Examine the roles of parathyroid hormone, calcitonin, and vitamin D in regulating calcium metabolism.
 Evaluate the use of calcium and vitamin D supplements, as well as calcitonin, in the treatment of osteoporosis.
Evaluate the use of calcium and vitamin D supplements, as well as calcitonin, in the treatment of osteoporosis.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of the bisphosphonates used in the treatment of osteoporosis.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of the bisphosphonates used in the treatment of osteoporosis.
 Outline appropriate management strategies of hypercalcemia as a medical emergency.
Outline appropriate management strategies of hypercalcemia as a medical emergency.
 Implement the nursing process in the care of the patient receiving drug therapy to regulate calcium and bone metabolism.
Implement the nursing process in the care of the patient receiving drug therapy to regulate calcium and bone metabolism.
Clinical Application Case Study
Carolyn Taylor, a 68-year-old retired teacher, has chronic venous insufficiency and osteoporosis. She has suffered two fractures from falls in recent years. Mrs. Taylor has been menopausal for 1 6 years and has not been on estrogen replacement therapy due to her vascular disease. Her health care provider prescribes alendronate once weekly.
KEY TERMS
Bisphosphonates: class of drugs that binds to bone and inhibits calcium resorption from bone
Calcitonin: hormone from the thyroid gland whose secretion is controlled by the concentration of ionized calcium in the blood flowing through the thyroid gland; lowers serum calcium in the presence of hypercalcemia
Hypercalcemia: abnormally high blood calcium level (greater than 10.5 mg/dL)
Hypocalcemia: abnormally low blood calcium level (less than 8.5 mg/dL)
Hyperparathyroidism: excessive production of parathyroid hormone (PTH)
Hypoparathyroidism: insufficient production of PTH
Osteoporosis: decreased bone density and weak, fragile bones that often lead to fractures, pain, and disability
Paget’s disease: inflammatory skeletal disease that affects older people
Parathyroid hormone (PTH): hormone secreted by the parathyroid glands; secretion is stimulated by low serum calcium levels and inhibited by normal or high levels
Tetany: neuromuscular irritability characterized by numbness and tingling of the lips, fingers, and toes; twitching of facial muscles; spasms of skeletal muscle; carpopedal spasm; laryngospasm; and convulsions
Vitamin D (calciferol): fat-soluble vitamin that includes both ergocalciferol (obtained from foods) and cholecalciferol (formed by exposure of skin to sunlight); functions as a hormone and plays an important role in calcium and bone metabolism
Introduction
Three hormones regulate calcium and bone metabolism— parathyroid hormone, calcitonin, and vitamin D—and act to maintain normal serum levels of calcium. When serum calcium levels are decreased, hormonal mechanisms raise them; when they are elevated, hormonal mechanisms lower them (Fig. 42.1). Overall, the hormones alter absorption of dietary calcium from the gastrointestinal (GI) tract, movement of calcium from bone to serum, and excretion of calcium through the kidneys.
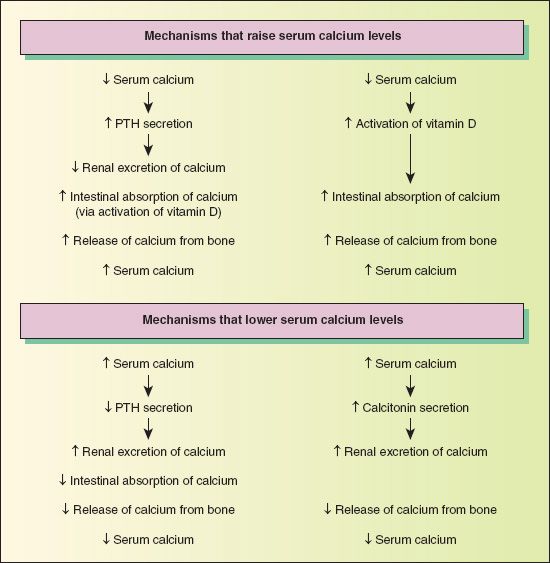
Figure 42.1 Hormonal regulation of serum calcium levels. When serum calcium levels are low (hypocalcemia), there is increased secretion of parathyroid hormone (PTH) and increased activation of vitamin D. These mechanisms lead to decreased loss of calcium in the urine, increased absorption of calcium from the intestine, and increased resorption of calcium from bone. These mechanisms work together to raise calcium levels to normal.
When serum calcium levels are high (hypercalcemia), there is decreased secretion of PTH and increased secretion of calcitonin. These mechanisms lead to increased loss of calcium from the intestine and decreased resorption of calcium from bone. These mechanisms lower serum calcium levels to normal.
