Describe characteristics of selected upper respiratory disorders and symptoms.
 Identify the prototype drug for each drug class.
Identify the prototype drug for each drug class.
 Discuss nasal decongestants in terms of their action, use, contraindications, adverse effects, and nursing implications.
Discuss nasal decongestants in terms of their action, use, contraindications, adverse effects, and nursing implications.
 Describe antitussive agents in terms of their action, use, contraindications, adverse effects, and nursing implications.
Describe antitussive agents in terms of their action, use, contraindications, adverse effects, and nursing implications.
 Describe expectorants in terms of their action, use, contraindications, adverse effects, and nursing implications.
Describe expectorants in terms of their action, use, contraindications, adverse effects, and nursing implications.
 Discuss mucolytics in terms of their action, use, contraindications, adverse effects, and nursing implications.
Discuss mucolytics in terms of their action, use, contraindications, adverse effects, and nursing implications.
 Discuss the advantages and disadvantages of using combination products to treat the common cold.
Discuss the advantages and disadvantages of using combination products to treat the common cold.
 Understand how to use the nursing process in the care of patients receiving nasal decongestants, antitussives, expectorants, and mucolytic agents.
Understand how to use the nursing process in the care of patients receiving nasal decongestants, antitussives, expectorants, and mucolytic agents.
Clinical Application Case Study
Archie Hobbs is a 45-year-old welder at an industrial plant. The occupational nurse at the facility sees a high rate of colds. Mr. Hobbs comes to the health office complaining about his nasal congestion and cough.
KEY TERMS
Antitussive: agent used to suppress cough by depressing the cough center in the medulla oblongata or the cough receptors in the throat, trachea, or lungs
Expectorant: agent that liquefies respiratory secretions and allows for their easier removal; administered orally
Mucolytic: agent that liquefies mucus in the respiratory tract; administered by inhalation
Nasal decongestant: agent used to relieve nasal obstruction and discharge
Rhinitis: inflammation of nasal mucosa
Rhinosinusitis: inflammation of the nasal and paranasal sinus mucosa
Sinusitis: inflammation of the paranasal sinuses (air cells that connect with the nasal cavity and are lined by similar mucosa)
Introduction
This chapter introduces the pharmacological care of the patient who is receiving drugs used to treat upper respiratory disorders, such as the common cold and sinusitis, with symptoms such as nasal congestion, cough, and excessive secretions. A more extensive discussion of some of these many drugs used to treat these conditions exists in other chapters; their discussion here relates to their use in upper respiratory conditions.
Overview of Nasal Congestion and Other Respiratory Symptoms
Etiology and Pathophysiology
The Common Cold
The common cold, a viral infection of the upper respiratory tract, is the most common respiratory tract infection. Adults usually have two to four colds per year; schoolchildren may have as many as 10 colds annually. Many types of viruses, most often the rhinovirus, cause colds. Shedding of these viruses by infected people, mainly from nasal mucosa, can result in rapid spread to other people.
The viruses can enter the body through mucous membranes. Cold viruses can survive for several hours on the skin and on hard surfaces, such as wood and plastic. There may also be airborne spread from sneezing and coughing, but this source is considered secondary. After the viruses gain entry, the incubation period is generally 5 days, the most contagious period is about 3 days after symptoms begin, and the cold usually lasts near 7 days. Because of the way cold viruses spread, frequent and thorough hand hygiene (by both infected and uninfected people) is the most important protective and preventive measure. The tendency for overmedication and inappropriate use of antibiotics for the common cold is widespread and poses significant risk of complications and drug resistance.
Rhinosinusitis
Some of the most common conditions that affect the upper respiratory system are inflammatory responses. Sinusitis is inflammation of the mucous membranes lining the paranasal sinuses. Rhinitis is inflammation and congestion of nasal mucosa. Because sinusitis is almost always accompanied by inflammation of the contiguous nasal mucosa, the term rhinosinusitis is preferred. Sinusitis often results from a viral infection; allergic rhinitis occurs as a response to an allergen. Seasonal rhinitis, or hay fever, occurs in a specific season.
