Recognize normal renal physiology and the conditions requiring diuretic administration.
 Describe the thiazide diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
Describe the thiazide diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
 Describe the loop diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
Describe the loop diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
 Describe the potassium-sparing diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
Describe the potassium-sparing diuretics in terms of their prototype, mechanism of action, indications for use, major adverse effects, and nursing implications.
 Discuss the rationale for using combination products containing a potassium-losing and a potassium-sparing diuretic.
Discuss the rationale for using combination products containing a potassium-losing and a potassium-sparing diuretic.
 Discuss the rationale for concomitant use of a loop diuretic and a thiazide or related diuretic.
Discuss the rationale for concomitant use of a loop diuretic and a thiazide or related diuretic.
 Understand how to apply the nursing process in the care of patients receiving diuretics.
Understand how to apply the nursing process in the care of patients receiving diuretics.
Clinical Application Case Study
Agnes Bass, a 68-year-old woman, presents to the emergency department in acute heart failure complaining of an inability to “catch my breath.” Her initial vital signs are temperature 99°F, pulse 108 beats per minute, respirations 28 per minute, and blood pressure 172/90 mm Hg. Her O2 saturation is 88% on room air. Mrs. Bass has a history of uncontrolled hypertension, and her husband reports that for the past 2 months, they did not have sufficient money to buy her medications.
KEY TERMS
Anasarca: generalized massive edema
Anuria: no urine output
Ascites: accumulation of fluid in the abdominal cavity
Ceiling threshold: near-maximum response of a drug that is yielded by a certain dose
Dependent edema: localized edema occurring in the feet and ankles in people who are ambulatory
Edema: excessive accumulation of fluid in body tissues
Introduction
Drugs used to treat fluid volume excess, thereby increasing urine formation and output, are referred to as diuretics. These drugs increase renal excretion of water, sodium, and other electrolytes. They are important therapeutic agents widely used in the management of both edematous (e.g., heart failure, renal and hepatic disease) and nonedematous (e.g., hypertension, ophthalmic surgery) conditions. Diuretics are also useful in preventing renal failure by their ability to sustain urine flow. To aid understanding of diuretic drug therapy, it is necessary to understand normal renal physiology.
Renal Physiology
The primary function of the kidneys is to regulate the volume, composition, and pH of body fluids. The kidneys receive approximately 25% of the cardiac output. From this large amount of blood flow, the normally functioning kidney is efficient in retaining substances needed by the body and eliminating those not needed.
The Nephron
The nephron is the functional unit of the kidney; each kidney contains approximately 1 million nephrons. Each nephron is composed of a glomerulus and a tubule (Fig. 32.1). The glomerulus is a network of capillaries that receives blood from the renal artery. Bowman’s capsule is a thin-walled structure that surrounds the glomerulus and then narrows and continues as the tubule. The tubule is a thin-walled structure of epithelial cells surrounded by peritubular capillaries. The tubule is divided into three main segments, the proximal tubule, loop of Henle, and distal tubule, which differ in structure and function. The tubules are often called convoluted tubules because of their many twists and turns. The convolutions provide a large surface area that brings the blood flowing through the peritubular capillaries and the glomerular filtrate flowing through the tubular lumen into close proximity. Consequently, substances can be readily exchanged through the walls of the tubules.
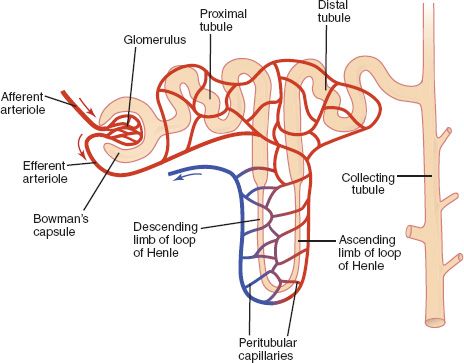
Figure 32.1 The nephron is the functional unit of the kidney
The nephron functions by three processes: glomerular filtration, tubular reabsorption, and tubular secretion. These processes normally maintain the fluid volume, electrolyte concentration, and pH of body fluids within a relatively narrow range. They also remove waste products of cellular metabolism. A minimum daily urine output of approximately 400 mL is required to remove normal amounts of metabolic end products.