Disorders of calcium and bone metabolism include hypocalcemia, hypercalcemia, osteoporosis, Paget’s disease, and bone breakdown associated with breast cancer and multiple myeloma. Drugs used to treat these disorders mainly alter serum calcium levels or strengthen bone. This chapter describes the characteristics of the hormones, calcium, phosphorus, and some associated disorders.
Overview of Calcium and Bone Metabolism
Etiology and Pathophysiology
Hypocalcemia, a low serum calcium level, stimulates parathyroid hormone (PTH) secretion, and hypercalcemia, a high serum calcium level, inhibits it (a negative feedback system). Because phosphate is closely related to calcium in body functions, PTH also regulates phosphate metabolism. In general, when serum calcium levels increase, serum phosphate levels decrease, and vice versa. Thus, an inverse relationship exists between calcium and phosphate.
When the serum calcium level falls below the normal range, PTH raises the level by acting on bone, intestines, and kidneys. In bone, breakdown is increased, so that calcium moves from bone into the serum. In the intestines, there is increased absorption of calcium ingested in food (PTH activates vitamin D, which increases intestinal absorption). In the kidneys, there is increased reabsorption of calcium in the renal tubules and less urinary excretion. The opposite effects occur with phosphate (PTH decreases serum phosphate and increases urinary phosphate excretion).
Calcium and phosphorus are discussed together because they are closely related physiologically. These mineral nutrients occur in many of the same foods, from which they are absorbed together. Calcium and phosphorous both play critical roles in cellular structure and function and, as calcium phosphate, in formation and maintenance of bones and teeth. Box 42.1 summarizes their characteristics and functions.
BOX 42.1 Characteristics and Functions of Calcium and Phosphorus
Calcium
Calcium is the most abundant cation in the body. Approximately 99% is located in the bones and teeth; the rest is in the extracellular fluid and soft tissues. Approximately half of serum calcium is bound, mostly to serum proteins, and is physiologically inactive. The other half is ionized and physiologically active. Ionized calcium can leave the vascular compartment and enter cells, where it participates in intracellular functions. An adequate amount of free (ionized) calcium is required for normal function of all body cells.
Of the calcium obtained from the diet, only 30% to 50% is absorbed from the small intestine; the rest is lost in feces. Absorption is increased in the presence of vitamin D, lactose, moderate amounts of fat, and high protein intake; increased acidity of gastric secretions; and a physiologic need. Absorption is inhibited by vitamin D deficiency; a high-fat diet; the presence of oxalic acid (from beet greens, chard), which combines with calcium to form insoluble calcium oxalate in the intestine; alkalinity of intestinal secretions, which leads to formation of insoluble calcium phosphate; diarrhea or other conditions of rapid intestinal motility, which do not allow sufficient time for absorption; and immobilization.
Calcium is lost from the body in feces, urine, and sweat. Even when there is deficient intake, approximately 150 mg are lost daily through the intestines (in mucosal and biliary secretions and sloughed intestinal cells). In lactating women, relatively large amounts are lost in breast milk.
Functions
 Calcium participates in many metabolic processes, including the regulation of
Calcium participates in many metabolic processes, including the regulation of
 Cell membrane permeability and function
Cell membrane permeability and function
 Nerve cell excitability and transmission of impulses (e.g., it is required for release of neurotransmitters at synapses)
Nerve cell excitability and transmission of impulses (e.g., it is required for release of neurotransmitters at synapses)
 Contraction of cardiac, skeletal, and smooth muscle
Contraction of cardiac, skeletal, and smooth muscle
 Conduction of electrical impulses in the heart
Conduction of electrical impulses in the heart
 Blood coagulation and platelet adhesion processes
Blood coagulation and platelet adhesion processes
 Hormone secretion
Hormone secretion
 Enzyme activity
Enzyme activity
 Catecholamine release from the adrenal medulla
Catecholamine release from the adrenal medulla
 Release of chemical mediators (e.g., histamine from mast cells)
Release of chemical mediators (e.g., histamine from mast cells)
 Calcium is required for building and maintaining bones and teeth. Bone calcium is composed mainly of calcium phosphate and calcium carbonate. In addition to these bound forms, a small amount of calcium is available for exchange with serum. This acts as a reserve supply of calcium. Calcium is constantly shifting between bone and serum as bone is formed and broken down. When serum calcium levels become low, calcium moves into serum.