Ciliated mucous membranes help move fluid and microorganisms out of the sinuses and into the nasal cavity. (These membranes perform the same tasks in other parts of the respiratory tract.) This movement becomes impaired when sinus openings are blocked by nasal swelling, and the impairment is considered a major cause of sinus infections. Another contributing factor is decreased oxygen content in the sinuses, which aids the growth of microorganisms and impairs local defense mechanisms. In acute rhinosinusitis, the classic symptom triad is purulent nasal drainage, nasal obstruction, and facial pressure and/or pain.
Clinical Manifestations
Nasal Congestion
Nasal congestion occurs when the nasal passages become blocked as membranes lining the nose become swollen due to inflamed blood vessels. The blood vessels in the nasal mucosa become dilated, and the mucous membranes become engorged with blood. Stimulation of the nasal membranes occurs at the same time, resulting in increased mucus secretion.
Cough
Cough (a forceful expulsion of air from the lungs) is a protective reflex response to mechanical, chemical, or inflammatory irritation of the lungs mediated through neurons in the brainstem or cough center. The cough reflex involves central and peripheral mechanisms. Centrally, the cough center in the medulla oblongata receives stimuli and initiates the reflex response (deep inspiration, closed glottis, buildup of pressure within the lungs, and forceful exhalation). Peripherally, air, dryness of mucous membranes, or excessive secretions may stimulate cough receptors in the pharynx, larynx, trachea, or lungs. A cough helps remove foreign bodies, environmental irritants, or accumulated secretions from the respiratory tract. A cough is productive when secretions are expectorated; it is nonproductive when it is dry and no sputum is expectorated.
Cough is a prominent symptom of respiratory tract infections (e.g., the common cold, influenza, bronchitis, pharyngitis) as well as chronic obstructive pulmonary diseases (e.g., emphysema, chronic bronchitis). When cough is associated with the common cold, it usually stems from postnasal drainage and throat irritation.
Bronchial Secretions
Bronchial secretions can result from numerous conditions, such as the common cold, where phlegm is produced in the chest. In addition, bronchial secretions can be a symptom of pneumonia, upper respiratory infections, acute and chronic bronchitis, emphysema, and asthma. Postnasal mucus may accumulate in the chest. Alternatively, secretions may be due to nonrespiratory conditions, such as immobility, debilitation, cigarette smoking, or surgery. Surgical procedures involving the chest or abdomen are most likely to be associated with retention of secretions because pain may decrease the patient’s ability to cough, breathe deeply, and ambulate.
Excessive secretions may seriously impair respiration by obstructing airways and preventing air flow to and from alveoli, where gas exchange occurs. Secretions also may cause atelectasis (a condition in which part of the lung is airless and collapses) by blocking airflow, and they may cause or aggravate infections by supporting bacterial growth.
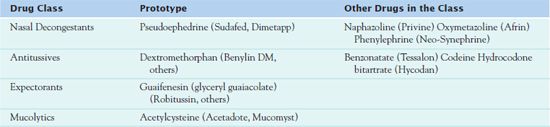
Drug Therapy
Numerous drugs are available to treat the symptoms of respiratory disorders. Many are nonprescription drugs that can be obtained alone or in combination products on an over-the-counter (OTC) basis. Available drugs include nasal decongestants, antitussives, expectorants, and mucolytics (Table 29.1).
Nasal Decongestants
Indications for nasal decongestants are the relief of nasal obstruction and discharge. Adrenergic (sympathomimetic) drugs are most often used for this purpose (see Chap. 27). These agents relieve nasal congestion and swelling by constricting arterioles and reducing blood flow to nasal mucosa. Oral and topical decongestants are available.  Pseudoephedrine (Sudafed) is the prototype.
Pseudoephedrine (Sudafed) is the prototype.
Pharmacokinetics
The onset of action of oral pseudoephedrine is approximately 30 minutes and typically peaks in 1 to 2 hours. The drug has a half-life of 4 to 8 hours. Metabolism to an active metabolite occurs in the liver. Excretion is via the kidneys, and the extent of excretion, is dependent on urine pH and flow rate.
Action
Pseudoephedrine acts directly on adrenergic receptors and acts indirectly by releasing norepinephrine from its storage sites. The drug produces vasoconstriction, which shrinks nasal mucosa membranes, resulting in decreased nasal congestion. It may potentiate the drainage of sinus secretions. In addition, pseudoephedrine may increase irritability of the heart muscle, especially at high doses.