Glomerular Filtration
Arterial blood enters the glomerulus by the afferent arteriole at the relatively high pressure of approximately 70 mm Hg. This pressure pushes water, electrolytes, and other solutes out of the capillaries into Bowman’s capsule and then to the proximal tubule. This fluid, called glomerular filtrate, contains the same components as blood except for blood cells, fats, and proteins that are too large to be filtered.
The glomerular filtration rate (GFR) is about 180 L/d, or 125 mL/min. Most of this fluid is reabsorbed as the glomerular filtrate travels through the tubules. The end product is about 2 L of urine daily. Because filtration is a nonselective process, the reabsorption and secretion processes determine the composition of the urine. After it is formed, urine flows into collecting tubules, which carry it to the renal pelvis, then through the ureters, bladder, and urethra for elimination from the body.
Blood that does not become part of the glomerular filtrate leaves the glomerulus through the efferent arteriole. The efferent arteriole branches into the peritubular capillaries that eventually empty into veins, which return the blood to systemic circulation.
Tubular Reabsorption
In relation to renal function, the term reabsorption indicates movement of substances from the tubule (glomerular filtrate) to the blood in the peritubular capillaries. Most reabsorption occurs in the proximal tubule. Almost all glucose and amino acids are reabsorbed; about 80% of water, sodium, potassium, chloride, and most other substances is reabsorbed. As a result, about 20% of the glomerular filtrate enters the loop of Henle. In the descending limb of the loop of Henle, water is reabsorbed; in the ascending limb, sodium is reabsorbed. A large fraction of the total amount of sodium (up to 30%) filtered by the glomeruli is reabsorbed in the loop of Henle. Additional sodium is reabsorbed in the distal tubule, primarily by the exchange of sodium ions for potassium ions secreted by epithelial cells of tubular walls. Final reabsorption of water occurs in the distal tubule and small collecting tubules. The remaining water and solutes are now appropriately called urine.
Antidiuretic hormone from the posterior pituitary gland promotes reabsorption of water from the distal tubules and the collecting ducts of the kidneys. This conserves water needed by the body and produces more concentrated urine. Aldosterone, a hormone from the adrenal cortex, promotes sodium-potassium exchange mainly in the distal tubule and collecting ducts. Thus, aldosterone promotes sodium reabsorption and potassium loss.
Tubular Secretion
The term secretion, in relation to renal function, indicates movement of substances from blood in the peritubular capillaries to glomerular filtrate flowing through the renal tubules. Secretion occurs in the proximal and distal tubules, across the epithelial cells that line the tubules. In the proximal tubule, uric acid, creatinine, hydrogen ions, and ammonia are secreted; in the distal tubule, potassium ions, hydrogen ions, and ammonia are secreted. Secretion of hydrogen ions is important in maintaining acid-base balance in body fluids.
Overview of Conditions Requiring Diuretic Agents
To adequately understand the pharmacologic treatment of fluid volume excess, it is important to understand the causes, pathophysiology, and clinical manifestations of renal disorders.
Etiology
Many clinical conditions alter renal function. In some conditions, excessive amounts of substances (e.g., sodium, water) are retained; in others, needed substances (e.g., potassium, proteins) are eliminated. Causal conditions include cardiovascular, renal, hepatic, and other disorders, which may be managed with diuretic drugs. Burns and trauma or allergic and inflammatory reactions may also lead to fluid shifts or loss.
Pathophysiology
Much of the pathophysiology related to the cause of conditions leading to the use of diuretics is discussed in other chapters. The pathophysiology of conditions producing edema formation (excessive accumulation of fluid in body tissues) is outlined below. Edema interferes with blood flow to tissues. Thus, it interferes with delivery of oxygen and nutrients and removal of metabolic waste products. If severe, edema may distort body features, impair movement, and interfere with activities of daily living.
Edema formation results from one or more of the following mechanisms that allow fluid to leave the bloodstream (intravascular compartment) and enter interstitial (third) spaces:
• Increased capillary permeability occurs as part of the response to tissue injury, including allergic and inflammatory reactions.
• Increased capillary hydrostatic pressure results from a sequence of events in which increased blood volume (from fluid overload or sodium and water retention) or obstruction of venous blood flow causes a high venous pressure and a high capillary pressure. This is the primary mechanism for edema formation in heart failure, pulmonary edema, and renal failure.