Calcium is required for building and maintaining bones and teeth. Bone calcium is composed mainly of calcium phosphate and calcium carbonate. In addition to these bound forms, a small amount of calcium is available for exchange with serum. This acts as a reserve supply of calcium. Calcium is constantly shifting between bone and serum as bone is formed and broken down. When serum calcium levels become low, calcium moves into serum.
Requirements and Sources
The calcium requirement of normal adults is approximately 1000 mg daily. Increased daily amounts are needed by growing children (1200 mg), pregnant or lactating women (1200 mg), and postmenopausal women who do not take replacement estrogens (1500 mg to prevent osteoporosis).
The best sources of calcium are milk and milk products. Three 8-ounces glasses of milk daily contain approximately the amount needed by healthy adults. Calcium in milk is readily used by the body because milk also contains lactose and vitamin D, both of which are involved in calcium absorption. Other sources of calcium include vegetables (e.g., broccoli, spinach, kale, mustard greens) and seafood (e.g., clams, oysters).
Phosphorus
Phosphorus is one of the most important elements in normal body function. Most phosphorus is combined with calcium in bones and teeth as calcium phosphate (~ 80%). The remainder is distributed in every body cell and in extracellular fluid. It is combined with carbohydrates, lipids, proteins, and various other compounds.
Phosphorus is obtained from the diet, and approximately 70% of dietary phosphorus is absorbed from the gastrointestinal (GI) tract. The most efficient absorption occurs when calcium and phosphorus are ingested in approximately equal amounts. Because this equal ratio is present in milk, milk is probably the best source of phosphorus. In general, factors that increase or decrease calcium absorption act the same way on phosphorus absorption. Vitamin D enhances, but is not essential for, phosphorus absorption. Large amounts of calcium or aluminum in the GI tract may combine with phosphate to form insoluble compounds and thereby decrease absorption of phosphorus.
Phosphorus is lost from the body primarily in urine. In people with acute or chronic renal failure, phosphorus intake is restricted because excretion is impaired.
Functions
Phosphorus, most of which is located intracellularly as the phosphate ion, performs many metabolic functions:
 It is an essential component of deoxyribonucleic acid, ribonucleic acid, and other nucleic acids in body cells. Thus, it is required for cell reproduction and body growth.
It is an essential component of deoxyribonucleic acid, ribonucleic acid, and other nucleic acids in body cells. Thus, it is required for cell reproduction and body growth.
 It combines with fatty acids to form phospholipids, which are components of all cell membranes in the body. This reaction also prevents buildup of excessive amounts of free fatty acids.
It combines with fatty acids to form phospholipids, which are components of all cell membranes in the body. This reaction also prevents buildup of excessive amounts of free fatty acids.
 It forms a phosphate buffer system, which helps to maintain acid-base balance. When excess hydrogen ions are present in kidney tubules, phosphate combines with them and allows their excretion in urine. At the same time, bicarbonate is retained by the kidneys and contributes to alkalinity of body fluids. Although there are other buffering systems in the body, failure of the phosphate system leads to metabolic acidosis (retained hydrogen ions or acid and lost bicarbonate ions or base).
It forms a phosphate buffer system, which helps to maintain acid-base balance. When excess hydrogen ions are present in kidney tubules, phosphate combines with them and allows their excretion in urine. At the same time, bicarbonate is retained by the kidneys and contributes to alkalinity of body fluids. Although there are other buffering systems in the body, failure of the phosphate system leads to metabolic acidosis (retained hydrogen ions or acid and lost bicarbonate ions or base).
 It is necessary for cellular use of glucose and production of energy.
It is necessary for cellular use of glucose and production of energy.
 It is necessary for proper function of several B vitamins (i.e., the vitamins function as coenzymes in various chemical reactions only when combined with phosphate).
It is necessary for proper function of several B vitamins (i.e., the vitamins function as coenzymes in various chemical reactions only when combined with phosphate).
Requirements and Sources
Daily requirements for phosphorus are approximately 800 mg for normal adults and 1200 mg for growing children and pregnant or lactating women. Phosphorus is widely available in foods. Good sources are milk and other dairy products, meat, poultry, fish, eggs, and nuts. There is little risk of phosphorus deficiency with an adequate intake of calcium and protein.
Disorders of parathyroid function are related to hypoparathyroidism (insufficient production of PTH) or hyperparathyroidism (excessive production of PTH). Most often, the cause of hypoparathyroidism is removal of or damage to the parathyroid glands during neck surgery. Most often, the cause of hyperparathyroidism is a tumor or hyperplasia of a parathyroid gland. It also may result from ectopic secretion of PTH by malignant tumors (carcinomas of the lung, pancreas, kidney, ovary, prostate gland, or bladder). Clinical manifestations and treatment of hypoparathyroidism are the same as those of hypocalcemia. Clinical manifestations and treatment of hyperparathyroidism are the same as those of hypercalcemia.