Use
Uses of pseudoephedrine include the temporary relief of symptoms associated with nasal congestion due to the common cold, allergies, and sinuses. Health care providers may also use it to reduce local blood flow before nasal surgery and to aid in visualization of the nasal mucosa during diagnostic examinations.
Table 29.2 presents dosage information about various decongestants. It is not necessary to adjust dosages for pseudoephedrine in patients with hepatic impairment. Specific guidelines for adjustment in dosage in the presence of hepatic impairment are not available.
 TABLE 29.2
TABLE 29.2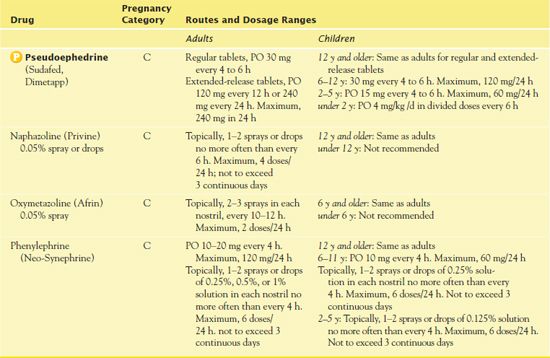
Use in Children
Experts consider pseudoephedrine effective in children older than 4 years of age, but research studies about the drug’s effectiveness in younger children are inconclusive. One issue is that the low doses found in children’s preparations may be insufficient to produce therapeutic effects. As a result, some pediatricians do not recommend use of the drug, whereas others say that it may be useful in some children.
Certain organizations have expressed caution about the use of pseudoephedrine in young children.
• In 2007, the Centers for Disease Control and Prevention (CDC) warned of the risk of serious injury or fatal overdose from the administration of cough and cold products to children and infants younger than 2 years of age.
• In 2007, the U.S. Food and Drug Administration (FDA) recommended that nonprescription cough and cold products containing pseudoephedrine, dextromethorphan, chlorpheniramine, diphenhydramine, brompheniramine, phenylephrine, clemastine, or guaifenesin not be used in children younger than 6 years of age.
• In 2008, the FDA issued a Public Health Advisory recommending that OTC cough and cold products not be used in infants and children younger than 2 years of age.
Use in Older Adults
The increased risk of adverse effects from oral nasal decongestants (e.g., hypertension, cardiac dysrhythmias, nervousness, insomnia) is a major concern in older adults. Adverse effects from topical agents are less likely, but rebound nasal congestion and systemic effects may occur with overuse. Older patients with significant cardiovascular disease should avoid pseudoephedrine.
Use in Patients With Renal Impairment
Because pseudoephedrine is excreted primarily via the kidneys, caution in patients with renal impairment is important. It may be necessary to reduce the dosage to avoid potential drug accumulation and drug toxicity.
Use in Patients With Critical Illness
It is appropriate to use pseudoephedrine in patients with critical illness for relief of symptoms. However, caution is warranted with concomitant medications and comorbid disease, such as cardiovascular disorders, glaucoma, and diabetes. In addition, pseudoephedrine may produce central nervous system (CNS) stimulation, so caution is also necessary in patients with seizure disorders.
Use in Patients Receiving Home Care
People often take pseudoephedrine in the home care setting. Household members may ask the home care nurse for advice about OTC remedies they are taking for conditions such as allergies, colds, coughs, and sinus headaches. Before recommending a particular product, the nurse needs to assess the intended recipient for conditions or other medications that contraindicate the product’s use. For example, the nasal decongestant component may cause or aggravate a cardiovascular disorder (e.g., hypertension). The home care nurse also needs to evaluate other medications the patient is taking in terms of potential drug interactions with the cold remedy. In addition, the nurse must emphasize the need to read the label of any OTC medication for ingredients, precautions, contraindications, drug interactions, and administration instructions.
QSEN Safety Alert 
To ensure accurate dosing in children, it is necessary to use measuring devices specifically designed for the administration of medications.
