Cultural and Pharmacogenetic Considerations
Bettyrae Jordan
Objectives
• Recognize verbal and nonverbal communication practices of various social and cultural groups.
• Explain appropriate spatial configurations for patients when delivering nursing care.
• Compare patients’ perception of time based on cultural constructs.
• Describe patients’ need to exercise control in their environment.
• Anticipate potential unique responses to drugs based on social, cultural, and biologic influences.
Key Terms
alternative health practices, p. 22
acculturation, p. 22
assimilation, p. 22
community, p. 22
complementary health practices, p. 22
culture, p. 22
cultural universals, p. 22
ethnopharmacology, p. 21
genomes, p. 24
healers, p. 22
pharmacogenetics, p. 21
pharmacogenomics, p. 24
polymorphisms, p. 24
traditional health practices, p. 22
Ethnopharmacology
Ethnopharmacology is the study of drug responses that may be unique to an individual owing to social, cultural, and biologic phenomena. The emergence of ethnopharmacology highlights the need for nurses to use knowledge and research from the social sciences as well as the biologic and physical sciences to provide holistic nursing care.
Pharmacogenetics integrates the study of pharmacokinetics, pharmacodynamics, and variations of the predicted response to a drug due to genetic factors. The nurse must integrate knowledge of pharmacogenetics within patients’ cultural contexts. Culture is defined as sets of learned behavior and ideas that human beings acquire as members of a community. A community is a cluster of individuals who function as a group to attain cultural universals. Cultural universals are designed to meet the community’s survival needs and common goals such as the obtainment of food and other practices that maintain the group. Providing culturally competent care complements the Quality and Safety Education for Nurses (QSEN) initiative (see Chapters 11 and 12 for more information on QSEN).
Transcultural Nursing
The concept of transcultural nursing was formalized by Madeleine Leininger, a nurse anthropologist. She founded the Transcultural Nursing Society in 1974. A challenge for nurses worldwide is the degree of cultural diversity owing to migration and global movement. Numerous cultural groups engage in the use of traditional health practices, which may include use of teas, herbs, spices, and special foods as well as homeopathic remedies, poultices, and ointments. These practices can have neutral, beneficial, or deleterious effects on a patient’s health. The nurse must obtain a thorough health history to determine all the pharmacotherapeutic agents the patient is using. Obtaining a thorough history is more difficult than it seems; patients may not reveal all information, assuming that because herbs, teas, and spices are natural substances, they are therefore not drugs. They may also be reluctant to share this information with a conventional health care practitioner.
Healers play a role in traditional health practices in about 80% of the population worldwide. Traditional healers usually have some practical knowledge of human anatomy and physiology, pharmacology, and pharmaceutical substances. Healers may combine practical knowledge with rituals that seek to control otherworldly forces such as deities or spirits. Every cultural group has its own traditions, superstitions, and belief systems. Throughout history, healing practices, religious ideology, and spirituality have been tightly intertwined.
Owing to varying degrees of assimilation and acculturation within and among cultural groups, it is essential for the nurse to not make generalizations about an individual’s beliefs or behaviors. Assimilation occurs when a less powerful group changes its ways to blend in with the dominant cultural group. Adults who immigrate to a new region usually take longer to assimilate than do younger people. Acculturation is the process by which a group adjusts to living within a dominant culture while at the same time maintaining its original identity. This sets the stage for complementary health practices that combine traditional beliefs and mainstream health practices.
Adding to the challenges faced by nurses in countries with numerous cultural groups is the phenomenon of the dominant group borrowing traditional health practices from other groups. When a dominant group adopts health practices from a nondominant group, they are called alternative health practices.
Use of complementary and alternative health practices is growing in the United States. A major impetus for this movement is that many individuals experience difficulty accessing or paying for mainstream health care. Even individuals who have access to mainstream health care may perceive that it is not personalized or effective, so they may opt for complementary health care (using a new therapy along with a mainstream therapy already in use) or alternative health care (using a new therapy in place of a mainstream therapy). This is evidenced by the vast amounts of teas and herbs available in most supermarkets (see Chapter 6) and by the increase in the use of acupuncture, acupressure, and massage as therapies.
