Understand the etiology and pathophysiology of adrenal cortex disorders.
 Identify the major manifestations of Addison’s disease and Cushing’s disease.
Identify the major manifestations of Addison’s disease and Cushing’s disease.
 Explain how corticotropin (ACTH) is used in the diagnosis of adrenocortical insufficiency.
Explain how corticotropin (ACTH) is used in the diagnosis of adrenocortical insufficiency.
 Explain how cosyntropin (Cortrosyn) is used in the diagnosis of adrenocortical insufficiency.
Explain how cosyntropin (Cortrosyn) is used in the diagnosis of adrenocortical insufficiency.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the drugs used in the treatment of Addison’s disease.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the drugs used in the treatment of Addison’s disease.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the drugs used in the treatment of Cushing’s disease.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the drugs used in the treatment of Cushing’s disease.
 Implement the nursing process in the care of the patient with Addison’s disease or Cushing’s disease.
Implement the nursing process in the care of the patient with Addison’s disease or Cushing’s disease.
Clinical Application Case Study
Rosa James is a 68-year-old woman who is being seen by her physician with symptoms of muscle weakness and fatigue. She states that she has felt depressed. Physical assessment reveals dark pigmentation of the mucous membranes and skin on the knuckles, knees, and elbows. She appears dehydrated with poor skin turgor. Her blood pressure is extremely low—84/50 mm Hg. Blood chemistry reveals of sodium level of 132 mEq/L and a potassium level of 5.5 mEq/L. Mrs. James is admitted to the hospital with suspected Addison’s disease.
KEY TERMS
Addisonian crisis: acute adrenocortical insufficiency
Adrenocortical excess: increase in adrenocortical function
Adrenocortical insufficiency: decrease in adrenocortical function
Introduction
Chapter 15 discussed corticosteroids, and Chapter 41 addressed the types of hormones secreted by the hypothalamus, including corticotropin-releasing hormone (CRH). This chapter introduces the pharmacological care of the patient with adrenocortical insufficiency and the patient with adrenocortical excess. The adrenal glands are attached to the upper portion of each kidney. The adrenal cortex of each adrenal gland secretes steroid hormones. The hypothalamic–pituitary–adrenal (HPA) axis regulates hormone secretion. The hypothalamus secretes CRH, which in turn stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH) (Fig. 43.1). The ACTH then stimulates the adrenal cortex to secrete glucocorticoid hormone (cortisol). As the levels of adrenal or steroid hormones increase, the levels of CRH and ACTH decrease; this is a negative feedback mechanism (Smeltzer, Bare, Hinkle, & Cheever, 2010).
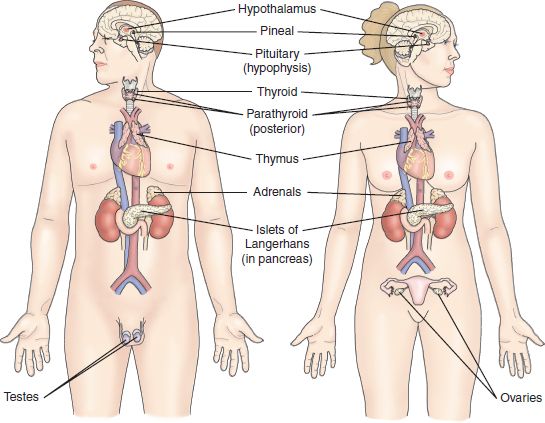
Figure 43.1 The adrenal glands are located on the top of each kidney. Adrenocorticotropic hormone is secreted by the pituitary gland.
Overview of Addison’s Disease
Etiology and Pathophysiology
There are two forms of adrenocortical insufficiency. Primary adrenal insufficiency, or Addison’s disease, occurs when adrenal cortical hormones are deficient. ACTH levels are elevated because the feedback mechanism is not working. Secondary adrenal insufficiency occurs when there is a disorder in the HPA system.
Primary adrenal insufficiency most commonly results from an autoimmune disorder that has destroyed the layers of the adrenal cortex. Other causes of adrenal cortex destruction include metastatic carcinoma, fungal infections such as histoplasmosis, cytomegalovirus, amyloid disease, and hemochromatosis. Hemorrhage of the adrenal cortex related to anticoagulant therapy, open heart surgery, giving birth, or trauma also leads to primary adrenal insufficiency.
