Recognize the role of dyslipidemia in metabolic syndrome.
 Identify sources and functions of cholesterol and triglycerides.
Identify sources and functions of cholesterol and triglycerides.
 Educate patients about nonpharmacologic measures to prevent or reduce dyslipidemia.
Educate patients about nonpharmacologic measures to prevent or reduce dyslipidemia.
 Identify the prototype drug from each drug class used to treat dyslipidemia.
Identify the prototype drug from each drug class used to treat dyslipidemia.
 Describe the classes of dyslipidemic drugs in terms of their mechanism of action, indications for use, major adverse effects, and nursing implications.
Describe the classes of dyslipidemic drugs in terms of their mechanism of action, indications for use, major adverse effects, and nursing implications.
 Apply the nursing process in the care of patients with dyslipidemia.
Apply the nursing process in the care of patients with dyslipidemia.
Clinical Application Case Study
Edward Watkins, a 62-year-old man, has had elevated cholesterol and triglyceride levels at his two previous visits to the nurse practitioner. He has tried diet modification and increasing exercise; however, he remains overweight and his lipid values remain elevated. His latest laboratory findings at this visit are total serum cholesterol 239 mg/dL, low-density lipoprotein cholesterol 162 mg/dL, high-density lipoprotein cholesterol 40 mg/dL, and triglycerides 220 mg/dL. His nurse practitioner decides to prescribe atorvastatin 10 mg PO once daily and gemfibrozil 600 mg PO twice a day.
KEY TERMS
Central adiposity: accumulation of abdominal fat, resulting in an increased waist circumference
Cholesterol: component of cell membrane that is produced and processed in the liver; a fat essential for the formation of steroid hormones that is produced in cells and taken in by dietary sources
Dyslipidemia: abnormal lipid levels in the blood; associated with atherosclerosis and its many pathophysiologic effects (e.g., myocardial ischemia and infarction, stroke, peripheral arterial occlusive disease)
Lipoproteins: specific proteins in plasma that transport blood lipids; contain cholesterol, phospholipid, and triglyceride bound to protein. They vary in density and amounts of lipid and protein
Metabolic syndrome: cluster of several cardiovascular risk factors linked with obesity: increased waist circumference, elevated triglycerides, reduced high-density lipoprotein cholesterol, elevated blood pressure, and elevated fasting glucose
Introduction
Although therapeutic lifestyle changes are the cornerstone of population-based interventions to manage dyslipidemia, they are often insufficient in achieving recommended treatment targets. When lifestyle changes alone do not reduce blood lipids, dyslipidemic drugs are used in the management of patients with elevated blood lipids, a major risk factor for atherosclerosis and vascular disorders such as coronary artery disease, strokes, and peripheral arterial insufficiency. These drugs have proven efficacy and are increasingly being used to reduce morbidity and mortality from coronary heart disease and other atherosclerosis-related cardiovascular disorders. Dyslipidemic drugs are used to decrease blood lipids, prevent or delay the development of atherosclerotic plaque, promote the regression of existing atherosclerotic plaque, and reduce morbidity and mortality from cardiovascular disease. To understand the clinical use of these drugs, it is necessary to understand characteristics of blood lipids, metabolic syndrome, and types of blood lipid disorders.
Overview of Dyslipidemia
Etiology
Blood lipids, which include cholesterol, phospholipids, and triglycerides, are derived from the diet or synthesized by the liver and intestine. Most cholesterol is found in body cells, where it is a component of cell membranes and performs other essential functions. In cells of the adrenal glands, ovaries, and testes, cholesterol is required for the synthesis of steroid hormones (e.g., cortisol, estrogen, progesterone, testosterone). In liver cells, cholesterol is used to form cholic acid, which is conjugated with other substances to form bile salts; these salts promote absorption and digestion of fats. In addition, a small amount of cholesterol is found in blood serum. Serum cholesterol is the portion of total body cholesterol involved in formation of atherosclerotic plaques. Unless a person has a genetic disorder of lipid metabolism, the amount of cholesterol in the blood is strongly related to dietary intake of saturated fat. Phospholipids are essential components of cell membranes, and triglycerides provide energy for cellular metabolism.
