Understand the pathophysiology of migraine headaches.
 Identify the major manifestations of tension headaches, cluster headaches, migraine headaches, and menstrual migraine headaches.
Identify the major manifestations of tension headaches, cluster headaches, migraine headaches, and menstrual migraine headaches.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for nonsteroidal anti-inflammatory drugs administered as abortive therapy for migraines.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for nonsteroidal anti-inflammatory drugs administered as abortive therapy for migraines.
 Describe the action, use, adverse effects, contraindications, and nursing implications for acetaminophen–aspirin–caffeine combinations administered as abortive therapy for headaches.
Describe the action, use, adverse effects, contraindications, and nursing implications for acetaminophen–aspirin–caffeine combinations administered as abortive therapy for headaches.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for ergot alkaloids administered as abortive therapy.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for ergot alkaloids administered as abortive therapy.
 Identify the prototypes and describe the action, adverse effects, contraindications, and nursing implications for triptans administered as abortive therapy.
Identify the prototypes and describe the action, adverse effects, contraindications, and nursing implications for triptans administered as abortive therapy.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for estrogen administered for menstrual migraines.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for estrogen administered for menstrual migraines.
 Identify the medications used for the prevention of migraine headaches.
Identify the medications used for the prevention of migraine headaches.
 Describe the action, use, adverse effects, contraindications, and nursing implications for antiemetic drugs used in the treatment of migraine headache.
Describe the action, use, adverse effects, contraindications, and nursing implications for antiemetic drugs used in the treatment of migraine headache.
 Implement the nursing process of care of patients of all ages who suffer from migraine headaches.
Implement the nursing process of care of patients of all ages who suffer from migraine headaches.
Clinical Application Case Study
Tanya Van Art, an 18-year-old young woman, has experienced headaches since she was 13 years old. She has been experiencing headaches with increased severity in the past year. While at work this past week, she developed a severe headache with nausea and vomiting. She was admitted to the emergency department. On admission, her blood pressure was 180/90 mm Hg and her pain was 10 on a 10-point scale. In the emergency department, she received ketorolac tromethamine 30 mg intravenous (IV). The diagnosis was acute migraine headache.
KEY TERMS
Abortive therapy: medications administered in the treatment of symptoms of migraine headache
Aura: subjective sensation that immediately precedes a migraine headache, consisting of a breeze, odor, or light
Cluster headache: recurrent, severe, unilateral orbitotemporal headache related to a histamine reaction
Menstrual migraine headache: migraine headache associated with a drop in circulating estrogen that occurs 2 to 3 days prior to the onset of menses
Migraine headache: unilateral pain in the head that may or may not be accompanied by an aura; may be associated with vertigo, nausea, vomiting, and photophobia
Preventive therapy: administration of medications to prevent the onset of migraine headaches
Tension headache: headache associated with nervous tension or anxiety, often related to chronic contraction of scalp muscles
Vascular constriction: narrowing of the blood vessels
Introduction
This chapter discusses the various types of headaches, all of which produce pain. However, the pain experienced by patients is different with each type of headache. This chapter also considers the pharmacological treatment of each of these headaches.
Different types of headaches have different symptoms. Cluster headaches are recurrent, severe, unilateral orbitotemporal headaches that are associated with histamine reactions. Tension headaches are the result of chronic contraction of the scalp muscles and are associated with nervous tension or anxiety. Migraine headaches are unilateral pain in the head that may or may not be accompanied by an aura. An aura is a subjective sensation that immediately precedes the migraine headache consisting a breeze, odor, or light. Menstrual migraine headaches are associated with a drop in circulating estrogen 2 to 3 days prior to the onset of menses.
Overview of Migraine Headaches
Migraine headaches are common disorders. Annually, they affect approximately 20% of women and 8% of men. Migraines demonstrate a familial pattern, and authorities believe that they are inherited as autosomal dominant traits with incomplete penetrance. Migraine headaches with an aura are more common with the genetic inheritance. During childhood, migraine headaches are evenly distributed between boys and girls; however, in adulthood, migraines affect women three times more often than men. Food that precipitate migraine effects include aged cheeses, fermented foods, aspartame, monosodium glutamate, and chocolate (Solomon & Jamieson, 2009).
Pathophysiology
Cluster Headaches
The pathophysiology of cluster headaches is not completely understood. One theory, the major one, states that primary cluster headaches are characterized by hypothalamic activation with secondary activations of the trigeminal autonomic reflex. Another theory states that neurogenic inflammation of the walls of the cavernous sinus obliterates venous outflow, injuring the transverse sympathetic fibers of the intracranial internal carotid artery and its branches (May, 2010).