Secondary adrenal cortical insufficiency results from hypopituitarism or surgical removal of pituitary gland (Porth & Matfin, 2009). The abrupt withdrawal of oral glucocorticoids also causes secondary adrenal insufficiency. Patients who have endogenous steroid production from a nonendocrine tumor have adrenocortical insufficiency.
Primary adrenocortical insufficiency is associated with the destruction of the adrenal cortex. The resulting deficiency in the mineralocorticoids causes an increase in the loss of urinary sodium, chloride, and water. The patient becomes hyponatremic, and the cardiac output decreases. This progression of the disease is known as Addisonian crisis. The loss of sodium leads to retention of potassium, resulting in symptoms of hyperkalemia.
Clinical Application 43-1
 Mrs. James is hyponatremic. When assessing her cardiac status, what findings would the nurse expect?
Mrs. James is hyponatremic. When assessing her cardiac status, what findings would the nurse expect?
 On the 2nd day of Mrs. James’ hospital admission, her sodium level is 125 mEq/L. What condition does the nurse suspect?
On the 2nd day of Mrs. James’ hospital admission, her sodium level is 125 mEq/L. What condition does the nurse suspect?
Clinical Manifestations
Clinical manifestations of adrenocortical insufficiency are evident when approximately 90% of the adrenal cortex has been destroyed. These signs and symptoms reflect loss of sodium, water, and chloride. Findings include decreased cardiac output, dehydration, weakness, and fatigue. Excessive sodium loss results in cardiovascular collapse and shock. Other symptoms include lethargy, weakness, fever, anorexia, nausea, vomiting, and weight loss. Hyperkalemia and hypoglycemia are present. (Any patient with unexplained severe hypoglycemia requires assessment for adrenal insufficiency (Nieman, 2011).) Hyperpigmentation of the gums and mucous membranes is also present; they may be bluish black. Women have diminished axillary and pubic hair, but men have few effects from the lack of androgens due to the production of hormones by the testes (Porth & Matfin, 2009).
Acute adrenal crisis, or Addisonian crisis, is a life-threatening condition that occurs when Addison’s disease is the underlying problem and the patient is exposed to minor illness or increased stress. Nausea, vomiting, hypotension, muscle weakness, and vascular collapse are present (Smeltzer, et al., 2010; Porth & Matfin, 2009). There may be a craving for salt.
NCLEX Success
1. A man is admitted to the emergency department. He is hypotensive with nausea, vomiting, and muscle weakness. He has been taking enoxaparin (Lovenox) 40 mg subcutaneously daily for the past 2 weeks. It is suspected that he has developed which of the following disorders?
A. hyperglycemia related to diabetes insipidus
B. sepsis related to his heart surgery
C. hemorrhage of the adrenal cortex
D. hyponatremia and cardiovascular collapse
2. A woman visits the clinic. She states that she has been satisfying her recent cravings for salt by eating large quantities of potato chips and other salty foods. She has been under a great deal of stress, and last week she received treatment for pneumonia. What do these symptoms suggest?
A. heart failure
B. Addisonian crisis
C. hypernatremia
D. thyrotoxicosis
Diagnosis
According to Smeltzer et al. (2010), patients commonly present to their primary health care provider with vague symptoms of adrenocortical insufficiency. However, as the adrenocortical insufficiency progresses, acute hypotension results and Addisonian crisis may develop. Making the diagnosis of adrenocortical insufficiency involves laboratory work. This includes early morning serum Cortisol and plasma ACTH levels. A serum Cortisol level less than 3 mcg/dL, or 80 nmol/L, is indicative of adrenocortical insufficiency. (The normal morning level of serum Cortisol is greater—10 to 20 mcg/dL, or 275 to 555 nmol/L.) An ACTH level greater than 22.0 nmol/L is indicative of (primary) adrenocortical insufficiency. (The normal morning level of ACTH is less than 18 nmol/L.)
Confirming the diagnosis of adrenocortical insufficiency requires a short plasma corticotropin stimulation test. The examiner administers corticotropin in the morning, and a subnormal blood Cortisol level in the morning and afternoon confirms the diagnosis. A higher Cortisol level in the morning is a sign that a person does not have adrenal insufficiency. In a patient with adrenal insufficiency, the response to the corticotropin, or ACTH, is the same both morning and afternoon.