Calcitonin is a hormone from the thyroid gland whose secretion is controlled by the concentration of ionized calcium in the blood flowing through the thyroid gland. When the serum level of ionized calcium increases, secretion of calcitonin increases. The function of calcitonin is to lower serum calcium in the presence of hypercalcemia, which it does by decreasing movement of calcium from bone to serum and increasing urinary excretion of calcium. The action of calcitonin is rapid but of short duration. Thus, this hormone has little effect on long-term calcium metabolism.
Vitamin D (calciferol) is a fat-soluble vitamin that includes both ergocalciferol (obtained from foods) and cholecalciferol (formed by exposure of skin to sunlight). It functions as a hormone and plays an important role in calcium and bone metabolism. The main action of vitamin D is to raise serum calcium levels by increasing intestinal absorption of calcium and mobilizing calcium from bone. It also promotes bone formation by providing adequate serum concentrations of minerals. Vitamin D is not physiologically active in the body. It must be converted to an intermediate metabolite in the liver, then to an active metabolite (1, 25-dihydroxyvitamin D or calcitriol) in the kidneys. PTH and adequate hepatic and renal function are required to produce the active metabolite.
Deficiency of vitamin D causes inadequate absorption of calcium and phosphorus. This, in turn, leads to low levels of serum calcium and stimulation of PTH secretion. In children, this sequence of events produces inadequate mineralization of bone (rickets), a rare condition in the United States. In adults, vitamin D deficiency causes osteomalacia, a condition characterized by decreased bone density and strength.
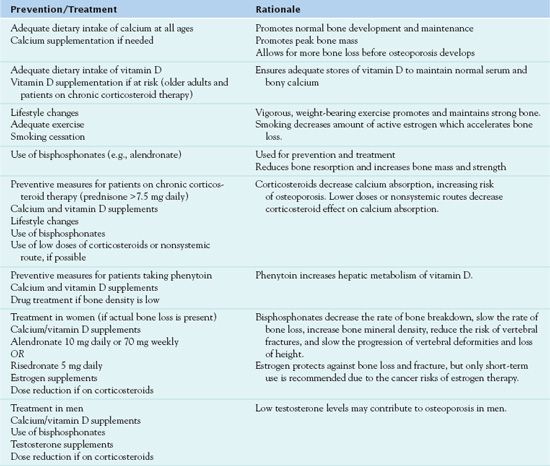
Bone is mineralized connective tissue that functions as structural support and a reservoir for calcium, phosphorus, magnesium, sodium, and carbonate. The role of bone in maintaining serum calcium levels takes precedence over its structural function (bone may be weakened or destroyed as calcium leaves bone and enters serum). Bone tissue is constantly being formed and broken down in a process called remodeling. Bone tissue removal is referred to as resorption. During childhood, adolescence, and early adulthood, formation usually exceeds breakdown (resorption) as the person attains adult height and peak bone mass. After approximately 35 years of age, resorption is greater than formation. Osteoporosis occurs when bone strength (bone density and bone quality) is impaired, leading to increased porousness and vulnerability to fracture. Hormonal deficiencies, some diseases, and some medications (e.g., glucocorticoids) can also increase resorption, resulting in loss of bone mass and osteoporosis. Table 42.1 presents an overview of the prevention and treatment of osteoporosis.
TABLE 42.1
Prevention and Treatment of Osteoporosis
Clinical Manifestations
The calcium disorders are hypocalcemia and hypercalcemia, either of which can be life-threatening. Hypocalcemic emergencies, for example, may result in tetany (neuromuscular irritability). The bone disorders discussed in this chapter are those characterized by increased resorption of calcium and loss of bone mass. These disorders weaken bone, and possibly leading to osteoporosis, with fractures, pain, and disability. Box 42.2 describes selected calcium and bone disorders.