The Giger and Davidhizar Transcultural Assessment Model
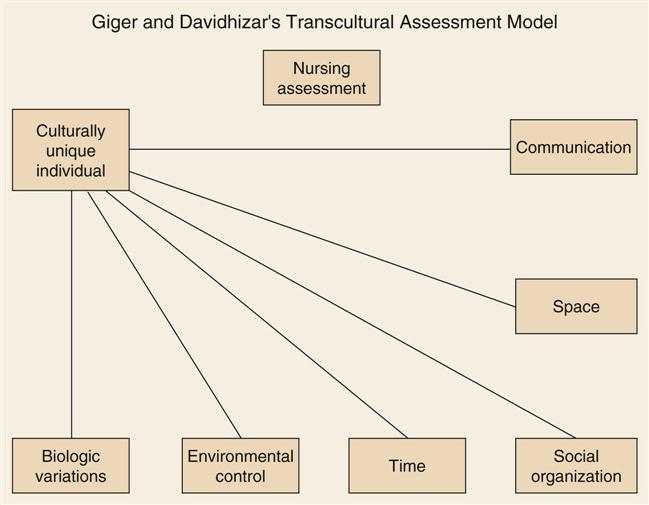
The Transcultural Assessment Model, developed by Giger and Davidhizar in 1998, suggests that all cultures have six cultural phenomena. These cultural phenomena flow from a culturally unique individual (Figure 3-1). The model has been frequently reviewed for relevancy and has been clinically useful for nurses and other members of the health care team.
Communication
Communication occurs verbally and nonverbally. Nurses must be alert to different types of communication styles among patients to provide culturally competent care.
Language
Patients’ use of languages other than English may pose a challenge to nurses working in the United States. Professional translators should be used whenever possible to safeguard a patient’s confidentiality. If a professional translator is not available, the nurse must select an alternative person carefully. (For example, asking the teenage son of a patient with gynecological health issues to translate may create an uncomfortable situation that is better avoided.) Even with the use of a translator, nuances in languages are unique and may not lend themselves to accurate translation in another language. There can be miscommunication between the patient, the translator, and the nurse.
Nurses should not confuse politeness with meaningful communication. Many patients will nod in agreement to statements made by the nurse even if the statements are not well understood because of language differences.
Vernacular English
Adding to the challenge of communication is the pervasive use of words and phrases that are popular in particular social or cultural groups. For example, the term “African-American Vernacular English” has been used to describe a style of English speaking that is used among some African Americans. It is thought to have its roots in the myriad of West African languages spoken by slaves brought to America. More generally, vernacular English is any style of English that varies from standard English. Its use by patients can lead to misunderstanding by the nurse or to other communication difficulties.
Greetings and Communication Styles
All cultures have prescribed norms for greeting and addressing others. Americans of European descent may be more informal when greeting and addressing others than descendants of non-European cultures. Nurses must keep in mind that patient-nurse interactions in health care settings are considered formal and that informal styles of communication should be used only after careful consideration.
For example, a communication style that might hinder culturally competent nursing care may be found in some patients of Asian descent, who might speak in a soft tone of voice and avoid direct eye contact. The nurse who is unaware of this may miss cues that care is needed. Asian Americans and Native Americans may be comfortable with periods of silence, while persons of Latin American, African, or European descent may be uneasy during periods of silence. Being cognizant of these preferences will help the nurse provide a comfortable environment for the patient.
Space
The amount of space around a person’s body is an important psychological consideration. Americans may desire a great deal of personal space. In some other cultures, population density may dictate limited personal space. Patients who are used to dense living quarters may feel insecure in a hospital room. It is important that the nurse have frequent contact with these patients and allow significant members of the social group to remain with the patient as much as possible.
A major challenge in caring for patients is the use of touch and the protection of modesty. Although nurses must touch patients to administer care, all cultures have taboos regarding touch. There are added considerations when the patient is of a different gender than the nurse. This is a particularly sensitive issue for groups within the Muslim, Orthodox Jewish, Amish, and Roma communities. For example, a Muslim woman may prefer to be cared for by a female nurse rather than a male nurse. Nurses should consider inquiring about patients’ preferences regarding touch before implementing nursing care. It may be best to have a family member of the same gender as the patient present during procedures, if possible. There may also be apparent paradoxes within cultures; for example, persons of Hispanic descent may value human contact but also value modesty.
Social Organization
Families are basic social units. The definition of family and the criteria for inclusion varies among individuals and among cultures. Americans of western European descent may have small, nuclear families, whereas other cultural groups living in the United States may have larger, extended families. Delivery of nursing care can be enhanced by including family whenever appropriate; nurses are in a position to advocate for inclusion of family in health care settings. Limiting the amount of time a patient can visit with members of the social group is a long-standing practice in American health care settings, but in some other countries, such as the Philippines, it is expected that family members will stay by the patient’s bedside and participate in his or her care.
Time
Nurses and their patients may have different perceptions of time. Time moves slowly for a patient who is anxious or in pain but moves quickly for a nurse who has a demanding workload. The use of vague terms to denote time may also cause a disparity between nurses’ and patients’ perceptions of time. Words like now, soon, or later may have vastly different nuances among individuals and groups.