Blood lipids are transported in plasma by specific proteins called lipoproteins. Each lipoprotein contains cholesterol, phospholipid, and triglyceride bound to protein. The lipoproteins vary in density and amounts of lipid and protein. Density is determined mainly by the amount of protein, which is more dense than fat. Thus, density increases as the proportion of protein increases. The lipoproteins are differentiated according to these properties, which can be measured in the laboratory. For example, high-density lipoprotein (HDL) cholesterol contains larger amounts of protein and smaller amounts of lipid; low-density lipoprotein (LDL) cholesterol contains less protein and larger amounts of lipid. Other plasma lipoproteins are chylomicrons and very-low-density lipoproteins (VLDLs). Additional characteristics of lipoproteins are described in Box 8.1.
BOX 8.1 Types of Lipoproteins
Chylomicrons, the largest lipoprotein molecules, are synthesized in the wall of the small intestine. They carry recently ingested dietary cholesterol and triglycerides that have been absorbed from the gastrointestinal tract. Hyperchylomicronemia normally occurs after a fatty meal, reaches peak levels in 3 to 4 hours, and subsides within 12 to 14 hours. Chylomicrons carry triglycerides to fat and muscle cells, where the enzyme lipoprotein lipase breaks down the molecule and releases fatty acids to be used for energy or stored as fat. This process leaves a remnant containing cholesterol, which is then transported to the liver. Thus, chylomicrons transport triglycerides to peripheral tissues and cholesterol to the liver.
Low-density lipoprotein (LDL) cholesterol, sometimes called “bad cholesterol,” transports approximately 75% of serum cholesterol and carries it to peripheral tissues and the liver. LDL cholesterol is removed from the circulation by receptor and nonreceptor mechanisms. The receptor mechanism involves the binding of LDL cholesterol to receptors on cell surface membranes. The bound LDL molecule is then engulfed into the cell, where it is broken down by enzymes and releases free cholesterol into the cytoplasm.
Most LDL cholesterol receptors are located in the liver. However, nonhepatic tissues (e.g., adrenal glands, smooth muscle cells, endothelial cells, and lymphoid cells) also have receptors by which they obtain the cholesterol needed for building cell membranes and synthesizing hormones. These cells can regulate their cholesterol intake by adding or removing LDL receptors.
Approximately two thirds of the LDL cholesterol is removed from the bloodstream by the receptor-dependent mechanism. The number of LDL receptors on cell membranes determines the amount of LDL degradation (i.e., the more receptors on cells, the more LDL is broken down). Conditions that decrease the number or function of receptors (e.g., high dietary intake of cholesterol, saturated fat, or calories) increase blood levels of LDL.
The remaining one third is removed by mechanisms that do not involve receptors. Nonreceptor uptake occurs in various cells, especially when levels of circulating LDL cholesterol are high. For example, macrophage cells in arterial walls can attach LDL, thereby promoting accumulation of cholesterol and the development of atherosclerosis. The amount of LDL cholesterol removed by nonreceptor mechanisms is increased with inadequate numbers of receptors or excessive amounts of LDL cholesterol.
A high serum level of LDL cholesterol is atherogenic and a strong risk factor for coronary heart disease. The body normally attempts to compensate for high serum levels by inhibiting hepatic synthesis of cholesterol and cellular synthesis of new LDL receptors.
Very-low-density lipoprotein (VLDL) contains approximately 75% triglycerides and 25% cholesterol. It transports endogenous triglycerides (those synthesized in the liver and intestine, not those derived exogenously, from food) to fat and muscle cells. There, as with chylomicrons, lipoprotein lipase breaks down the molecule and releases fatty acids to be used for energy or stored as fat. The removal of triglycerides from VLDL leaves a cholesterol-rich remnant, which returns to the liver. Then the cholesterol is secreted into the intestine, mostly as bile acids, or it is used to form more VLDL and recirculated.
High-density lipoprotein (HDL) cholesterol, often referred to as “good cholesterol,” is a small but very important lipoprotein. It is synthesized in the liver and intestine, and some is derived from the enzymatic breakdown of chylomicrons and VLDL. It contains moderate amounts of cholesterol. However, this cholesterol is transported from blood vessel walls to the liver for catabolism and excretion. This reverse transport of cholesterol has protective effects against coronary heart disease.
