the drug, at the lowest possible dose, with the fewest adverse effects.
Do not overexert yourself if you have myasthenia gravis. Rest between activities. Although the dose of medication may be increased during periods of increased activity, it is desirable to space activities to obtain optimal benefit from the drug, at the lowest possible dose, with the fewest adverse effects.
 Report increased muscle weakness, difficulty breathing, or recurrent of myasthenic symptoms to your physician. These are signs of drug underdosage (myasthenic crisis) and indicate a need to increase or change drug therapy.
Report increased muscle weakness, difficulty breathing, or recurrent of myasthenic symptoms to your physician. These are signs of drug underdosage (myasthenic crisis) and indicate a need to increase or change drug therapy.
 Report adverse reactions, including abdominal cramps, diarrhea, excessive oral secretions, difficulty in breathing, and muscle weakness. These are signs of drug overdosage (cholinergic crisis) and require immediate discontinuation of drugs and treatment by a physician. Respiratory failure can result if this condition is not recognized and treated properly. Atropine may be administered for overdose of cholinergic drugs.
Report adverse reactions, including abdominal cramps, diarrhea, excessive oral secretions, difficulty in breathing, and muscle weakness. These are signs of drug overdosage (cholinergic crisis) and require immediate discontinuation of drugs and treatment by a physician. Respiratory failure can result if this condition is not recognized and treated properly. Atropine may be administered for overdose of cholinergic drugs.
Clinical Application 46-2
 Ms. Collins takes her neostigmine 50-mg extended-release tablet one morning. At 2:00 PM, she develops nausea and becomes diaphoretic. She calls the home care nurse about her symptoms. What does the nurse suspect has contributed to the development of these symptoms?
Ms. Collins takes her neostigmine 50-mg extended-release tablet one morning. At 2:00 PM, she develops nausea and becomes diaphoretic. She calls the home care nurse about her symptoms. What does the nurse suspect has contributed to the development of these symptoms?
 Ms. Collins continues to take the 50-mg extended-release tablets. One week later, the home care nurse visits and finds that her respirations are very shallow at a rate of 8 breaths per minute. Based on this assessment, what does the nurse suspect is wrong with the patient?
Ms. Collins continues to take the 50-mg extended-release tablets. One week later, the home care nurse visits and finds that her respirations are very shallow at a rate of 8 breaths per minute. Based on this assessment, what does the nurse suspect is wrong with the patient?
 The home care nurse calls 9-1-1. She informs the paramedics of Ms. Collins diagnosis of myasthenia gravis and the medications she is taking. What medication do the paramedics administer?
The home care nurse calls 9-1-1. She informs the paramedics of Ms. Collins diagnosis of myasthenia gravis and the medications she is taking. What medication do the paramedics administer?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