Tension Headaches
The pathophysiology of tension headaches is multifactorial. A wide variation exists in the experiences of people who suffer from tension headaches, but the current theory of chronic tension headache asserts that a person experiences a sensitization of the dorsal horn neurons related to increased nociceptive inputs from pericranial myofascial tissues. Experts believe that this heightened sensitivity of pain pathways in the central nervous system (CNS) plays a critical role in the pathogenesis. With a decreased pain threshold, the person misinterprets incoming signals as pain. Decreased pain, thermal, and electrical thresholds reported in patients with chronic tension headaches probably represent a central misinterpretation of incoming signals (Taylor, 2008).
Migraine Headaches
Authorities have proposed two theories related to the pathophysiology of migraine headaches. First, at the onset of a migraine, the trigeminal nerve is stimulated, resulting in the release of neuropeptides. This leads to painful neurogenic inflammation in the meningeal vasculature characterized by plasma protein extravasation, vasodilation, and mast cell degranulation. Second, neurogenic vasodilation of the meningeal blood vessels occurs, producing inflammation. The activations of trigeminal sensory fibers cause neurogenic dural vasodilation mediated by the calcitonin gene-related peptide. The calcitonin gene-related peptide is elevated during a migraine (Porth & Matfin, 2009).
Clinical Manifestations
Cluster Headaches
Cluster headaches usually occur up to eight times per day, with severe orbital, supraorbital, or temporal pain accompanied by autonomic symptoms such as ptosis, miosis, lacrimation, conjunctival injection, rhinorrhea, and nasal congestion (May, 2010).
Tension Headaches
Characteristic signs and symptoms of tension headaches include bilateral, nonthrobbing head pain of mild to moderate intensity. Patients may describe pressure, head fullness, or a band-like sensation around the head, or they may report a feeling like a heavy weight is on their head or shoulders (Taylor, 2008).
Migraine Headaches
Migraine headaches with an aura have four phases: prodrome, aura, headache, and recovery. The prodrome phase occurs hours or days before the onset of a migraine headache. Symptoms include depression, irritability, feeling cold, cravings, loss of appetite, alterations in activity, polyuria, diarrhea, and constipation. The aura phase, which occurs only in some patients, involves an aura lasting 1 hour with focal neurologic symptoms, visual disturbances, or vision in only half of the visual field. The headache phase is characterized by vasodilation and a decline in serotonin levels. A throbbing headache becomes more intense, lasting for several hours. The headache can become incapacitating, with photophobia, nausea, and vomiting. The recovery phase involves slow subsiding of the pain. There may be muscle contractions in the neck and scalp, with localized tenderness, tiredness, and alterations in mood. The patient may sleep for hours after the recovery phase (Smeltzer, Bare, Hinkle, & Cheever, 2010).
Chronic migraine headaches may be a problem. The chronic migraine is diagnosed by the presence of a migraine headache without an aura for 8 days or more per month for 3 months. The headache is unilateral, pulsating, with moderate to severe intensity, and aggravated by activity (Garza & Schwedt, 2011).
Drug Therapy
Cluster Headaches
Treatment of cluster headaches involves subcutaneous sumatriptan and oxygen. It is important to note that although oxygen may be effective in some patients, repeated or frequent use in a short period of time should be avoided. Evidence has shown that the frequency of cluster headaches may increase in some patients with overuse of oxygen. Ergot derivatives, lidocaine, and octreotide are also effective in the treatment of acute cluster headaches.
Tension Headaches
Acute therapy for tension headaches entails the use of non-pharmacological methods such as rest, relaxation techniques, or stress-reduction strategies as well as medication. Pharmacological treatment of tension headaches includes acetaminophen, aspirin, and nonsteroidal anti-inflammatory agents (see Chap. 14).
Migraine Headaches
There are two specific courses of treatment for migraine headaches: abortive and preventive therapy. Abortive therapy is the administration of medications to treat the symptoms of migraine headache. Preventive therapy is the administration of medications to prevent the development of a migraine headache. Medications used in the treatment of migraine headaches are listed in Table 51.1.
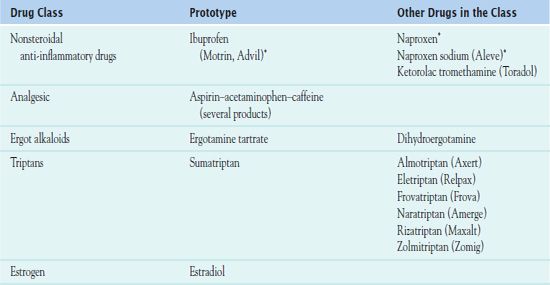
*See Chap. 14 for more information. Naproxen is commonly prescribed for the treatment of migraine headaches.
The abortive agents administered for the treatment of migraine headaches include nonsteroidal anti-inflammatory agents, aspirin-acetaminophen with caffeine medication, the ergot alkaloids, and the triptans. According to the American Academy of Neurology, the pharmacological and nonpharmacological treatment of long-term migraine is to reduce the frequency, severity, and disability. The initial pharmacotherapy for acute treatment of migraine is the administration of triptans (serotonin receptor [5-HT1B and 5-HT1D] agonists). Patients who experience nausea and vomiting may receive intranasal or subcutaneous sumatriptan.
Women who experience menstrual migraines take estrogen preparations. People who suffer from migraines take preventive medications, which are discussed later in this chapter.
Clinical Application 51-1
 What does the nurse teach Ms. Van Art about the pathophysiology of acute migraine?
What does the nurse teach Ms. Van Art about the pathophysiology of acute migraine?
NCLEX Success
1. A patient is admitted to the emergency department with a severe headache with nausea and vomiting. She receives a diagnosis of an acute migraine headache. Which of the following medications assists in decreasing the nausea and vomiting related to the acute migraine episode?
A. intravenous ketorolac
B. intranasal sumatriptan
C. inhaled albuterol
D. oral diclofenac
2. Which of the following medications are administered for preventive therapy in the treatment of migraine?
A. beta blockers
B. nonsteroidal anti-inflammatory agents
C. ergot alkaloids
D. analgesics
Nonsteroidal Anti-Inflammatory Agents
Ibuprofen is the prototype of the nonsteroidal anti-inflammatory agents (see Chap. 14). However, naproxen sodium is more commonly prescribed for the treatment of migraine headaches. Thus, © naproxen or naproxen sodium (Aleve) is the prototype described in detail in this chapter.
Pharmacokinetics
There are two types of naproxen: naproxen and naproxen sodium. Naproxen has an onset of action of 1 hour, a peak of action of 2 to 4 hours, and duration of action of 7 hours or less. Naproxen sodium has an onset of action of 1 hour, a peak of action of 1 to 2 hours, and the same duration of action as naproxen. Metabolism of both agents occurs in the liver, and they have a half-life of 12 to 15 hours. Excretion is in the urine. Naproxen and naproxen sodium cross the placental barrier and enter the breast milk.
Action
Naproxen is a nonselective inhibitor of cyclooxygenase resulting in the inhibition of prostaglandin synthesis of COX-1 and COX-2. Naproxen sodium improves the solubility of naproxen through faster absorption and rapid onset of action (Suthisisang, Poolsup, Suksomboon, Lertpipopmetha, & Tepwitukgid, 2010).
Use
Prescribers order naproxen sodium to reduce the pain resulting from an acute migraine headache. Table 51.2 presents dosage information for naproxen and related drugs.
 TABLE 51.2
TABLE 51.2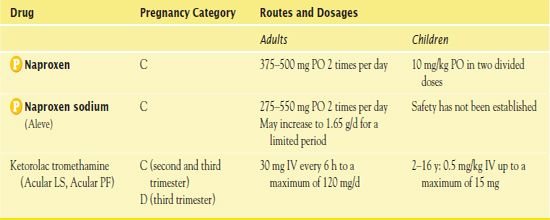
*Drugs used in headache treatment.
Use in Older Adults
Older people should not take more than 200 mg of naproxen sodium every 12 hours.
Use in Patients With Renal Impairment
Caution is necessary with the administration of naproxen sodium in patients with renal disease because the renal system excretes the drug.
Use in Patients With Hepatic Impairment
Caution is warranted with the administration of naproxen sodium in patients with hepatic impairment because the site of metabolism is the liver.
Adverse Effects
The most severe adverse effects of naproxen sodium include bronchospasm and anaphylaxis. Gastrointestinal (GI) adverse effects include GI bleeding, nausea, dyspepsia, and GI pain. U.S. Food and Drug Administration (FDA) has issued a BLACK BOX WARNING ♦ stating that naproxen sodium may put patients at increased risk for cardiovascular events and GI bleeding.
Contraindications
Contraindications to naproxen or naproxen sodium include a known allergy to aspirin or other nonsteroidal anti-inflammatory drugs as well as pregnancy and lactation. It is important to administer the medication cautiously to patients with asthma, cardiovascular dysfunction, hypertension, GI bleeding, and peptic ulcer.
