Comfort, Rest, and Sleep
Objectives
• Define the key terms and key abbreviations in this chapter.
• Explain why comfort, rest, and sleep are important.
• List the OBRA room requirements for comfort, rest, and sleep.
• Describe 4 types of pain and the factors affecting pain.
• Explain why pain is personal.
• List the signs and symptoms of pain.
• List the nursing measures that relieve pain.
• Explain the purposes of a back massage.
• Explain why meeting basic needs is important for rest.
• Identify when rest is needed.
• Explain how circadian rhythm affects sleep.
• Describe the stages of sleep.
• Know the sleep requirements for each age-group.
• Describe the factors affecting sleep.
• Describe the common sleep disorders.
• List the nursing measures that promote rest and sleep.
• Explain how dementia affects sleep.
• Perform the procedure described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| CMS | Centers for Medicare & Medicaid Services |
| NREM | No rapid eye movement |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| REM | Rapid eye movement |
Comfort, rest, and sleep are needed for well-being. The total person—the physical, emotional, social, and spiritual—is affected by comfort, rest, and sleep problems. Discomfort and pain can be physical or emotional. Whatever the cause, they affect rest, sleep, function, and quality of life.
Rest and sleep restore energy and well-being. Illness and injury increase the need for rest and sleep. The body needs more energy for healing, repair, and daily functions.
See Focus on Long-Term Care and Home Care: Comfort, Rest, and Sleep.
Comfort
Comfort is a state of well-being. The person has no physical or emotional pain. He or she is calm and at peace. Age, illness, and activity affect comfort. So do temperature, ventilation, noise, odors, and lighting. Such factors are controlled to the meet the person’s needs (Chapter 20).
See Focus on Communication: Comfort.
Pain
Pain or discomfort means to ache, hurt, or be sore. It is unpleasant. Comfort and discomfort are subjective (Chapter 8). That is, you cannot see, hear, touch, or smell pain or discomfort. You must rely on what the person says. Report complaints to the nurse for the nursing process.
Pain differs for each person. What hurts to one person may ache to another. What one person calls sore, another may call aching. If a person complains of pain or discomfort, the person has pain or discomfort. Believe the person.
Pain is a warning sign from the body. Often called the fifth vital sign (Chapter 29), it signals tissue damage. Pain often causes the person to seek health care.
See Focus on Communication: Pain.
Types of Pain
Doctors use the type of pain for diagnosing. Nurses use the type for the nursing process.
Factors Affecting Pain
A person may handle pain well one time and poorly the next time. Many factors affect reactions to pain.
Past Experience.
Past experiences help us learn what to do or expect. Whether it is going to school, driving, taking a test, shopping, having a baby, or caring for children, the past prepares us for like events at another time. We also learn from the experiences of others.
The severity of pain, its cause, how long it lasted, and if relief occurred all affect the current response to pain. Knowing what to expect can help or hinder the person’s response.
Some people have not had pain. When it occurs, pain can cause fear and anxiety. They can make pain worse.
Anxiety.
Anxiety relates to feelings of fear, dread, worry, and concern. The person is uneasy, tense, and feels troubled or threatened. Sensing danger, the person does not know what is wrong or why.
Pain and anxiety are related. Pain can cause anxiety. Anxiety worsens pain. Reducing anxiety helps lessen pain. For example, the nurse explains about pain after surgery and about pain-relief drugs. The person knows the cause of pain and what to expect. This helps lessen anxiety and therefore the amount of pain.
Rest and Sleep.
Rest and sleep restore energy and reduce body demands. The body repairs itself. Without needed rest and sleep, thinking and coping with daily life are affected. Pain seems worse. Rest and sleep needs increase with illness and injury.
Attention.
Thinking about pain makes it seem worse. Pain may be all that the person thinks about. Even mild pain can seem worse if it is the person’s main focus.
Pain often seems worse at night. Activity is less, music and TV are off, and it is quiet. There are no visitors. Others are asleep. When unable to sleep, the person has time to think about pain.