BOX 42.2 Calcium and Bone Disorders
Hypocalcemia
Hypocalcemia is an abnormally low blood calcium level (i.e., less than 8.5 mg/dL). Causes may include inadequate intake of calcium and vitamin D, numerous disorders (e.g., diarrhea or malabsorption syndromes that cause inadequate absorption of calcium and vitamin D, hypoparathyroidism, renal failure, severe hypomagnesemia, hypermagnesemia, acute pancreatitis, rhabdomyolysis, tumor lysis syndrome, vitamin D deficiency), and several drugs (e.g., cisplatin, cytosine arabinoside, foscarnet, ketoconazole, pentamidine, agents used to treat hypercalcemia). Calcium deficits caused by inadequate dietary intake affect bone tissue rather than serum calcium levels. Two mechanisms result in hypocalcemia associated with renal failure. First, inability to excrete phosphate in urine leads to accumulation of phosphate in the blood (hyperphosphatemia). Because phosphate levels are inversely related to calcium levels, hyperphosphatemia induces hypocalcemia. Second, when kidney function is impaired, vitamin D conversion to its active metabolite is impaired. This results in decreased intestinal absorption of calcium.
Clinical manifestations are characterized by increased neuromuscular irritability, which may progress to tetany. Tetany is characterized by numbness and tingling of the lips, fingers, and toes; twitching of facial muscles; spasms of skeletal muscle; carpopedal spasm; laryngospasm; and convulsions. In young children, hypocalcemia may be manifested by convulsions rather than tetany and erroneously diagnosed as epilepsy. This may be a serious error because anticonvulsant drugs used for epilepsy may further decrease serum calcium levels. Severe hypocalcemia may cause lethargy or confusion.
Hypercalcemia
Hypercalcemia is an abnormally high blood calcium level (i.e., greater than 10.5 mg/dL). It may be caused by hyperparathyroidism, hyperthyroidism, malignant neoplasms, vitamin D or vitamin A intoxication, aluminum intoxication, prolonged immobilization, adrenocortical insufficiency, and ingestion of thiazide diuretics, estrogens, and lithium. Cancer is a common cause, especially carcinomas (of the breast, lung, head and neck, or kidney) and multiple myeloma. Cancer stimulates bone breakdown, which increases serum calcium levels. Increased urine output leads to fluid volume deficit. This leads, in turn, to increased reabsorption of calcium in renal tubules and decreased renal excretion of calcium. Decreased renal excretion potentiates hypercalcemia. Patients at risk for hypercalcemia should be monitored for early signs and symptoms, so treatment can be started before severe hypercalcemia develops.
Clinical manifestations are caused by the decreased ability of nerves to respond to stimuli and the decreased ability of muscles to contract and relax. Hypercalcemia has a depressant effect on nerve and muscle function. Gastrointestinal problems with hypercalcemia include anorexia, nausea, vomiting, constipation, and abdominal pain. Central nervous system problems include apathy, depression, poor memory, headache, and drowsiness. Severe hypercalcemia may produce lethargy, syncope, disorientation, hallucinations, coma, and death. Other signs and symptoms include weakness and decreased tone in skeletal and smooth muscle, dysphagia, polyuria, polyphagia, and cardiac dysrhythmias. In addition, calcium may be deposited in various tissues, such as the conjunctiva, cornea, and kidneys. Calcium deposits in the kidneys (renal calculi) may lead to irreversible damage and impairment of function.
Osteoporosis
Osteoporosis is characterized by decreased bone density (osteopenia) and weak, fragile bones that often lead to fractures, pain, and disability. Although any bones may be affected, common fracture sites are the vertebrae of the lower dorsal and lumbar spines, wrists, and hips. Risk factors include female sex, advanced age, small stature, lean body mass, white or Asian race, positive family history, low calcium intake, menopause, sedentary lifestyle, nulliparity, smoking, excessive ingestion of alcohol or caffeine, high protein intake, high phosphate intake, hyperthyroidism, and chronic use of certain medications (e.g., corticosteroids, phenytoin). Postmenopausal women who do not take estrogen replacement therapy are at high risk because of estrogen deficiency, age-related bone loss, and a low peak bone mass. Osteoporosis occurs in men but less often than in women. Both men and women who take high doses of corticosteroids are at high risk because the drugs demineralize bone. In addition, renal transplant recipients can acquire osteoporosis from corticosteroid therapy, decreased renal function, increased parathyroid hormone secretion, and cyclosporine immunosuppressant therapy.
Osteopenia or early osteoporosis may be present and undetected unless radiography or a bone density measurement is done. If detected, treatment is needed to slow bone loss. If undetected or untreated, clinical manifestations of osteoporosis include shortened stature (a measurable loss of height), back pain, spinal deformity, or a fracture. Fractures often occur with common bending or lifting movements or falling.
Paget’s Disease
Paget’s disease is an inflammatory skeletal disease that affects older people. Its etiology is unknown. It is characterized by a high rate of bone turnover and results in bone deformity and pain. It is treated with nonnarcotic analgesics and drugs that decrease bone resorption (e.g., bisphosphonates, calcitonin).