The mechanisms by which HDL cholesterol exerts protective effects are unknown. Possible mechanisms include clearing cholesterol from atheromatous plaque, increasing excretion of cholesterol so less is available for reuse in the formation of LDL cholesterol, and inhibiting cellular uptake of LDL cholesterol. Regular exercise and moderate alcohol consumption are associated with increased levels of HDL cholesterol; obesity, diabetes mellitus, genetic factors, smoking, and some medications (e.g., steroids and beta-blockers) are associated with decreased levels. HDL cholesterol levels are not directly affected by diet.
Pathophysiology
Dyslipidemia (also called hyperlipidemia because increased blood levels of lipoproteins accompany increased blood lipid levels), abnormal lipid levels in the blood, is associated with atherosclerosis and its many pathophysiologic effects (e.g., myocardial ischemia and infarction, stroke, peripheral arterial occlusive disease). (Because increased blood levels of lipoproteins accompany increased blood lipid levels, dyslipidemia is also called hyperlipidemia.) Ischemic heart disease has a high rate of morbidity and mortality. Elevated total cholesterol and LDL cholesterol and reduced HDL cholesterol are the abnormalities that are major risk factors for coronary artery disease. Elevated triglycerides also play a role in cardiovascular disease. For example, high blood levels reflect excessive caloric intake (excessive dietary fats are stored in adipose tissue; excessive proteins and carbohydrates are converted to triglycerides and also stored in adipose tissue) and obesity. High caloric intake also increases the conversion of VLDL to LDL cholesterol, and high dietary intake of triglycerides and saturated fat decreases the activity of LDL receptors and increases synthesis of cholesterol. Very high triglyceride levels are associated with acute pancreatitis.
Dyslipidemia may be primary (i.e., genetic or familial) or secondary to dietary habits, other diseases (e.g., diabetes mellitus, alcoholism, hypothyroidism, obesity, obstructive liver disease), and medications (e.g., beta-blockers, cyclosporine, oral estrogens, glucocorticoids, sertraline, thiazide diuretics, anti– human immunodeficiency virus [HIV] protease inhibitors).
Metabolic syndrome is a group of cardiovascular risk factors linked with obesity. The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (NCEP III) clustered several elements of metabolic syndrome: central adiposity (increased waist circumference), elevated triglycerides, reduced HDL cholesterol, elevated blood pressure, and elevated fasting glucose. These risk factors frequently have an additive effect in the development of cardiovascular, cerebrovascular, and peripheral vascular disease, and they are principal contributors to the significant morbidity and mortality of these conditions. Improvements in insulin resistance and lipid profiles are essential lifestyle modifications and constitute first-line treatment of metabolic syndrome. This chapter specifically addresses management of components of metabolic syndrome related to dyslipidemia; an additional discussion of other factors is found in Chapters 26 and 39.
Clinical Manifestations
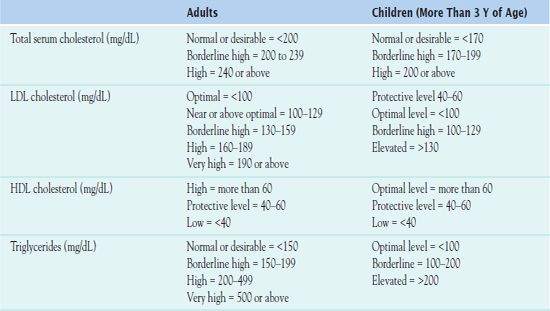
A lipid profile consists of a total cholesterol, HDL cholesterol, LDL cholesterol, and triglycerides. For accurate interpretation, blood samples for laboratory testing of triglycerides should be drawn after the patient has fasted for 12 hours. Fasting is not required for cholesterol testing. Normal lipid levels in adults and children are outlined in Table 8.1. Types of dyslipidemias are described in Box 8.2. Although hypercholesterolemia is usually emphasized, hypertriglyceridemia is also associated with most types of hyperlipoproteinemia.
BOX 8.2 Types of Dyslipidemias
Type I is characterized by elevated or normal serum cholesterol, elevated triglycerides, and chylomicronemia. This rare condition may occur in infancy and childhood.