• Decreased plasma oncotic pressure may occur with decreased synthesis of plasma proteins (caused by liver disease or malnutrition) or increased loss of plasma proteins (caused by burn injuries or the nephrotic syndrome). Plasma proteins are important in keeping fluids within the bloodstream. When plasma proteins are lacking, fluid seeps through the capillaries and accumulates in tissues.
Clinical Manifestations
• Clinical manifestations reflect the alterations in fluid and electrolyte balance brought on by the inability of the kidneys to control the volume, composition, and pH of body fluids. Edema is a symptom of many disease processes and may occur in any part of the body. Specific manifestations of edema are determined by its location and extent. A common type of localized edema, known as dependent edema, occurs in the feet and ankles, especially with prolonged sitting or standing. A less common but more severe type of localized edema in the lungs is pulmonary edema, a life-threatening condition that occurs with circulatory overload (e.g., of intravenous [IV] fluids, blood transfusions) or acute heart failure. Generalized massive edema, or anasarca, interferes with the functions of many body organs and tissues.
Drug Therapy
Diuretic drugs act on the kidneys to decrease reabsorption of sodium, chloride, water, and other substances. Major subclasses are the thiazides and related diuretics, loop diuretics, and potassium-sparing diuretics, which act at different sites in the nephron (Fig. 32.2). The choice of diuretic drug depends primarily on the patient’s condition.
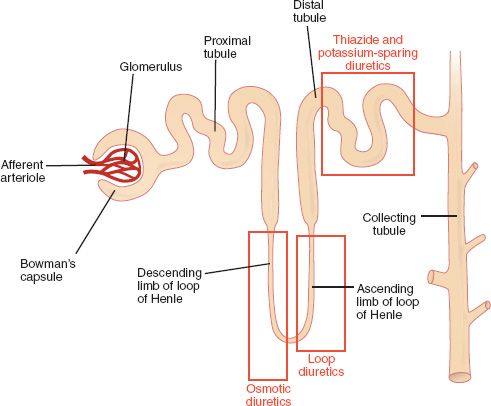
Figure 32.2 Diuretic sites of action in the nephron. Diuretics act at different sites in the nephron to decrease reabsorption of sodium and water and to increase urine output.
Major clinical indications for diuretics are edema, heart failure, and hypertension. In edematous states, diuretics mobilize tissue fluids by decreasing plasma volume. In hypertension, the exact mechanism by which diuretics lower blood pressure is unknown, but antihypertensive action is usually attributed to sodium depletion. Initially, diuretics decrease blood volume and cardiac output. With chronic use, cardiac output returns to normal, but there is a persistent decrease in plasma volume and peripheral vascular resistance. Sodium depletion may have a vasodilating effect on arterioles.
Chapters 24 and 28 further discuss the use of diuretic agents in the management of heart failure and hypertension, respectively. The following section describes the types of diuretics, and Table 32.1 lists individual drugs.
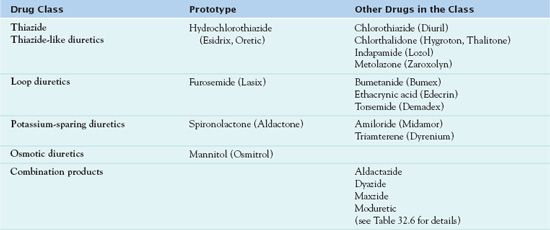
Thiazide Diuretics
Thiazide diuretics are synthetic drugs that are chemically related to the sulfonamides and differ mainly in their duration of action.  Hydrochlorothiazide (Esidrix, Oretic), the most commonly used drug in the class, is the prototype. It is not a strong diuretic and works efficiently only when urine flow is adequate. Thiazide diuretics are the drugs of choice for most patients who require diuretic therapy, especially for long-term management of heart failure and hypertension. All drugs in this group have similar effects.
Hydrochlorothiazide (Esidrix, Oretic), the most commonly used drug in the class, is the prototype. It is not a strong diuretic and works efficiently only when urine flow is adequate. Thiazide diuretics are the drugs of choice for most patients who require diuretic therapy, especially for long-term management of heart failure and hypertension. All drugs in this group have similar effects.
