Cholinergic Agonists and Anticholinergics
Objectives
• Compare the responses of cholinergic agonists and anticholinergic drugs.
• Differentiate between direct-acting and indirect-acting cholinergic agonists.
• Contrast the major side effects of cholinergic agonists and anticholinergics.
• Differentiate the uses of cholinergic agonists and anticholinergics.
• Apply the nursing process for the patient taking neostigmine, a reversible cholinesterase inhibitor.
Key Terms
acetylcholine, p. 268
anticholinergics, p. 272
anticholinesterases, p. 269
cholinergic blocking agents, p. 272
cholinergic agonists, p. 268
cholinesterase, p. 269
direct-acting cholinergic agonists, p. 269
indirect-acting cholinergic agonists, p. 270
miosis, p. 269
muscarinic receptors, p. 269
mydriasis, p. 272
nicotinic receptors, p. 269
parasympatholytics, p. 272
parasympathomimetics, p. 268
The two groups of drugs that affect the parasympathetic nervous system are the (1) cholinergic agonists (parasympathomimetics) and the (2) anticholinergics (parasympatholytics). The Unit V opener offers a discussion and comparison of the parasympathetic nervous system (parasympathomimetics and parasympatholytics) and the sympathetic nervous system.
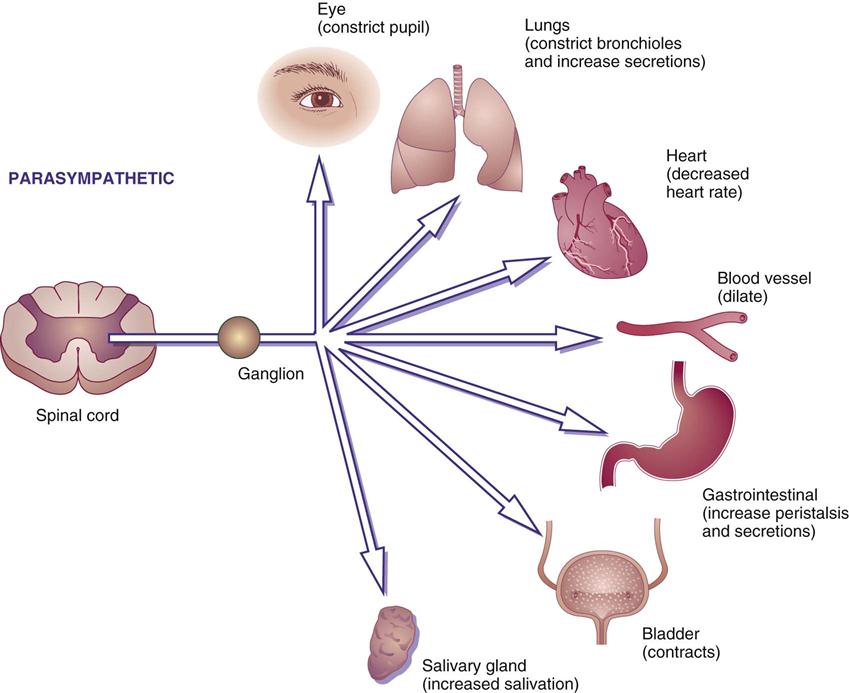
Cholinergic Agonists
Drugs that stimulate the parasympathetic nervous system are called cholinergic agonists, or parasympathomimetics, because they mimic the parasympathetic neurotransmitter acetylcholine. Cholinergic agonists are also called cholinomimetics or cholinergic stimulants. Acetylcholine (ACh) is the neurotransmitter located at the ganglions and the parasympathetic terminal nerve endings. It innervates cholinergic receptors in organs, tissues, and glands. The two types of cholinergic receptors are (1) muscarinic receptors, which stimulate smooth muscle and slow the heart rate; and (2) nicotinic receptors (neuromuscular), which affect the skeletal muscles. Many cholinergic agonists are nonselective because they can affect both the muscarinic and nicotinic receptors. However, there are selective cholinergic agonists for the muscarinic receptors that do not affect the nicotinic receptors. Figure 19-1 illustrates the effects of parasympathetic or cholinergic stimulation.