Type IIa (familial hypercholesterolemia) is characterized by a high level of low-density lipoprotein (LDL) cholesterol, a normal level of very-low-density lipoprotein (VLDL), and a normal or slightly increased level of triglycerides. It occurs in children and is a definite risk factor for development of atherosclerosis and coronary artery disease.
Type IIb (combined familial hyperlipoproteinemia) is characterized by increased levels of LDL, VLDL, cholesterol, and triglycerides and lipid deposits (xanthomas) in the feet, knees, and elbows. It occurs in adults.
Type III is characterized by elevations of cholesterol and triglycerides plus abnormal levels of LDL and VLDL. This type usually occurs in middle-aged adults (40-60 years) and is associated with accelerated coronary and peripheral vascular disease.
Type IV is characterized by normal or elevated cholesterol levels, elevated triglycerides, and increased levels of VLDL. This type usually occurs in adults and may be the most common form of hyperlipoproteinemia. Type IV is often secondary to obesity, excessive intake of alcohol, or other diseases. Ischemic heart disease may occur at 40 to 50 years of age.
Type V is characterized by elevated cholesterol and triglyceride levels with an increased level of VLDL and chylomicronemia. This uncommon type usually occurs in adults. Type V is not associated with ischemic heart disease. Instead, it is associated with fat and carbohydrate intolerance, abdominal pain, and pancreatitis, which are relieved by lowering triglyceride levels.
Additionally, the total cholesterol–to–HDL cholesterol ratio is a number that is useful in predicting the risk of developing atherosclerosis (total cholesterol value is divided by the value of the HDL cholesterol). The ideal ratio is less than 4. Even with a favorable ratio, it is still important to try to obtain an LDL of less than 80 to 100 mg/dL, particularly in the presence of multiple other risk factors for coronary artery disease.
Management
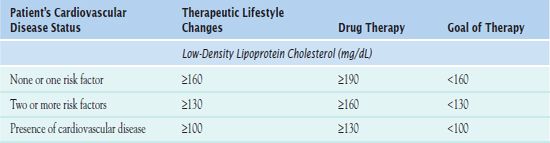
Overall, the most effective blood lipid profile for prevention or management of metabolic syndrome and its sequelae is high HDL cholesterol, low LDL cholesterol, and low total cholesterol. A low triglyceride level is also desirable. NCEP III classified blood lipid levels and has summarized the current recommendations for the management of dyslipidemia based on a person’s blood levels of total and LDL cholesterol and risk factors for cardiovascular disease (Table 8.2). Note that therapeutic lifestyle changes, including exercise, smoking cessation, changes in diet, and drug therapy, are recommended at lower serum cholesterol levels in patients who already have cardiovascular disease or diabetes mellitus. Also, the target LDL serum level is lower in these patients.
Lifestyle Changes
The NCEP III proposed the following guidelines as treatment goals for patients with lipid abnormalities:
• Assess for, and treat, if present, conditions known to increase blood lipids (e.g., diabetes mellitus, hypothyroidism).
• Stop medications known to increase blood lipids, if possible.
• Start a low-fat diet. A step I diet contains no more than 30% of calories from fat, less than 10% of calories from saturated fats (e.g., meat, dairy products), and less than 300 mg of cholesterol per day. A step II diet contains no more than 30% of calories from fat, less than 7% of calories from saturated fat, and less than 200 mg of cholesterol per day. The step II diet is more stringent and may be used initially in patients with more severe dyslipidemia, cardiovascular disease, or diabetes mellitus. It can decrease LDL cholesterol levels by 8% to 15%. Diets with more stringent fat restrictions than the step II diet are not recommended because they produce little additional reduction in LDL cholesterol, raise serum triglyceride levels, and lower HDL cholesterol concentrations.
• Use the “Mediterranean diet,” which includes moderate amounts of monounsaturated fats (e.g., canola, olive oils) and polyunsaturated fats (e.g., safflower, corn, cottonseed, sesame, soybean, sunflower oils), to also decrease risks of cardiovascular disease.
• Increase dietary intake of soluble fiber (e.g., psyllium preparations, oat bran, pectin, fruits, and vegetables). This diet lowers serum LDL cholesterol by 5% to 10%.