Nursing Implications
Preventing Interactions
The administration of naproxen sodium with lithium results in increased lithium levels and the risk of lithium toxicity.
Assessing for Therapeutic Effects
Following the administration of naproxen or naproxen sodium, the patient should exhibit diminished pain. The nurse assesses the patient’s pain level using a pain scale.
Assessing for Adverse Effects
The nurse assesses the patient for GI upset, dyspepsia, or bleeding. He or she also assesses pulmonary function and lung sounds for bronchospasm or anaphylactic reaction.
Patient Teaching
Box 51.1 identifies patient teaching guidelines for naproxen sodium.
BOX 51.1  Patient Teaching Guidelines for Naproxen Sodium
Patient Teaching Guidelines for Naproxen Sodium
 Take the medication with meals to prevent gastrointestinal upset.
Take the medication with meals to prevent gastrointestinal upset.
 Take medication as prescribed.
Take medication as prescribed.
 Do not cut, crush, or chew tablets.
Do not cut, crush, or chew tablets.
 Do not operate machinery if dizziness or drowsiness occurs.
Do not operate machinery if dizziness or drowsiness occurs.
 Report sore throat, fever, rash, itching, edema, visual changes, and black, tarry stools to your health care provider.
Report sore throat, fever, rash, itching, edema, visual changes, and black, tarry stools to your health care provider.
Other Drugs in the Class
Migraine sufferers often seek treatment in the emergency department when the more commonly used abortive therapies are ineffective. In the emergency setting, ketorolac tromethamine is the most frequently administered intravenous medication for migraine sufferers who have not responded to oral abortive therapy.
Clinical Application 51-2
 What is the rationale for administering ketorolac to Ms. Van Art?
What is the rationale for administering ketorolac to Ms. Van Art?
Acetaminophen, Aspirin, and Caffeine
The combination of  acetaminophen, aspirin, and caffeine may be effective for the treatment of headaches. In the United States, brand names include Anacin Advanced Headache Formula, Excedrin Extra Strength, Excedrin Migraine, Goody’s Extra Strength, and Vanquish Extra Strength Pain Reliever.
acetaminophen, aspirin, and caffeine may be effective for the treatment of headaches. In the United States, brand names include Anacin Advanced Headache Formula, Excedrin Extra Strength, Excedrin Migraine, Goody’s Extra Strength, and Vanquish Extra Strength Pain Reliever.
Pharmacokinetics
To understand the pharmacokinetics of acetaminophen, aspirin, and caffeine, it is important to review each medication individually. Acetaminophen reaches a peak of action in 0.5 to 2 hours and possesses a 1-to 3-hour half-life. It crosses the placental barrier and enter the breast milk. The drug is metabolized in the liver and excreted in the urine. Aspirin has an onset of action of 5 to 30 minutes, reaches a peak of action in 15 to 120 minutes, and has a duration of action of 3 to 6 hours. The half-life of aspirin is 15 minutes to 12 hours. The drug is absorbed in the stomach and metabolized in the liver. Caffeine has an onset of action of 15 minutes and reaches a peak of action in 15 to 45 minutes. It readily crosses the placental barrier and enters breast milk. Like acetaminophen and aspirin, metabolism of caffeine takes place in the liver and elimination occurs in the kidneys.
Action
Acetaminophen may act as an analgesic, and its mechanism of action is unknown. Aspirin has the ability to inhibit the synthesis of prostaglandins, which are a mediator of inflammation. Caffeine increases calcium permeability in the sarcoplasmic reticulum to promote the accumulation of cyclic adenosine monophosphate (cAMP) and block the adenosine receptors, stimulating the CNS, cardiac activity, gastric acid secretion, and diuresis. It causes constriction of the blood vessels, which is known as vascular constriction. Migraine headaches result from the vasodilation of blood vessels. In addition, caffeine increases the effectiveness of acetaminophen and aspirin by approximately 40%.
Use
Acetaminophen-aspirin-caffeine products are administered to reduce pain related to migraine or tension headache. Table 51.3 presents oral dosage of information for these combination products.
 TABLE 51.3
TABLE 51.3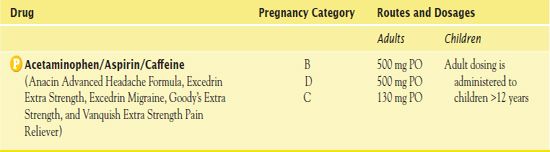
Use in Children
Children older than 12 years of age may receive the adult dose of the combination agent.