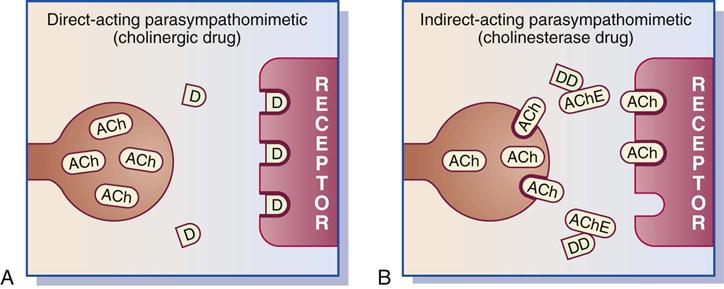
There are direct-acting cholinergic agonists and indirect-acting cholinergic agonists. Direct-acting cholinergic agonists act on receptors to activate a tissue response (Figure 19-2, A). Indirect-acting cholinergic agonists inhibit the action of the enzyme cholinesterase (ChE) (acetylcholinesterase) by forming a chemical complex, thus permitting acetylcholine to persist and attach to the receptor (Figure 19-2, B). Drugs that inhibit cholinesterase are called cholinesterase inhibitors, acetylcholinesterase (AChE) inhibitors, or anticholinesterases. Cholinesterase may destroy acetylcholine before it reaches the receptor or after it has attached to the site. By inhibiting or destroying the enzyme cholinesterase, more acetylcholine is available to stimulate the receptor and remain in contact with it longer.
Cholinesterase inhibitors (anticholinesterases) can be separated into reversible inhibitors and irreversible inhibitors. The reversible inhibitors bind the enzyme cholinesterase for several minutes to hours, and the irreversible inhibitors bind the enzyme permanently. The resulting effects vary with how long the cholinesterase is bound.
The major responses of cholinergic agonists are to stimulate bladder and gastrointestinal (GI) tone, constrict the pupils of the eyes (miosis), and increase neuromuscular transmission. Other effects of cholinergic agonists include decreased heart rate and blood pressure and increased salivary, GI, and bronchial glandular secretions. Table 19-1 lists the functions of direct- and indirect-acting cholinergic agonists.
TABLE 19-1
EFFECTS OF CHOLINERGIC AGONISTS
| BODY TISSUE | RESPONSE |
| Cardiovascular* | Decreases heart rate, lowers blood pressure because of vasodilation, and slows conduction of atrioventricular node. |
| Gastrointestinal† | Increases tone and motility of smooth muscle of stomach and intestine. Increases peristalsis and relaxes sphincter muscles. |
| Genitourinary | Contracts muscles of the urinary bladder, increases tone of ureters, and relaxes bladder’s sphincter muscles. Stimulates urination. |
| Ocular† | Increases pupillary constriction, or miosis (pupil becomes smaller) and increases accommodation (flattening or thickening of eye lens for distant or near vision). |
| Glandular* | Increases salivation, perspiration, and tears. |
| Bronchial (lung)* | Stimulates bronchial smooth muscle contraction and increases bronchial secretions. |
| Striated muscle† | Increases neuromuscular transmission and maintains muscle strength and tone. |
*Tissue responses to large doses of cholinergic agonists.
†Major tissue responses to normal doses of cholinergic agonists.
Direct-Acting Cholinergic Agonists
Many drugs classified as direct-acting cholinergic agonists are primarily selective to the muscarinic receptors but are nonspecific because the muscarinic receptors are located in the smooth muscle of the GI and genitourinary tracts, glands, and heart. Bethanechol chloride (Urecholine), a direct-acting cholinergic agonist, acts on the muscarinic (cholinergic) receptor and is used primarily to increase micturition (urination) in the treatment of urinary retention and neurogenic bladder. Metoclopramide HCl (Reglan) is a direct-acting cholinergic agonist that is usually prescribed to treat gastroesophageal reflux disease (GERD). Metoclopramide accelerates gastric emptying time. Prototype Drug Chart 19-1 details the pharmacologic behavior of bethanechol, which is a classic cholinergic agonist.