• Dietary supplements (e.g., Cholestin) and cholesterol-lowering margarines (e.g., Benecol, Take Control) can help reduce cholesterol levels. These products are considered to be foods, not drugs, and are costly.
• Start a weight-reduction diet if the patient is overweight or obese. Weight loss can increase HDL and decrease LDL.
• Emphasize regular aerobic exercise (usually 30 minutes at least three times weekly). This strategy increases blood levels of HDL.
• If the patient smokes, help develop a cessation plan. In addition to numerous other benefits, HDL levels are higher in nonsmokers.
• If the patient is postmenopausal, hormone replacement therapy can raise HDL and lower LDL.
• If the patient has elevated serum triglycerides, initial management includes efforts to achieve desirable body weight, ingest low amounts of saturated fat and cholesterol, exercise regularly, stop smoking, and reduce alcohol intake, if indicated. The goal is to reduce serum triglyceride levels to 200 mg/dL or less.
• Unless lipid levels are severely elevated, 6 months of intensive diet therapy and lifestyle modification may be undertaken before drug therapy is considered. It is essential that therapeutic lifestyle changes continue during drug therapy because the benefits of diet, exercise, and drug therapy are additive.
Box 8.3 identifies some herbs and foods that have a known effect on cholesterol.
BOX 8.3 Herbs and Foods Known to Have an Effect on Cholesterol and Triglyceride Levels
 Garlic, an herb, may lower cholesterol and triglycerides. However, there is little scientific support for this therapy. Bleeding may be increased when garlic is combined with anticoagulants, and insulin doses may need to be decreased as a result of the hypoglycemic effect of garlic.
Garlic, an herb, may lower cholesterol and triglycerides. However, there is little scientific support for this therapy. Bleeding may be increased when garlic is combined with anticoagulants, and insulin doses may need to be decreased as a result of the hypoglycemic effect of garlic.
 Flax or flax seed, used internally as a laxative and a dyslipidemic agent. Absorption of all medications may be decreased when taken with flax, resulting in a less than therapeutic effect.
Flax or flax seed, used internally as a laxative and a dyslipidemic agent. Absorption of all medications may be decreased when taken with flax, resulting in a less than therapeutic effect.
 Soy, used as a food source and has been researched extensively. Use of soy to lower total and LDL cholesterol has been documented. Additionally, it is possible that an intake of soy proteins may have other beneficial vascular effects.
Soy, used as a food source and has been researched extensively. Use of soy to lower total and LDL cholesterol has been documented. Additionally, it is possible that an intake of soy proteins may have other beneficial vascular effects.
 Plant-derived stanol and sterol esters, which are added to margarine and other food products. These substances may also help lower total and LDL cholesterol. However, cholesterol-lowering margarines containing plant sterols cost approximately two to five times that of ordinary margarine. (Products such as orange juice and other beverages containing lecithin emulsified plant stanols have reduced total and LDL cholesterol to a similar degree as the margarines.) In addition, little is known about their long-term effects, and researchers have shown that plant sterol supplementation may have caused harmful vascular effects in animals.
Plant-derived stanol and sterol esters, which are added to margarine and other food products. These substances may also help lower total and LDL cholesterol. However, cholesterol-lowering margarines containing plant sterols cost approximately two to five times that of ordinary margarine. (Products such as orange juice and other beverages containing lecithin emulsified plant stanols have reduced total and LDL cholesterol to a similar degree as the margarines.) In addition, little is known about their long-term effects, and researchers have shown that plant sterol supplementation may have caused harmful vascular effects in animals.
 Theaflavin, found in green tea, which has been shown to lower total cholesterol and low-density lipoprotein-cholesterol complex
Theaflavin, found in green tea, which has been shown to lower total cholesterol and low-density lipoprotein-cholesterol complex
 Red yeast rice, which has been shown to lower cholesterol. However, dosage standardization is a concern, and information about long-term safety is unavailable.
Red yeast rice, which has been shown to lower cholesterol. However, dosage standardization is a concern, and information about long-term safety is unavailable.
Clinical Application 8-1
 What is the purpose of attempting weight reduction and increasing activity for Mr. Watkins before starting dyslipidemic medications?