Adverse Effects
Some notable significant adverse reactions of pseudoephedrine include hypotension, dysrhythmia, impaired coordination, dizziness, excitability, headache, insomnia, restlessness, seizures, vertigo, dysuria, urinary retention, urinary difficulty, and thrombocytopenia. Some people may also experience blurred vision, tinnitus, chest tightness, dry nose, nasal congestion, and wheezing.
Contraindications
Contraindications to pseudoephedrine use include severe hypertension or coronary artery disease because of the drug’s cardiac stimulating and vasoconstricting effects. Another contraindication is narrow-angle glaucoma. Caution is necessary with cardiac dysrhythmias, hyperthyroidism, diabetes mellitus, glaucoma, and prostatic hypertrophy. Patients who take tricyclic or monoamine oxidase (MAO) inhibitor antidepressants should not receive pseudoephedrine.
Nursing Implications
Preventing Interactions
Many medications interact with pseudoephedrine, increasing its effect (Box 29.1). Caffeine can enhance the adverse effects of pseudoephedrine. The herb coleus may increase the effectiveness of the drug. Tannin-containing herbs such as green or black tea or witch hazel may decrease the absorption and effectiveness of the drug.
BOX 29.1  Drug Interactions: Pseudoephedrine
Drug Interactions: Pseudoephedrine
Drugs That Increase the Effects of Pseudoephedrine
 Cocaine, digoxin, general anesthetics, monoamine oxidase (MAO) inhibitors, other adrenergic drugs, thyroid preparations, xanthines
Cocaine, digoxin, general anesthetics, monoamine oxidase (MAO) inhibitors, other adrenergic drugs, thyroid preparations, xanthines
Increase the risk of cardiac dysrhythmias
 Antihistamines, epinephrine, ergot alkaloids, MAO inhibitors, methylphenidate
Antihistamines, epinephrine, ergot alkaloids, MAO inhibitors, methylphenidate
Increase the risk of hypertension due to vasoconstriction
Use of Over-the-Counter (OTC) Cough and Cold Medications in Children Younger Than 2 Years
by IRWIN, K.A.
Journal of Pediatric Health Care
2007, 21(4), 272–275
Reviews of the use of OTC cough and cold medicines in children younger than 2 years of age have demonstrated that the use of decongestants, antitussives, antihistamines, and expectorants as OTC cold medications in these young children should be avoided. Additionally, complementary and alternative therapies such as echinacea, vitamin C, and zinc have no beneficial effect in treating the cold symptoms in children and are not recommended for use. Investigations have demonstrated that not only are OTC cough and cold medicines no more effective than a placebo in reducing symptoms, but they may be harmful. In 2005, the Centers for Disease Control and Prevention (CDC) reviewed the deaths of three children younger than 6 months of age. The CDC discovered that the underlying cause of death was excessive levels of OTC cough and cold medicines. The main medicine prominently linked with death was pseudoephedrine.
IMPLICATIONS FOR NURSING PRACTICE: Health care providers often recommend that parents try one or more decongestants, antitussives, antihistamines, and expectorants available as OTC cold medications in treating cold symptoms in children. However, medications useful in adults may not be effective in children; the best available evidence should govern appropriate decisions regarding use of any medication in any age group.
Administering the Medication
Patients may take the oral form of pseudoephedrine with or without food. It is important not to crush extended-release preparations.
Assessing for Therapeutic Effects
The nurse assesses for decreased nasal inflammation and congestion after administration of pseudoephedrine. Laboratory monitoring is not necessary.
Assessing for Adverse Effects
The nurse must monitor for cardiac symptoms, particularly in patients with a cardiac history. If anaphylaxis, chest tightness, or throat swelling occurs, it is necessary to discontinue pseudoephedrine immediately.
Patient Teaching
Box 29.2 outlines patient teaching guidelines for nasal decongestants such as pseudoephedrine.
BOX 29.2  Patient Teaching Guidelines for Nasal Decongestants, Antitussive Medications, Expectorants, and Mucolytics
Patient Teaching Guidelines for Nasal Decongestants, Antitussive Medications, Expectorants, and Mucolytics
General Considerations
 These drugs may relieve symptoms but do not cure the disorder causing the symptoms.
These drugs may relieve symptoms but do not cure the disorder causing the symptoms.