Pharmacokinetics
Bethanechol chloride (Urecholine) is poorly absorbed from the GI tract. The percentage of protein-binding and the half-life are unknown. The drug is most likely excreted in the urine.
Pharmacodynamics
The principal use of bethanechol is to promote micturition by stimulating the muscarinic cholinergic receptors in the detrusor muscle to contract the bladder and produce urine output. The patient voids approximately 30 minutes to 1.5 hours after taking an oral dose of bethanechol because of the increased tone of the detrusor muscle. Bethanechol also increases peristalsis in the GI tract. The drug should be taken on an empty stomach. It should not be administered by injection.
Side Effects and Adverse Reactions
Mild to severe side effects of most muscarinic agonists such as bethanechol include hypotension, bradycardia, blurred vision, excessive salivation, increased gastric acid secretion, abdominal cramps, diarrhea, bronchoconstriction, and, in some cases, cardiac dysrhythmias. This group of agents should be prescribed cautiously for patients with low blood pressure and heart rates. Muscarinic agonists are contraindicated for patients with intestinal or urinary tract obstruction, severe bradycardia, and for those with active asthma.
Direct-Acting Cholinergics: Eye
Pilocarpine is a direct-acting cholinergic agonist that constricts the pupils of the eyes, thus opening the canal of Schlemm to promote drainage of aqueous humor (fluid). This drug is used to treat glaucoma by relieving fluid (intraocular) pressure in the eye and to promote miosis in eye surgery and examinations. An oral form of pilocarpine is used to relieve xerostomia (dry mouth). Pilocarpine also acts on the nicotinic receptor, as does carbachol. Both agents are discussed in more detail in Chapter 49.
Indirect-Acting Cholinergic Agonists
The indirect-acting cholinergic agonists do not act on receptors; instead they inhibit or inactivate the enzyme cholinesterase, permitting acetylcholine to accumulate at the receptor sites (see Figure 19-2, B). This action gives them the name cholinesterase (ChE) inhibitors, acetylcholinesterase (AChE) inhibitors, or anticholinesterases, of which there are two types: reversible and irreversible.
The function of the enzyme cholinesterase is to break down into choline and acetic acid. A small amount of cholinesterase can break down a large amount of acetylcholine in a short period. A cholinesterase inhibitor drug binds with cholinesterase, allowing acetylcholine to activate the muscarinic and nicotinic cholinergic receptors. This action permits skeletal muscle stimulation, which increases the force of muscular contraction. Because of this action, cholinesterase inhibitors are useful to increase muscle tone for patients with myasthenia gravis (a neuromuscular disorder). By increasing acetylcholine, additional effects occur, such as increase in GI motility, bradycardia, miosis, bronchial constriction, and increased micturition.
The primary use of reversible cholinesterase inhibitors is to treat myasthenia gravis; another use is to treat Alzheimer’s disease. The primary clinical indication for irreversible cholinesterase inhibitors is glaucoma.
Reversible Cholinesterase Inhibitors
Reversible cholinesterase inhibitors are used (1) to produce pupillary constriction in the treatment of glaucoma and (2) to increase muscle strength in patients with myasthenia gravis. Drug effects persist for several hours. Drugs used to increase muscular strength in myasthenia gravis include neostigmine (Prostigmin [short-acting]), pyridostigmine bromide (Mestinon [moderate-acting]), ambenonium chloride (Mytelase [long-acting]), and edrophonium chloride (Tensilon [short-acting for diagnostic purposes]). These drugs are discussed in more detail in Chapter 24. A reversible anticholinesterase drug is physostigmine (Antilirium) or ophthalmic form (Isopto Eserine). Physostigmine is used as an antidote for atropine to reverse anticholinergic toxicity. Ophthalmic agents are further discussed in Chapter 49.
Side Effects
Caution for reversible cholinesterase inhibitors is required for patients who have bradycardia, asthma, peptic ulcers, or hyperthyroidism. Cholinesterase inhibitors are contraindicated for patients with intestinal or urinary obstruction.