What is the purpose of attempting weight reduction and increasing activity for Mr. Watkins before starting dyslipidemic medications?
 How would the nurse interpret the current laboratory values of Mr. Watkins?
How would the nurse interpret the current laboratory values of Mr. Watkins?
NCLEX Success
1. The primary focus for prevention and management of metabolic syndrome and its sequelae is
A. elevated high-density lipoprotein (HDL) cholesterol, depressed low-density lipoprotein (LDL) cholesterol, low total cholesterol
B. low HDL cholesterol, low LDL cholesterol, low total cholesterol
C. low triglycerides
D. high HDL cholesterol, low LDL cholesterol, low triglycerides
2. A person with type 1 diabetes mellitus and hypertension has the following lipid profile: total serum cholesterol 288 mg/dL, low-density lipoprotein (LDL) cholesterol 200 mg/dL, high-density lipoprotein (HDL) cholesterol 48 mg/dL, and triglycerides 200 mg/dL. The patient’s total cholesterol–to–HDL cholesterol ratio and relative cardiac risk is
A. 4.0, with an increased risk of developing atherosclerosis, particularly in the presence of multiple other risk factors for coronary artery disease
B. 4.5, with no risk of developing atherosclerosis
C. 5.0, with no risk of developing atherosclerosis
D. 6.0, with an increased risk of developing atherosclerosis, particularly in the presence of multiple other risk factors for coronary artery disease
3. A 48-year-old man visits his health care provider for his annual checkup. He is otherwise in good health, but assessment findings reveal the new onset of a slight increase in blood pressure and a total serum cholesterol of 240 mg/dL. What can the nurse anticipate as the preferred treatment for this patient?
A. a low-lipid diet and an exercise program
B. a low-lipid diet and a cholesterol synthesis inhibitor
C. an exercise program and a fibrate
D. a low-lipid diet, an exercise program, and niacin
Drug Therapy
Clinical data suggest that drug therapy may be efficacious even for those with mild to moderate elevations of LDL cholesterol. Dyslipidemic drugs act by altering the production, absorption, metabolism, or removal of lipids and lipoproteins. Drug therapy is initiated when 6 months of dietary and other lifestyle changes fail to decrease dyslipidemia to an acceptable level. It is also recommended for patients with signs and symptoms of coronary heart disease, a strong family history of coronary heart disease or dyslipidemia, or other risk factors for atherosclerotic vascular disease (e.g., hypertension, diabetes mellitus, cigarette smoking). Although several dyslipidemic drugs are available, none is effective in all types of dyslipidemia.
Drug selection is based on the type of dyslipidemia and its severity. To lower cholesterol using a single drug, a statin is preferred. To lower cholesterol and triglycerides, a statin, a cholesterol absorption inhibitor, gemfibrozil, a fibrate, or the vitamin niacin may be used. To lower triglycerides, gemfibrozil, ezetimibe, a cholesterol absorption inhibitor, or niacin may be given. Gemfibrozil, rather than niacin, is usually preferred for people with diabetes because niacin increases blood sugar.
Categories of drugs are described in upcoming sections. Table 8.3 and the DRUGS AT A GLANCE tables list individual drugs used in the treatment of dyslipidemia. Figure 8.1 shows the sites of action of dyslipidemic drugs.