 An adequate fluid intake, humidification of the environment, and sucking on hard candy or throat lozenges can help relieve mouth dryness and cough.
An adequate fluid intake, humidification of the environment, and sucking on hard candy or throat lozenges can help relieve mouth dryness and cough.
 Over-the-counter (OTC) cold remedies should not be used longer than 1 week. Do not use nose drops or sprays more often or longer than recommended. Excessive or prolonged use may damage nasal mucosa and produce chronic nasal congestion.
Over-the-counter (OTC) cold remedies should not be used longer than 1 week. Do not use nose drops or sprays more often or longer than recommended. Excessive or prolonged use may damage nasal mucosa and produce chronic nasal congestion.
 Do not increase dosage if symptoms are not relieved by recommended amounts.
Do not increase dosage if symptoms are not relieved by recommended amounts.
 See a health care provider if symptoms persist longer than 1 week.
See a health care provider if symptoms persist longer than 1 week.
 Inform health care providers about any herbal supplements that are being taken.
Inform health care providers about any herbal supplements that are being taken.
 Read the labels of OTC allergy, cold, and sinus remedies for information about ingredients; many products contain more than the active ingredient. Understand dosages, conditions, or other medications with which the drugs should not be taken and adverse effects.
Read the labels of OTC allergy, cold, and sinus remedies for information about ingredients; many products contain more than the active ingredient. Understand dosages, conditions, or other medications with which the drugs should not be taken and adverse effects.
 Do not combine two drug preparations containing the same or similar active ingredients. For example, pseudoephedrine is the nasal decongestant component of most prescription and OTC sinus and multi-ingredient cold remedies. The recommended dose for immediate-release preparations is usually 30 to 60 mg of pseudoephedrine; doses in extended-release preparations are usually 120 mg. Taking more than one preparation containing pseudoephedrine (or phenylephrine, a similar drug) may increase dosage to toxic levels and cause irregular heartbeats and extreme nervousness.
Do not combine two drug preparations containing the same or similar active ingredients. For example, pseudoephedrine is the nasal decongestant component of most prescription and OTC sinus and multi-ingredient cold remedies. The recommended dose for immediate-release preparations is usually 30 to 60 mg of pseudoephedrine; doses in extended-release preparations are usually 120 mg. Taking more than one preparation containing pseudoephedrine (or phenylephrine, a similar drug) may increase dosage to toxic levels and cause irregular heartbeats and extreme nervousness.
 Note that many combination products contain acetaminophen or ibuprofen as pain relievers. If you are taking another form of one of these drugs (e.g., Tylenol or Advil), there is a risk of overdosage and adverse effects. Acetaminophen can cause liver damage; ibuprofen is a relative of aspirin that can cause gastrointestinal upset and bleeding. Thus, you need to be sure your total daily dosage is not excessive (with Tylenol, above four doses of 1000 mg each; with ibuprofen, above 2400 mg).
Note that many combination products contain acetaminophen or ibuprofen as pain relievers. If you are taking another form of one of these drugs (e.g., Tylenol or Advil), there is a risk of overdosage and adverse effects. Acetaminophen can cause liver damage; ibuprofen is a relative of aspirin that can cause gastrointestinal upset and bleeding. Thus, you need to be sure your total daily dosage is not excessive (with Tylenol, above four doses of 1000 mg each; with ibuprofen, above 2400 mg).
 People with diabetes mellitus should read OTC labels for sugar content because many decongestants and cough medicines may contain sucrose, glucose, or corn syrup as a base.
People with diabetes mellitus should read OTC labels for sugar content because many decongestants and cough medicines may contain sucrose, glucose, or corn syrup as a base.
Self-Administration
 Take medications as prescribed or as directed on the labels of OTC preparations. Taking excessive amounts or taking recommended amounts too often can lead to serious adverse effects.
Take medications as prescribed or as directed on the labels of OTC preparations. Taking excessive amounts or taking recommended amounts too often can lead to serious adverse effects.
 Do not chew or crush long-acting tablets or capsules (e.g., those taken once or twice daily). Such actions can cause rapid drug absorption, high blood levels, and serious adverse effects, rather than the slow absorption and prolonged action intended with these products.