Irreversible Cholinesterase Inhibitors
Irreversible cholinesterase inhibitors are potent agents because of their long-lasting effect. The enzyme cholinesterase must be regenerated before the drug effect diminishes—a process that may take days or weeks. These drugs are used to produce pupillary constriction.
Table 19-2 lists examples of cholinergic drugs and their standard dosages and common uses.
TABLE 19-2
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Direct-Acting Cholinergic Agonists | ||
| bethanechol Cl (Urecholine) | See Prototype Drug Chart 19-1. | |
| metoclopramide HCl (Reglan) | A: PO: 5-10 mg q8h PRN | For GERD, gastroparesis, and nausea. Central dopamine receptor antagonist. Increases gastric emptying time. Pregnancy category: B; PB: 30%;  : 2.5-6 h : 2.5-6 h |
| carbachol (Miostat) | Ophthalmic: 0.75%-3%, 1-2 gtt, 3 daily | To reduce IOP, miosis. See Chapter 49. |
| pilocarpine HCl (Pilocar) | Ophthalmic: 0.5%-4%, 1 gt | To reduce IOP, miosis. See Chapter 49. |
| Cholinesterase Inhibitor | ||
| donepezil HCl (Aricept); rivastigmine (Exelon) | See Chapter 23, Table 23-6. | |
| Indirect-Acting Cholinergics or Cholinesterase Inhibitors for the Eye | ||
| demecarium bromide (Humorsol) | 0.125%-0.25%, 1 gt q12-48h | To reduce IOP in glaucoma; long-acting miotic. See Chapter 49. |
| echothiophate iodide (Phospholine Iodide) | 0.03%-0.25%, 1 gt daily or b.i.d. | To reduce IOP; long-acting miotic. See Chapter 49. |
| isoflurophate (Floropryl) | 0.25%, ointment q8-72h | To treat glaucoma. Apply to the conjunctival sac. See Chapter 49. |
| Reversible Cholinesterase Inhibitors: Myasthenia Gravis | ||
| ambenonium Cl (Mytelase) | A: PO: 2.5-5 mg t.i.d./q.i.d.; dose may be increased; maint: 50-75 mg t.i.d./q.i.d. | To increase muscle strength in myasthenia gravis; long-acting. May be used with glucocorticoids. Pregnancy category: C; PB: UK;  : UK : UK |