Another test that confirms the diagnosis of adrenocortical insufficiency is the standard high-dose test. It is a three-step process:
1. Measurement of baseline serum Cortisol
2. Intravenous (IV) administration of 250 meg of ACTH 30 minutes later
3. Measurement of serum Cortisol 30 to 60 minutes later
An increase of at least 18 to 20 mcg/dL is considered normal. No increase in serum cortisol indicates the presence of adrenocortical insufficiency.
Diagnosis of secondary adrenocortical insufficiency in its early stages requires the low-dose test. It is also used for the diagnosis of chronic partial pituitary ACTH deficiency. This test involves the administration of 1 mcg of cosyntropin (Cortrosyn) as an IV bolus. Normally, an increase in cortisol occurs in 20 minutes. In patients with adrenocortical insufficiency, there is no increase in the serum cortisol level.
Overview of Cushing’s Disease
Etiology and Pathophysiology
The cause of Cushing’s disease is adrenocortical excess. In the majority of patients, the increased adrenocortical function results from excessive corticotropin, leading to hyperplasia of the adrenal cortex. In a smaller percentage of patients, it is the result of a cortisol-secreting adrenal tumor, whether from too much corticotropin (ACTH) or a primary tumor of the adrenal gland. A malignant tumor of the adrenal gland can produce many corticosteroids, whereas the benign adrenal tumor only produces one corticosteroid that is secreted by the adrenal gland. Other, much less common causes are hyperplasia of the adrenal gland or ectopic production of ACTH by malignancies such as bronchogenic carcinoma (Smeltzer et al., 2010). Long-term treatment with pharmacological glucocorticoids leads to iatrogenic Cushing’s syndrome.
Clinical Manifestations
Patients with Cushing’s disease often present with classic signs and symptoms. These include obesity, with a heavy trunk and thin extremities; a fatty “buffalo hump” at the neck and supraclavicular region; and a moon-faced appearance. The skin becomes fragile and tears easily, and broad purple striae and bruises may develop. Wound healing may be impaired. The hair is thin. Women have virilization with the appearance of masculine traits such as increased facial hair, breast atrophy, enlarged clitoris, disrupted menses, and voice deepening. Libido is diminished or absent in men and women. Depression, weakness, and lassitude may also occur.
The excessive secretion of corticotropin leads to osteoporosis and fractures, which are caused by the increase in calcium reabsorption from the bone. Blood glucose levels are also increased, and glucose intolerance may occur as a result of increased hepatic gluconeogenesis and resistance to insulin. Peptic ulcers may develop because of increased secretion of gastric acid and pepsin.
Diagnosis
The diagnosis of Cushing’s disease requires an overnight dexamethasone suppression test. The patient takes dexamethasone, a synthetic glucocorticoid, 1 mg orally at 11 PM. He or she then has a serum Cortisol level drawn at 8 AM. A cortisol level of less than 5 mcg/dL indicates that the HPA axis is functioning normally. Cortisol levels are higher in patients with adrenal or ectopic tumors.
NCLEX Success
3. A women receives a diagnosis of Cushing’s disease. She has an excess of which of the following hormones?
A. luteinizing hormone
B. glucose
C. insulin
D. corticotropin
4. A man has a low level of adrenocorticotropic hormone and a high level of cortisol. What disease does he have?
A. Cushing’s disease
B. Addison’s disease
C. adrenal cortex hemorrhage
D. myocardial infarction
Drugs Used to Treat Addison’s Disease
The goal of treatment for Addison’s disease is to replace the adrenocorticoids to correct adrenal insufficiency. It is important to replace both the mineralocorticoid and adrenocorticoid. Lifetime hormone replacement is necessary. Table 43.1 summarizes the adrenocorticoid and mineralocorticoids administered for the treatment of adrenocortical insufficiency.
TABLE 43.1
Drugs Administered for Addison’s Disease
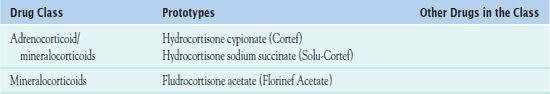
ADRENOCORTICOIDS/MINERALOCORTICOIDS
 Hydrocortisone cypionate (Cortef) or
Hydrocortisone cypionate (Cortef) or  hydrocortisone sodium succinate (Solu-Cortef) is a combination of a mineralocorticoid and adrenocorticoid. Both of these drugs are useful in acute and chronic adrenal insufficiency.
hydrocortisone sodium succinate (Solu-Cortef) is a combination of a mineralocorticoid and adrenocorticoid. Both of these drugs are useful in acute and chronic adrenal insufficiency.
Pharmacokinetics and Action
The oral preparation of hydrocortisone has a 1 to 2-hour onset of action, a peak of action in 1 to 2 hours, and a duration of action of 1 to 1.5 days. The parenteral preparation of the drug has an immediate onset of action, an unknown peak of action, and a duration of action of 1 to 1.5 days. Metabolism occurs in the liver. Excretion is in the kidneys.
Action
Hydrocortisone enters the cells and binds to the receptors in the cytoplasm to decrease inflammation; it suppresses the migration of polymorphonuclear lymphocytes and decreases capillary permeability. The mineralocorticoid in the drug increases the retention of sodium.
Use
Health care providers used hydrocortisone to replace adrenocorticoids and mineralocorticoids in patients with Addison’s disease. The drug is also useful in congenital adrenal hyperplasia. Table 43.2 gives route and dosage information for adrenocorticoids and mineralocorticoids.
 TABLE 43.2
TABLE 43.2
DRUGS AT A GLANCE: Adrenocorticoids/Mineralocorticoids and Mineralocorticoids
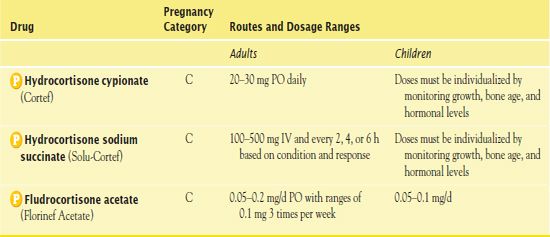
Use in Children
It is necessary to individualize the dose depending on the severity of the adrenal insufficiency and the response to the medication. The drug may affect growth velocity, and it is important to carefully assess growth and development with infants and children. Also, the nurse assesses neonate’s respiratory status closely after the administration of parenteral hydrocortisone. Some preparations contain benzyl alcohol, which may cause gasping syndrome in neonates.
Use in Older Adults
Elderly people should receive the lowest possible dosage because of the increased risk of adverse effects with systemic corticosteroids.
Adverse Effects
Hydrocortisone has significant adverse effects, including the following:
• Cardiac effects: fluctuations in blood pressure, shock, dysrhythmias, myocardial infarction, embolism, circulatory collapse, heart failure, and cardiac arrest
• Central nervous system (CNS) effects: vertigo, headache, and depression
• Dermatologic effects: fragile skin that tears easily, petechiae, ecchymoses
• Gastrointestinal (GI) effects: peptic or esophageal ulcers, pancreatitis, increased appetite, and weight gain
• Hematologic effects: sodium and fluid retention
• Metabolic effects: hyperglycemia and Cushing’s syndrome
• Musculoskeletal effects: osteoporosis and spontaneous fractures (long-term administration)
• Reproductive (female) effects: amenorrhea and irregular menses
• Other effects: immunosuppression, muscle weakness, impaired wound healing, and anaphylaxis
Contraindications
Contraindications to hydrocortisone include a known hypersensitivity to the drug or any component of the formulation as well as a serious infection. A BLACK BOX WARNING ♦ states that patients who are being treated with hydrocortisone should not receive live virus vaccines.
Nursing Implications
Preventing Interactions
Several medications and herbal supplements interact with hydrocortisone, increasing or decreasing its effects (Boxes 43.1 and 43.2). Hydrocortisone has numerous other interactions. Combination of hydrocortisone with certain drugs may result in the following effects:
• Salicylates: increased serum salicylate levels
• Acetylcholinesterase drugs: diminished therapeutic effect
• Anticoagulants: increased bleeding; it is necessary to monitor the ProTime and the International Normalized Ratio closely
• Food: interference with calcium absorption
• Alcohol: increased risk of gastric mucosal irritation and development of gastric ulcers
BOX 43.1  Drug Interactions: Hydrocortisone
Drug Interactions: Hydrocortisone
Drugs That Increase the Effects of Hydrocortisone
 Estrogen, hormonal contraceptives, ketoconazole, troleandomycin
Estrogen, hormonal contraceptives, ketoconazole, troleandomycin
Increase steroid blood levels
Drugs That Decrease the Effects of Hydrocortisone
 Cholestyramine, phenobarbital, phenytoin, rifampin
Cholestyramine, phenobarbital, phenytoin, rifampin
Decrease steroid blood levels