Personal and Family Duties.
Often pain is ignored when there are children to care for. Some people go to work with pain. Others deny pain, fearing a serious illness. Illness can interfere with a job, going to school, or caring for children, a partner, or ill parents.
The Value or Meaning of Pain.
To some people, pain is a sign of weakness. It may mean a serious illness with painful tests and treatments. Therefore pain is ignored or denied. Pain can bring pleasure. The pain of childbirth is an example.
For some persons, pain means not having to work or assume daily routines. Pain is used to avoid certain people or things. The pain is useful. Some people like to be doted on and pampered. The person values and wants the attention.
Support From Others.
Dealing with pain is often easier when family and friends offer comfort and support. The pain of childbirth is easier with support and encouragement from a loving father. A child bears pain better when comforted by a parent or family member. The use of touch by a valued person is comforting. Just being nearby also helps.
With no family or friends, some people deal with pain alone. Being alone can increase anxiety. The person has more time to think about the pain. Facing pain alone is hard, especially for children and older persons.
Culture.
Culture affects pain responses. In some cultures, the person in pain is stoic. To be stoic means to show no reaction to joy, sorrow, pleasure, or pain. Strong verbal and nonverbal pain reactions are seen in other cultures. See Caring About Culture: Pain Reactions.
Non-English-speaking persons may have problems describing pain in English. The agency must identify these persons. The agency uses interpreters to communicate with the person. All persons have the right to be comfortable and as pain-free as possible.
Illness.
Some diseases affect pain sensations. Central nervous system disorders are examples. The person may not feel pain. Or it may be severe. Pain signals illness or injury. If pain is not felt, the person does not know to seek health care. The person is at risk for undetected disease or injury.
Signs and Symptoms
You cannot see, hear, feel, or smell the person’s pain. Rely on what the person tells you. Promptly report any information you collect about pain. Write down what the person says. Use the person’s exact words to report and record. The nurse needs the following information.
• Onset and duration. When did the pain start? How long has it lasted?
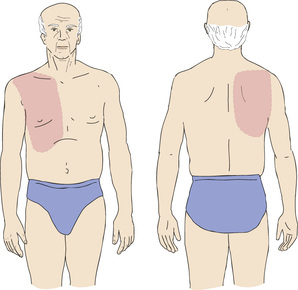
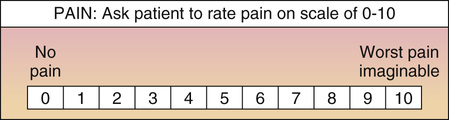
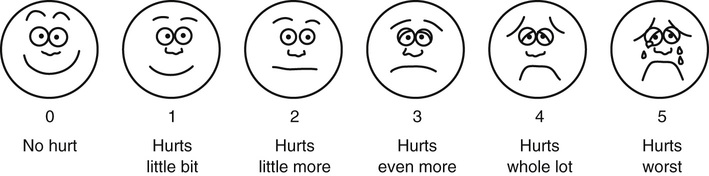
• Intensity. Does the person complain of mild, moderate, or severe pain? Ask the person to rate the pain on a scale of 0 to 10, with 10 as the most severe (Fig. 31-2). Or use the Wong-Baker FACES® Pain Rating Scale (Fig. 31-3). Designed for children, the scale is useful for all age-groups. To use the scale, tell the person that each face shows how a person feels. Read the description for each face. Then ask the person to choose the face best describing how he or she feels.
• Description. Ask the person to describe the pain. If necessary, offer some of the words listed in Box 31-1.
• Factors affecting pain. Ask what makes the pain better. Also ask what makes it worse.
• Vital signs. Measure pulse, respirations, and blood pressure (Chapter 29). Increases in these vital signs often occur with acute pain. Vital signs may be normal with chronic pain.
• Other signs and symptoms. Does the person have other symptoms—dizziness, nausea, vomiting, weakness, numbness or tingling, or others? Box 31-2 lists the signs and symptoms that often occur with pain.