| edrophonium Cl (Tensilon) | A: IV: 2 mg; then 8 mg if no response IM: 10 mg; may repeat with 2 mg in 30 min C: <34 kg: IV: 1 mg; repeat in 30-45 sec if no response; max: 5 mg C: >34 kg: IV: 2 mg; repeat with 1 mg if no response; max: 10 mg | To diagnose myasthenia gravis; very short-acting. Pregnancy category: C; PB: UK;  : 1.2-2 h : 1.2-2 h |
| neostigmine methylsulfate (Prostigmin) | A: 15 mg t.i.d.; gradually increase to maintenance dose of 150 mg; max: 375 mg/d A: IM/IV: 0.5-2.5 mg q1-3h; max: 10 mg/d C: IM/IV: 0.01-0.04 mg/kg q2-4h | To increase muscle strength in myasthenia gravis; short-acting. Used also to prevent or treat postoperative urinary retention. Pregnancy category: C; PB: 15%-25%;  : 1-1.5 h : 1-1.5 h |
| physostigmine salicylate (Antilirium); (Isopto Eserine Salicylate-ophthalmic form) | A: IV/IM: 0.5-2 mg/dose, repeat q10-30min PRN; C: IV: 0.02 mg/kg/dose, repeat q5-10 min PRN; max: 2 mg total A: 0.25% to 0.5%, 1-2 gtt daily or q.i.d.; max: 8 gtt/d | To reverse anticholinergic toxicity and to reduce IOP, miosis; short-acting. Pregnancy category: C; PB: UK;  : 15-40 min : 15-40 min |
| pyridostigmine bromide (Mestinon) | A: PO: 60-120 mg t.i.d./q.i.d.; maint: 600 mg/d in 3-4 divided doses; SR: 180-540 mg daily or b.i.d. IM/IV: 2 mg q2-3h C: PO: 7 mg/kg/d in 5-6 divided doses | To increase muscle strength in myasthenia gravis. Prevents destruction of the neurotransmitter acetylcholine. Pregnancy category: C; PB: 10%;  : 3-4 h : 3-4 h |
| Antidote for Irreversible and Reversible Cholinesterase Inhibitors | ||
| pralidoxime Cl (Protopam) | A: IV: 1-2 g in 100 mL of saline solution infused over 15-30 min; follow with 250 mg q5min PRN | To treat overdose of a cholinesterase inhibitor for myasthenia gravis and to treat overdose of organophosphate pesticides that cause muscle paralysis. Pregnancy category: C; PB: UK;  : 1-2.7 h : 1-2.7 h |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 : UK
: UK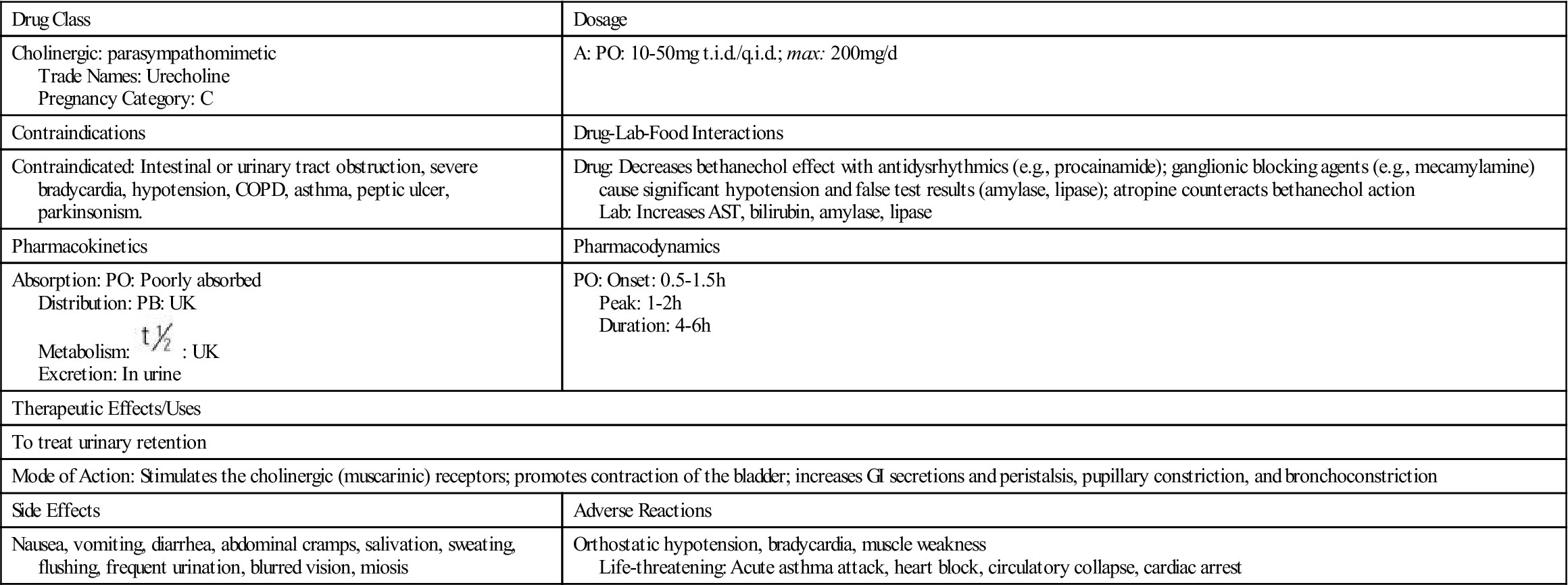
 , half-life; t.i.d., three times a day; UK, unknown.
, half-life; t.i.d., three times a day; UK, unknown.

