Use in Patients With Hepatic Impairment
People with hepatic impairment should not receive this combination agent on an ongoing basis. They may not metabolize acetaminophen in this combined medication effectively, leading to hepatotoxicity.
Adverse Effects
Each component of the combination medication has adverse effects, which will be addressed individually. Acetaminophen may result in headache, chest pain, dyspnea, myocardial damage with doses of 5 to 8 g/day, and hepatic impairment. Aspirin may lead to GI effects such as dyspepsia, heartburn, and epigastric discomfort as well as hematologic effects such as occult blood loss and hemostatic defects. Aspirin toxicity involves respiratory alkalosis, tachypnea, hemorrhage, excitement, confusion, seizures, tetany, cardiovascular collapse, and metabolic acidosis. Caffeine may result in excitement, insomnia, restlessness, tremors, headaches, and lightheadedness, as well as cardiovascular effects such as tachycardia, hypertension, extrasystole, and palpitations.
Contraindications
Contraindications to acetaminophen include a known allergy to the drug. Caution is necessary in impaired hepatic function, chronic alcoholism, pregnancy, and lactation. Contraindications to aspirin includes a known hypersensitivity to the drug or other anti-inflammatory agents. Vigilance is warranted with renal impairment. Contraindications to caffeine include duodenal ulcers, diabetes, and lactation. Caution is essential in pregnancy, renal and hepatic impairment, and cardiovascular disease.
Nursing Implications
People most commonly take the acetaminophen-aspirin-caffeine in the home setting. It is important to be familiar with all aspects of each medication to maintain medication safety.
Preventing Interactions
Several drug-drug interactions may occur with acetaminophen-aspirin-caffeine combinations. Box 51.2 names the specific medications that increase or decrease the effects of each of the medications in the combined drug. Other drug-drug interactions include the following:
BOX 51.2  Drug Interactions: Acetaminophen, Aspirin, and Caffeine
Drug Interactions: Acetaminophen, Aspirin, and Caffeine
Drugs That Increase the Effects of Acetaminophen
 Alcohol, barbiturates, carbamazepine, hydantoins, rifampin, sulfinpyrazone
Alcohol, barbiturates, carbamazepine, hydantoins, rifampin, sulfinpyrazone
Increase the risk of hepatotoxicity
Drugs That Increase the Effects of Aspirin
 Alcohol, anticoagulants, nonsteroidal anti-inflammatory agents
Alcohol, anticoagulants, nonsteroidal anti-inflammatory agents
Increase the bleeding risk
 Carbonic anhydrase inhibitors
Carbonic anhydrase inhibitors
Increase the risk of salicylate toxicity
Drugs That Increase the Effects of Caffeine
 Cimetidine, hormonal contraceptive, disulfiram, ciprofloxacin, mexiletine
Cimetidine, hormonal contraceptive, disulfiram, ciprofloxacin, mexiletine
Increase the central nervous system effects
Drugs That Decrease the Effects of Aspirin
 Acetazolamide, methazolamide, antacids, alkalinizers
Acetazolamide, methazolamide, antacids, alkalinizers
Decrease the salicylate levels
Drugs That Decrease the Effects of Caffeine
 Nicotine
Nicotine
Produces vasoconstriction
• Oral anticoagulants combined with acetaminophen increase hypothrombinemic effects.
• Aspirin combined with sulfonylureas and insulin results in greater glucose-lowering effects.
• Valproic acid combined with aspirin puts patients at risk for seizure activity secondary to protein receptor site displacement.
• Spironolactone or furosemide combined with aspirin leads to decreased diuretic effects.
• Theophylline or clozapine combined with caffeine increases the serum levels of theophylline or clozapine.
The concomitant administration of caffeine and guarana, ma huang, and ephedra with caffeine is not recommended.
Assessing for Therapeutic Effects
Following the administration of the acetaminophen–aspirin–caffeine combination, the patient should exhibit diminished pain. The nurse assesses for pain using a pain scale.
Assessing for Adverse Effects
The nurse assesses for hepatotoxicity, allergic reaction, fluid and electrolyte imbalance, hypoglycemia, agitation, and cardiovascular effects.
Patient Teaching
Box 51.3 identifies patient teaching guidelines for acetaminophen–aspirin–caffeine combinations.
BOX 51.3  Patient Teaching Guidelines for Acetaminophen-Aspirin- Caffeine Combinations
Patient Teaching Guidelines for Acetaminophen-Aspirin- Caffeine Combinations