Pharmacokinetics
Hydrochlorothiazide is administered orally and is well absorbed, widely distributed in body fluids, and highly bound to plasma proteins. The drug accumulates only in the kidneys. Diuretic effects usually occur within 2 hours, peak at 4 to 6 hours, and last 6 to 24 hours. Antihypertensive effects usually last long enough to allow use of a single daily dose. Most of the drug is excreted unchanged by the kidneys within 3 to 6 hours.
Action
Hydrochlorothiazide acts to decrease reabsorption of sodium, water, chloride, and bicarbonate in the distal convoluted tubule. Most sodium is reabsorbed before it reaches the distal convoluted tubule and only a small amount is reabsorbed at this site.
Use
Health care providers use hydrochlorothiazide to treat mild to moderate hypertension and the edema associated with heart failure and nephrotic syndrome. For most patients, this drug is effective. Table 32.2 presents route and dosage information for hydrochlorothiazide and the other thiazide diuretics.
 TABLE 32.2
TABLE 32.2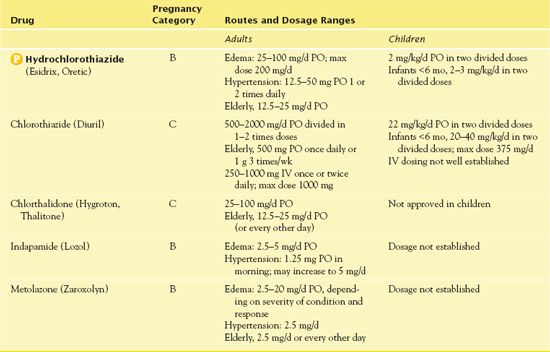
Use in Children
Authorities have not established the safety and effectiveness of hydrochlorothiazide in children. IV chlorothiazide usually is not recommended. Thiazides do not commonly cause hyperglycemia, hyperuricemia, or hypercalcemia in children, as they do in adults.
Use in Older Adults
Prescribers often order hydrochlorothiazide and other thiazide diuretics for the management of hypertension and heart failure, which are common in older adults. Older adults are especially sensitive to adverse drug effects, such as hypotension and electrolyte imbalance. The drug may aggravate renal or hepatic impairment. With rapid or excessive diuresis, myocardial infarction, renal impairment, or cerebral thrombosis may occur from fluid volume depletion and hypotension. The smallest effective dose is recommended. Adverse effects may exceed therapeutic benefits at doses greater than 25 mg.
Use in Patients With Renal Impairment
Hydrochlorothiazide may be useful in managing edema due to renal disorders such as nephrotic syndrome and acute glomerulonephritis. However, its effectiveness decreases as the GFR decreases, and it becomes ineffective when the GFR is less than 30 mL/min. The drug may accumulate and increase adverse effects in patients with impaired renal function. Thus, it is necessary to perform renal function tests periodically.
Use in Patients With Hepatic Impairment
Patients with severe hepatic impairment are at significant risk for thiazide-induced hypokalemic and hypochloremic alkalosis. Hepatic encephalopathy and death have occurred due to the electrolyte imbalances that accompany diuretic therapy. Blood ammonia levels may become increasingly elevated in people with previously elevated ammonia concentrations. Therapy with thiazide diuretics should be administered cautiously in patients with hepatic impairment and discontinued promptly if signs of impending hepatic coma (e.g., increased jaundice, tremors, confusion, and asterixis) appear.
Use in Patients With Critical Illness
Hydrochlorothiazide is ineffective when immediate diuresis is required because of its slow onset of action. The loop diuretics are more likely to be administered in a critical care setting, because more potent diuretic agents may be necessary (see later discussion).
QSEN Safety Alert 
It is important to note that hydrochlorothiazide should not be given the morning of surgery, because it may lead to volume depletion, causing the blood pressure to be labile and undergo frequent changes with general anesthesia.
Use in Patients Receiving Home Care
Diuretics are often taken in the home setting. The home care nurse may need to assist patients and caregivers in using the drugs safely and effectively, monitor patient responses, and provide information as indicated. With each home visit, the nurse assesses nutritional status, blood pressure, weight, and use of over-the-counter medications that may aggravate edema or hypertension.
Adverse Effects
Adverse effects of hydrochlorothiazide include hypersensitivity reactions, hypotension, weakness, dizziness, diarrhea, constipation, electrolyte imbalances (e.g., hyponatremia, hypokalemia, hypochloremia), hyperglycemia, paresthesia, and erectile dysfunction.