Do not chew or crush long-acting tablets or capsules (e.g., those taken once or twice daily). Such actions can cause rapid drug absorption, high blood levels, and serious adverse effects, rather than the slow absorption and prolonged action intended with these products.
 For OTC drugs available in different dosage strengths, start with lower recommended doses rather than “maximum strength” formulations or the highest recommended doses. It is safer to see how the drugs affect you, then increase doses if necessary.
For OTC drugs available in different dosage strengths, start with lower recommended doses rather than “maximum strength” formulations or the highest recommended doses. It is safer to see how the drugs affect you, then increase doses if necessary.
 With topical nasal decongestants:
With topical nasal decongestants:
 Use only preparations labeled for intranasal use. For example, phenylephrine (Neo-Synephrine) is available in both nasal and eye formulations. The two types of solutions cannot be used interchangeably. In addition, phenylephrine preparations may contain 0.125%, 0.25%, 0.5%, or 1% of drug. Be sure the concentration is appropriate for the person to receive it (e.g., an infant, young child, older adult).
Use only preparations labeled for intranasal use. For example, phenylephrine (Neo-Synephrine) is available in both nasal and eye formulations. The two types of solutions cannot be used interchangeably. In addition, phenylephrine preparations may contain 0.125%, 0.25%, 0.5%, or 1% of drug. Be sure the concentration is appropriate for the person to receive it (e.g., an infant, young child, older adult).
 Blow the nose gently before instilling nasal solutions or sprays. This clears nasal passages and increases effectiveness of medications.
Blow the nose gently before instilling nasal solutions or sprays. This clears nasal passages and increases effectiveness of medications.
 To instill nose drops, lie down or sit with the neck hyperextended and instill medication without touching the dropper to the nostrils (to avoid contamination of the dropper and medication). Rinse the medication dropper after each use.
To instill nose drops, lie down or sit with the neck hyperextended and instill medication without touching the dropper to the nostrils (to avoid contamination of the dropper and medication). Rinse the medication dropper after each use.
 For nasal sprays, sit or stand, squeeze the container once to instill medication, and rinse the spray tip after each use. Most nasal sprays are designed to deliver one dose when used correctly.
For nasal sprays, sit or stand, squeeze the container once to instill medication, and rinse the spray tip after each use. Most nasal sprays are designed to deliver one dose when used correctly.
 Report palpitations, dizziness, drowsiness, or rapid pulse. These effects may occur with nasal decongestants and cold remedies and may indicate excessive dosage.
Report palpitations, dizziness, drowsiness, or rapid pulse. These effects may occur with nasal decongestants and cold remedies and may indicate excessive dosage.
 Take dextromethorphan as directed; increased intake can lead to increased CNS impairment. Take cough syrups undiluted and avoid eating and drinking for approximately 30 minutes.
Take dextromethorphan as directed; increased intake can lead to increased CNS impairment. Take cough syrups undiluted and avoid eating and drinking for approximately 30 minutes.
 Part of the beneficial effect of cough syrups stems from soothing effects on pharyngeal mucosa. Food or fluid removes the medication from the throat.
Part of the beneficial effect of cough syrups stems from soothing effects on pharyngeal mucosa. Food or fluid removes the medication from the throat.
 If the cough has not improved after 7 days or if symptoms include high fever, skin rash, or persistent headache with cough, seek help from a health care provider.
If the cough has not improved after 7 days or if symptoms include high fever, skin rash, or persistent headache with cough, seek help from a health care provider.
 If you are taking acetylcysteine, understand that increasing fluid intake as directed helps loosen and mobilize secretions. In addition:
If you are taking acetylcysteine, understand that increasing fluid intake as directed helps loosen and mobilize secretions. In addition:
 The nebulization may initially cause an unpleasant odor, which soon resolves.
The nebulization may initially cause an unpleasant odor, which soon resolves.
 If the mask leaves a sticky residue on the face, remove it with water.
If the mask leaves a sticky residue on the face, remove it with water.
 Clean the nebulizer equipment after use to minimize infections and prevent buildup of the drug on the equipment.
Clean the nebulizer equipment after use to minimize infections and prevent buildup of the drug on the equipment.