Adding to the complexity of time perception are the concepts of linear time and circular time. When time is perceived as linear, the present flows into the future and is irretrievably lost. Viewing time as linear is likely to prompt thinking such as “I must do this now.” When time is perceived as circular, the present has more stability and the need to do things at the moment has less urgency. Viewing time as circular is likely to prompt thinking such as, “I will have the opportunity to do this later.”
The cultural aspect of time perception has a profound effect on pharmacotherapeutic adherence. All cultures have a concept of time as it is related to the past, present, and future. All humans are acutely aware that the present is here and now and in real time; it is the relative importance placed on the past, present, and future that directs the use of time.
People of western European descent may exhibit a great deal of future orientation. This can lead to health practices perceived to prevent illness, such as adhering to a low-fat diet to prevent higher cholesterol or wearing a condom during sex to prevent disease. Concern for the future also serves as motivation to take steps to control chronic illness, which is likely to lead to greater adherence to long-term pharmacotherapy. Explanations for these phenomena are that people of western European descent have historically experienced longevity and expect to have a lengthy future, and that their economic and social lives have revolved around calendars and clocks for centuries.
Non-European cultural groups such as those of African, Asian, Native American, or Latin American descent have exhibited less dependence on strict time schedules for economic and social activities. These groups’ perception of time may be rooted in agrarian cultures that use daily and seasonal rhythms of the earth and the sun to direct activities. This could result in emphasis being placed on the present; measures to ease the discomfort of a current illness may take precedence over measures to promote long-term wellness or treat a chronic illness. Patients with a present-oriented perception of time are more likely to discontinue mainstream prescriptive therapies when they feel well. It must be noted, however, that with the shrinking of agrarian cultures and the spreading of European-style practices, this treatment of time is changing. The nurse must therefore assess the patient’s degree of acculturation or assimilation.
Cultural groups that are steeped in traditional practices or perceive that their cultural identities are threatened are likely to have a past orientation of time, which may lead to the use of traditional health practices over mainstream health practices. Health behaviors of individuals are also influenced by the quantity and quality of past experiences with the health care system.
Environmental Control
A major aspect of culture is the desire to control nature to facilitate the needs of human beings. The concept of “nature” may include otherworldly forces or beings, such as deities and spirits. Illness may be attributed to cosmic forces and believed to be cured or ameliorated by persons who possess special abilities. Traditional healers are thought to have influence over otherworldly forces.
Healers and spiritual advisors can be beneficial in health care settings; examples include the practice of clergy (e.g., minister, priest, rabbi) visiting ill members of a congregation or the inclusion of a traditional healer in the plan of care.
The Indian Health Service is a federal agency within the U.S. Department of Health and Human Services that oversees the health care of approximately 2 million Native Americans who belong to federally recognized tribes. Similarly, the Canadian health care system has developed many initiatives to improve the health care of its indigenous peoples, known as First Nation, Inuit, and Metis. In both systems, the use of traditional healers and spiritual guides is incorporated into mainstream prescriptive therapies.
Biologic Variations
Through the work of the Human Genome Project, an international collaborative research program, the field of pharmacogenomics is rapidly expanding. In the United States, the project is managed by the National Human Genome Research Institute, which is part of the National Institutes of Health (NIH). Pharmacogenomics refers to the general study of all the different genes that determine drug behavior. An example of a significant finding of pharmacogenomics is the effect of the Cytochrome P-450 (CYP) enzymes on drug response, drug-drug interactions, and adverse drug events, which are described later in the chapter.
The Genographic Project has performed DNA testing on populations all over the world. Findings reveal that human beings are 99.9% genetically identical; this implies that there are not multiple races but multiple genotypes (an individual’s genetic identity).
To illustrate the significance of these findings to the patient care setting, it is necessary to review additional terms used in the fields of pharmacogenomics and pharmacogenetics. Genomes are a complete set of chromosomes and make up a cell’s DNA. Polymorphisms are DNA variants that occur within a specific population at a frequency greater than 1%. A substrate is a substance that binds to and is metabolized by one or more enzymes. Drugs are chemical substances and a type of substrate. The Cytochrome P-450 enzyme system either induces or inhibits the action of substrates. Induction or inhibition of a substrate accounts for the variations in drug metabolism in individuals and groups. The Division of Clinical Pharmacology at Indiana University Department of Medicine continually updates a clinically relevant table of drug interactions caused by the Cytochrome P-450 system.
Human migration around the world has been so vast over such a long period that most people have a variety of genetic markers. The study of pharmacogenetics can pave the way for pharmacotherapy that yields greater therapeutic benefits and causes fewer adverse reactions. The application of pharmacogenetics should be approached with caution. A person who is dark-skinned and appears to be of African descent is likely to have some European genetic markers.