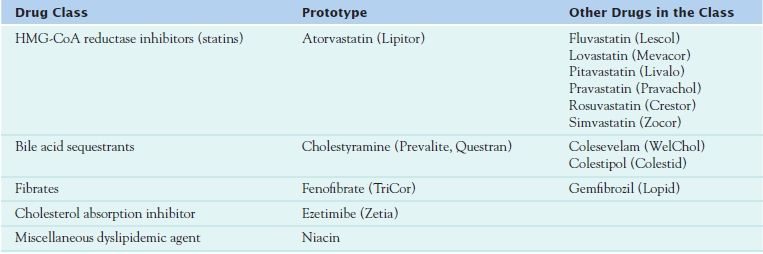
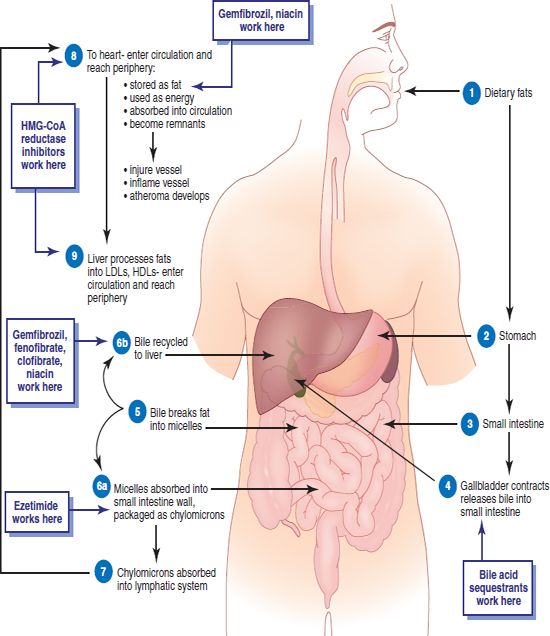
Figure 8.1 Sites of action of dyslipidemic drugs.
HMG-CoA Reductase Inhibitors
 Atorvastatin (Lipitor), one of the most widely used drugs in the United States, is the prototype of the class of drugs called the hydroxymethylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors, or statins. By decreasing production of cholesterol, the statins decrease total serum cholesterol, LDL cholesterol, VLDL cholesterol, and triglycerides. They reduce LDL cholesterol within 2 weeks and reach maximal effects in approximately 4 to 6 weeks. HDL cholesterol levels remain unchanged or may increase.
Atorvastatin (Lipitor), one of the most widely used drugs in the United States, is the prototype of the class of drugs called the hydroxymethylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors, or statins. By decreasing production of cholesterol, the statins decrease total serum cholesterol, LDL cholesterol, VLDL cholesterol, and triglycerides. They reduce LDL cholesterol within 2 weeks and reach maximal effects in approximately 4 to 6 weeks. HDL cholesterol levels remain unchanged or may increase.
The most commonly prescribed statin, atorvastatin, is useful for treating dyslipidemia and is an overall tool in the primary prevention of cardiovascular disease. Lack of evidence or inconsistent findings concerning the use of statins in women, in people older than 65 years of age, and in people with diabetes mellitus without known cardiovascular disease have led to much controversy concerning the role of statins in primary cardiovascular prevention. The Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) supported the use of the dyslipidemic agents in these clinically defined groups. Atorvastatin and other statins also reduce the risk of angina pectoris and peripheral arterial disease as well as the need for angioplasty and coronary artery grafting to increase or restore blood flow to the myocardium.
Several studies have suggested that atorvastatin may possess some benefits that other statins do not. Research has focused on multiple outcomes, including intimal thickness, results of imaging studies, mortality, incidence of stroke, and progression of lesions, but there continue to be questions about the benefit profiles of individual drugs.
Pharmacokinetics
Atorvastatin is rapidly absorbed following oral administration and undergoes extensive first-pass metabolism by the liver, which results in low levels of drug available for general circulation. Peak effect occurs in 1 to 2 hours. Food decreases the rate and extent of absorption. Metabolism occurs in the liver, with 80% to 85% of drug metabolites excreted in feces and the remaining products excreted in urine.
Action
The statins inhibit an enzyme (HMG-CoA reductase) required for hepatic synthesis of cholesterol. In part, metabolism involves one or more hepatic cytochrome P450 enzymes (including CYP2D6), leading to an increased risk of drug interactions and problems with certain foods (e.g., grapefruit juice). Additionally, some of the variability in the response to statins and associated adverse effects statins may relate to genetic differences in the rate of drug metabolism. For example, a CYP2D6 functional deficiency is present in about seven percent of Caucasians and African Americans, and this deficiency is rare in people of Asian descent.
Use
Atorvastatin and the other statins are indicated for the treatment of hypercholesterolemia and reducing cardiovascular events in people with multiple risk factors. The statins are the most powerful drug class for reduction of LDL cholesterol but are expensive. These drugs also decrease triglyceride levels and raise HDL levels. In renal impairment, plasma levels are not affected, and dosage reductions are not necessary.
Table 8.4 presents dosage information for atorvastatin and other statins.
 TABLE 8.4
TABLE 8.4Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