Contraindications
Contraindications to hydrochlorothiazide include known sensitivity to thiazides of sulfonamide-derived agents, or renal decompensation or anuria (no urine output).
QSEN Safety Alert 
It is essential to use thiazide diuretics and related drugs cautiously in patients who are allergic to sulfonamide drugs because there is a known cross-sensitivity of some sulfonamide-allergic patients to a sulfonamide nonantibiotic.
Also, caution is necessary during pregnancy because the drug crosses the placenta and may have adverse effects on the fetus by compromising placental perfusion. It may cause an increased risk of congenital defects.
Nursing Implications
Preventing Interactions
Several drugs and herbs increase or decrease the effects of hydrochlorothiazide (Boxes 32.1 and 32.2). The thiazide diuretic can increase the effects of angiotensin-converting enzyme inhibitors, other hypertensive agents, allopurinol, calcitriol, and lithium.
BOX 32.1  Drug Interactions: Hydrochlorothiazide
Drug Interactions: Hydrochlorothiazide
Drugs That Increase the Effects of Hydrochlorothiazide
 Alcohol, barbiturates, monoamine oxidase inhibitors, opioids, phosphodiesterase 5 inhibitors, prostacyclin analogues
Alcohol, barbiturates, monoamine oxidase inhibitors, opioids, phosphodiesterase 5 inhibitors, prostacyclin analogues
Increase hypotensive effects, possibly contributing to orthostasis
 Beta-blockers
Beta-blockers
Increase the risk of hyperglycemia, hyperlipidemia, and hyperuricemia
 Carbamazepine
Carbamazepine
Increases the risk of hyponatremia
 Chlorpropamide, corticosteroids, digoxin
Chlorpropamide, corticosteroids, digoxin
Increase the risk of hypokalemia
Drugs That Decrease the Effects of Hydrochlorothiazide
 Cholestyramine
Cholestyramine
May significantly decrease absorption
 Methylphenidate, nonsteroidal anti-inflammatory drugs, yohimbine
Methylphenidate, nonsteroidal anti-inflammatory drugs, yohimbine
Decrease hypotensive effects
BOX 32.2  Herb and Dietary Interactions: Hydrochlorothiazide, Furosemide, and Spironolactone
Herb and Dietary Interactions: Hydrochlorothiazide, Furosemide, and Spironolactone
Herbs and Foods That Increase the Effects of These Diuretics
 Black cohosh
Black cohosh
 California poppy
California poppy
 Coleus
Coleus
 Goldenseal
Goldenseal
 Hawthorn
Hawthorn
 Mistletoe
Mistletoe
 Periwinkle
Periwinkle
 Quinine
Quinine
 Shepherd’s purse
Shepherd’s purse
Herbs and Foods That Decrease the Effects of These Diuretics
 American ginseng
American ginseng
 Bayberry
Bayberry
 Blue cohosh
Blue cohosh
 Ginger
Ginger
 Kola
Kola
 Licorice
Licorice
 Foods
Foods
Administering the Medication
Hydrochlorothiazide, like all thiazide diuretics, has a ceiling threshold, which means that a certain dose yields a near-maximum diuretic response. This dose, known as the ceiling dose, is dependent on the type of diuretic and the extent of a person’s disease. As the maximum effect is reached, a subsequent increase in dose does not enhance efficacy. In addition, there is a direct correlation between the dosage increase and the possible onset of adverse effects. When the diuretic dose is less than at ceiling, fluid retention remains following diuresis.
Assessing for Therapeutic Effects
The nurse assesses for the return of blood pressure to acceptable levels and improvement in the edema associated with heart failure and nephrotic syndrome.
Assessing for Adverse Effects
Monitoring for transient or irreversible hearing impairment, tinnitus, or dizziness is important. Ototoxicity is more likely to occur with high serum drug levels (e.g., high doses or in patients with severe renal impairment) or when other ototoxic drugs (e.g., aminoglycoside antibiotics) are being taken concurrently.
Patient Teaching
The nurse instructs the patient regarding the importance of taking the medication as prescribed, keeping follow-up appointments, and watching for signs and symptoms of adverse effects. Box 32.3 presents general patient teaching guidelines, which are a good reference.
BOX 32.3  Patient Teaching Guidelines for Diuretics
Patient Teaching Guidelines for Diuretics