Certain classifications of medications have different effects in individuals whose genetic markers are predominantly characteristic of a certain biologic group. For example, in the United States, Caucasian people are more likely than people of Asian or African heritage to have abnormally low levels of the CYP2D6 enzyme that metabolizes drugs belonging to a variety of therapeutic areas, such as antidepressants, antipsychotics, and beta blockers.
African Americans respond poorly to several classes of antihypertensive agents (beta blockers and angiotensin-converting enzyme inhibitors). Differences in skin structure and physiology can affect response to dermatologic and topically applied products. Clinical trials have demonstrated lower responses to interferon-alpha used in the treatment of hepatitis C among African Americans compared with other racial subgroups.
As another example, the U.S. Food and Drug Administration has entered into an agreement with the manufacturers of drugs containing carbamazepine (Tegretol) to include product labeling recommending that patients of Asian ancestry be genetically tested before starting on this agent. There is a strong association between serious skin reactions and an inherited variant of the H 1502LA-B gene found in Asians.
These intrinsic biologic factors must be considered along with extrinsic factors such as diet and environmental and sociocultural issues to prescribe effective therapies and provide holistic health care.
Researchers conducting clinical trials for development of new drugs are now required to obtain genetic testing of the participants in the study. Issues to be resolved before widespread testing are the cost-versus-benefit ratio and ethical considerations. Genetic testing is expensive and generally not covered by third-party payers. Genetic information can affect employment, insurability, and family relationships.
Table 3-1 applies the Giger and Davidhizar Transcultural Assessment model to four broad cultural categories of peoples of European descent, African descent, Latin and Native American descent, and Asian descent. It is important to keep in mind that there is no generic prototype for any of these categories. Italian Americans are likely to have different customs than German Americans. There may be a perception in the United States that most Asians are Chinese and most Hispanics are Mexican, but in fact there is great variation among these broad groups regarding geography of origin, language, customs, and spiritual systems. Another misperception in the United States is that people of African descent are from one country, but Africa comprises 54 countries over a large geographical area; language, customs, and spiritual systems vary extensively.
TABLE 3-1
SELECTED ETHNIC/CULTURAL GROUPS AND COMPONENTS OF THE GIGER AND DAVIDHIZAR TRANSCULTURAL ASSESSMENT MODEL*
| CULTURAL PHENOMENA | COMMUNICATION STYLES | SPATIAL PREFERENCES | SOCIAL ORGANIZATION | PERCEPTION OF TIME | ENVIRONMENTAL CONTROL | BIOLOGIC VARIATIONS |
| People of European descent | Prefer direct eye contact. Use moderate to loud vocal volume. Use many words to describe symptoms. Uncomfortable with periods of silence. | Prefer a large amount of personal space. Value privacy. Exhibit a low to moderate amount of touching among group members. | Small, nuclear families. Extended family members often live a far distance away. High degree of individualism. | High level of importance placed on the future. Expect that the present level of comfort be addressed. Little focus on the past. | Primarily believe that healthy behaviors prevent illness. Secondarily believe that illness is caused by cosmic forces. Believe in being united with a deity in the afterlife. | Poor metabolizers of antidepressants, antipsychotics, cardiovascular agents, and isoniazid (INH), which can lead to toxicity. |
| People of African descent | Prefer direct eye contact. Use moderate to loud vocal volume. Uncomfortable with periods of silence. | Comfortable with a smaller amount of personal space. Exhibit moderate amount of touching among group members. | Small, nuclear families in America but might classify nonrelated persons as family. Important to recognize these members of the social group. | High level of importance placed on the present. Connected with the past as evidenced by the use of home remedies passed through generations. Become more concerned with the future as longevity increases. | Spiritually oriented. Important to include clergy in care. Believe in being united with a deity in the afterlife. | May have diminished therapeutic effects from beta blockers, ACE inhibitors, and warfarin sodium (Coumadin). |
| People of Latin American descent and Native Americans | Not likely to make direct eye contact with persons perceived to be in authoritative positions. Varying degrees of comfort with silence. | Comfortable with a small amount of personal space. Latin Americans value touching. Native Americans use touch lightly. | Large, extended families. Important to include family members in care. | High level of importance placed on the present. Connected with the past as evidenced by the use of traditional healers. Become more concerned with the future as longevity increases. . | Spiritually oriented. Followers of Christian religions derive comfort from religious artifacts such as rosary beads. There may be multiple deities in indigenous religions. | Native Americans have a high incidence of lactose intolerance resulting in low-calcium diets. Also exhibit enhanced vasomotor responses to alcohol. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree