Children in the Community
Anne Rath Rentfro and Michelle McGlynn
Focus Questions
What are common health care needs of children from birth through adolescence?
Who are the children “at risk” who require community/public health nursing interventions?
What is the impact of poverty on child health?
What community resources are available to promote the health of children?
Key Terms
Advocacy
Anticipatory guidance
Children’s Health Insurance Program (CHIP)
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program
Emancipated minor
Head Start
Hidden costs
High-technology home care
Home Start
Managed care programs
Medically fragile children
Normalization
Poverty
Primary prevention
Role modeling
Technology-dependent
Children in the united states
Children have unique needs and health concerns. Community/public health nurses whose practice includes families and children need to be aware of the special needs and health risks of children in the United States.
Demographics
There are almost 75 million children under the age of 18 in the United States, representing about one-fourth of the population (U. S. Census Bureau, 2010). Approximately 57% of American children are non-Hispanic white, 20% are Hispanic, 15% are African American, 4% are Asian/Pacific Islander, and 1% are American Indian/Alaska Native (Chau et al., 2010; U. S. Census Bureau, 2010).
The proportion of U.S. children under age 18 who lived in poverty in 2009 (20%) increased from 18% in 2007 (DeNavas-Walt et al., 2010). Although more non-Hispanic white children live in low-income families, their proportion (29%) is lower compared with other ethnic or racial groups. Minority groups are disproportionately affected by poverty, with over 60% of Hispanic (10.6 million), African American (6.6 million), and American Indian (0.3 million) children living in low-income families compared with about 30% of white (11 million) and Asian (1.1 million) children (Chau et al., 2010). Almost half (44%) of children from single-parent households live in poverty compared with only 11% of children from married couple–related families. For children under age 6 years in single-parent households, the poverty rate is 54% (DeNavas-Walt et al., 2010).
Impact of Poverty on Child Health
Low household income is consistently associated with poor health (see Chapter 21). Poverty (that is, inadequate food, clothing, and shelter) negatively affects children’s health and well-being in a number of ways (Brouse & Basch, 2010; Larson & Halfon, 2010). Death rates are higher among poor children, who are also more likely to be born prematurely or at low birth weight (Abdullah et al., 2010; Anum et al., 2010; Holzman et al., 2009; Yoder et al., 2010). Depression and conduct disorders occur more often, and violence is commonly encountered within the context of poverty. Chronic health problems, obesity, injuries, adolescent pregnancy, substance abuse, school failure, and school dropout appear in children who live below the poverty level (Abdullah et al., 2010; Leatherman & Dunford, 2010; Wells et al., 2010). Obesity and sedentary behavior are more likely to occur in poor children as well as stress and adverse health outcomes such as compromised immune systems (Cochran, 2008; Nilsen, 2007; Wells et al., 2010).
Poor families survive by using crisis-oriented rather than preventive approaches to health. Social determinants—such as unavailable transportation, lack of health insurance, minimum wage employment, cultural and linguistic differences, stigma, undocumented status, neighborhood conditions, housing, inaccessible resources, or lengthy eligibility processes—may produce barriers to health care services and complicate health care delivery (Brouse & Basch, 2010; Hernandez et al., 2010; Jacobi et al., 2011). O’Connor (2011) described how nurses can improve healthcare equity using the International Nurses’ Day kit to alleviate health care disparities. In the United States, eligible families may receive services from sources such as Temporary Assistance to Needy Families (TANF) (U.S. Department of Health and Human Services [USDHHS], 2008) and Medicaid (USDHHS, 2011a). Medicaid along with the Children’s Health Insurance Program (CHIP) provides health services for low to moderate income children. However, over 70% of uninsured children live in poverty (Kaiser Family Foundation [KFF], 2011a). Eight million children lack health insurance and most of them live in employed families (KFF, 2011a). Economic downturn has contributed to employer- sponsored insurance program decreases; however, legislative incentives have contributed to increases in CHIP enrollment. Although the number of uninsured children has decreased in the United States since 2007, employer-sponsored insurance is likely to continue to decline, predominantly affecting the young adult population and, in turn, children (Holahan, 2011).
Legal Parameters Guiding the Care of Children
Because children are minors, parents or guardians make legal decisions for them. Guardians act as protectors and should advocate for the child’s best interests. Faced with multiple family constellations and potential health care situations, the legal system in most states clarifies who makes decisions for the child and determines a child’s legal age (see Chapter 6). General policies, often set by state legislation, categorize and label children based on preset criteria, which are often based solely on age rather than decisional capacity (Chenneville et al., 2010). For example, legislation determines that children enter public school based on age rather than developmental readiness for school. One example where policy is not strictly aligned with age alone is that of emancipated minors. Emancipated minors are adolescents who are legally underage, but recognized legally as adults under circumstances prescribed by state law. Situations resulting in emancipation vary from state to state but usually include pregnant female adolescents, high school graduates, married adolescents, military personnel, or adolescents living independently from their parents or guardians. Some minors may consent to certain medical and surgical procedures without notifying their parents or guardians. The types of consensual services vary but generally include treatment for sexually transmitted diseases (STDs), counseling about human immunodeficiency virus (HIV), contraceptive services, services for pregnancy, treatment for drug and alcohol problems, outpatient mental health counseling, and services for emergency situations (Chenneville et al., 2010).
Regardless of emancipation status, nurses can advocate to encourage children’s participation in decision making in their own health care. Health care providers and parents frequently make decisions for younger children. Community health nurses should, when possible, give children opportunities to express opinions about decisions that affect them. In addition, in the United States, a child whose parents refuse lifesaving measures for that child based on religious practices has the legal right to petition the court (Ganjoo et al., 2011). Nurses often present information about options to families; therefore, knowledge about broadened options available to these families for adequate decision making is essential. For example, families may be unaware that some isolated protein preparations may be acceptable alternatives for people who have religious restrictions to transfusion (Ganjoo et al., 2011).
Community health nurses participate in the legal aspects of children’s health in cases of child abuse or neglect (see Chapter 23). Nurses encounter these issues with minors during the consent process for sensitive services, such as STD treatment, family planning, or abortion services, or when parents or guardians refuse needed care for their child (see Chapter 6). Nurses who know local laws and maintain a relationship with child protective services, act as advocates for children in the community.
History of Community Health Care for Children
Since the 1880s, community health nurses have assisted new mothers to care for their newborn children. This important role decreases high infant death rates and child neglect (Bhutta et al., 2005; Walker & Chesnut, 2010). Evidence-based instruments such as the Optimality Index and automated informatics systems such as the Omaha System indicate that public health nursing, including prenatal and postnatal home visits, continues to provide positive outcomes (Maher et al., 2011; Monsen et al., 2010).
At the beginning of the twentieth century, infection killed many children. Sick children remained at home for care. Community health nurses played a vital role in infection control through home risk assessment, family education about infection control, and care of the sick. Nurses monitored quarantined families; still many children died due to lack of sophisticated medical technology. By the middle of the century, the focus of community health nurses expanded to include population-focused care with education about the growth and development of children which is consistent with current public health nursing competencies and standards of practice (Weierbach, 2007).
Before World War II, support services for children with significant disabilities were minimal. Families either institutionalized those children with disabilities or cared for them at home without external resources. In 1935, Title V of the Social Security Act authorized the Crippled Children’s Services (CCS) programs, later renamed the Title V Children with Special Health Care Needs (CSHCN) programs. This program provided federal and state funds for infrastructure and direct care of children with special needs. Program enhancements in 1989 included a focus on development of family-centered, community-based, and coordinated systems of care for special needs children. By the late 1950s, immunization programs prevented many communicable diseases, shifting emphasis to students with special needs and special school placements. Educational rights and services for children with disabilities changed dramatically with the 1975 enactment of Public Law (PL) 94-142, Education for All Handicapped Children Act. This law guaranteed free and appropriate education for all children with disabilities ages 6 through 21 years in the least restrictive environment. Subsequent amendments (PL 99-457 and PL 102-119) expanded eligibility to all children with disabilities from birth through age 21 years (University of North Carolina Chapel Hill, 2010).
Currently, technology has resulted in an entirely new population of children for community health nurses (Hewitt-Taylor, 2010). The number of children surviving the perinatal period with significant impairment has grown rapidly with a corresponding rise in programs to maximize human potential and minimize economic costs associated with disability (Smith & Dragoo, 2010). Technology-dependent or medically fragile children now challenge health care. Community health nurses provide optimal care in the home, while promoting normal growth and development for these children in schools and communities (Darvill et al., 2009).
In general, community health nurses’ goals have changed minimally from those of 100 years ago. Goals continue to emphasize health promotion, disease prevention, and risk reduction for the child, the family, and the community. Techniques used and resources available to reach contemporary goals, however, are diverse and vary from one state to another. Nursing responsibilities in the community continue to focus on assessing the child in the family environment and planning interventions using appropriate resources.
Financing Health Care for Children
Access to health care is directly related to a family’s ability to pay for that care (see Chapters 3 and 4). Children’s health care in the United States may be financed by private payment, private insurance, Medicaid, the Children’s Health Insurance Program (CHIP), state Title V CSHCN programs, or other sources, such as nonprofit organizations providing care to low-income families. The Children’s Health Insurance Reauthorization Act of 2009 (CHIPRA) along with national health reform stimulated and simplified enrollment resulting in an increase of 4.5% in insured children in most states. This increased enrollment was attributed to outreach initiatives and national economic decline driving families to use public programs. For example, Texas experienced a large increase after initiating outreach efforts that included telethons, special enrollment dates, use of mass media and implementation of an online application, renewal, and premium payment system. Montana also experienced large growth in 2009. Clearly, offering simple clear access, reducing barriers, and expanding eligibility requirements reduces the number of uninsured children (KFF, 2011b).
Many children receive care through their parents’ employer-provided health insurance plans. Employers continue to increase employees’ share of premium costs and many limit health coverage solely to their employees, excluding families. For these families, cost of health insurance coverage becomes prohibitive (see Chapters 4 and 21). Employer-provided health insurance for most families consists of managed care programs, with limitations on choices and providers. Managed care provides opportunities for better coordination of care but may limit access to specialty care providers and hinder provider–client relationships.
For those who cannot afford health care, federal service falls into two categories, grants or Medicaid. Grants encourage the availability of specific health care services to specific populations, for example, maternal and child health care services, immunization programs, community and migrant farm worker health centers, and physician services in underserved locations. Medicaid is federal- and state-funded and provides health care for the poor. Health reform is likely to shift usage patterns and affect federal programming (Hall, 2011).
Many children from poor families receive care funded through the Medicaid program (Title XIX of the Social Security Act) (see Chapter 4). States administer the program, choosing to pay for services in various ways, most frequently through managed care plans or on a fee-for-service basis. Medicaid enrollment experienced a sevenfold increase between 2009 and June 2010, accompanied by a national recession and a doubling of the nation’s unemployment rate (Kaiser Commission, 2011).
An important component of the Medicaid program for children is the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program. It is a separately mandated program serving children from birth to age 21 years. As with Medicaid, it funds, but does not provide, direct services. The goal of EPSDT is to ensure that all children enrolled in Medicaid receive a basic set of comprehensive services to promote health and identify and treat problems at early stages. EPSDT services follow a prescribed schedule and include well-child care; immunizations; laboratory studies; anticipatory guidance; mental health, vision, dental, and hearing screenings; tobacco avoidance information; and treatment for any identified conditions. The Patient Protection and Affordable Act of 2010 provides new opportunities to support EPSDT and similar programs to support children in the community (Hanlon, 2010).
The CHIP program allows states to provide health insurance to children whose families are above the financial eligibility for Medicaid, either through expansion of the Medicaid program or development of a new children’s health insurance program (KFF, 2011a). States retain significant flexibility in establishing eligibility, subsidies, payment rates, and use of health plans, although the federal Health Care Financing Administration (HCFA) must approve each state’s plan. The benefit package offered by the state must be at least equal to the level of typical commercial health insurance and includes preventive, primary, specialty, dental, and vision care.
With the authorization of the Title V of the Social Security Act, state CSHCN programs provide care to eligible children with severe or chronic illnesses. States may set up specialty care networks and clinics or contract with providers to pay for care on a fee-for-service basis (USDHHS, 2011b).
In addition to public and private sources of health insurance, community-based, nonprofit agencies and clinics provide care to children and families who have no other source of payment. These include community and migrant health care centers, charitable care programs, Indian Health Services, and others. Community health nurses must become familiar with all potential sources of low-cost health care within their communities (Hanlon, 2010).
Families and communities with children
Children and Their Family Constellations
Children live in almost every conceivable form of family constellation (see Chapter 12). Although most children’s families are what would be considered the nuclear family, which consists of the husband, the wife, and their children (adopted or natural), many experience an alternative family environment at some point during their childhood with fewer children living with married parents than in years past. Grandparents play a vital role in many homes. As the numbers of divorces and remarriages increase, the number of children in blended families and reconstituted families with stepparents, stepsiblings, and extra sets of grandparents also increases. Family constellations are currently more diverse than any other time in history and affect children’s socialization within their communities (Grusec & Hastings, 2007).
In 2009, approximately 67% of the 113 million households in the United States claimed to be family households. Almost one-third of U.S. households have children (age < 18 years) who are generally living with two parents; however, 21% live with only their mothers, and 8% live with only their fathers. Marked differences exist across racial lines, with more white children living in two-parent homes compared with African American or Hispanic American children (U. S. Census Bureau, 2010).
Extended families, which include the nuclear family along with blood relatives or those related through marriage, are an important consideration in planning nursing care (Kelly et al., 2010; Ward & Hisley, 2009). Extended families may change the dynamics of nurses’ interactions with children. For example, the teenage mother frequently lives with her mother, who may help care for the baby. Both caregivers should be included in well-baby care counseling. New teen mothers and more experienced grandmothers may differ in their learning needs. Some children live in multiple “families” that share common ownership of property and goods (communal families), and others are raised by same-gender couples (nontraditional families) (Neville & Henrickson, 2009).
Families with foster-care and homeless children require extensive community resources and support (Todres, 2010). Community health nurses locate, facilitate access, and coordinate care for these children and their families. Homeless children and those in foster care typically have significant health care needs and are likely to be eligible for Medicaid and other community services which may become more available as health reform evolves (Todres, 2010). Nurses act as advocates, seeking appropriate community sources and coordinating care among multiple agencies including those related to unemployment and mental health (Dragon, 2011).
Developmental Tasks of Families
Developmental tasks contribute to overall health in childhood. Children must accomplish physical, cognitive, and psychosocial tasks to progress toward maturity (Table 27-1). For example, sitting alone, walking, learning concepts of time and numbers, and development of trust and sense of self are tasks required for this progression. Families work to master a set of developmental tasks, as well. Developmental tasks of families involve interaction among family members rather than developmental tasks of the individual child and aim to strengthen family units (Hockenberry & Wilson, 2010). Family developmental stages include aspects of physical requirements, cultural practices, and development of the family’s values and aspirations (see Unit Three, Family as Client).
Table 27-1
Developmental Tasks for Infants and Children (Includes Physical, Psychosocial, and Cognitive)
| Age | Task | |
| Infancy | 3 months | Decrease in primitive reflexes except protective and postural reflexes |
| Social smile (indicates development of memory traces) | ||
| 4 months | Laugh | |
| 5 months | Birth weight doubles | |
| When prone, can push up on arms | ||
| Rolls over | ||
| 6 months | Teething begins | |
| Sits with support | ||
| Exhibits “stranger anxiety” (is wary of strangers and clings to mother) | ||
| 8 months | Sits alone | |
| Crawls | ||
| 9 months | Pincer grasp | |
| Holds own bottle | ||
| 10 months | Stands with support | |
| 12 months | Birth weight triples | |
| Takes first steps alone | ||
| Develops trust | ||
| Speaks five words | ||
| Claps hands, waves bye-bye | ||
| Toddlerhood | 13 months–2.5 years | Masters walking |
| Climbs stairs | ||
| Feeds self (autonomy) | ||
| Language (increases to 400 words and 2- to 3-word phrases) | ||
| Toilet training and bowel and bladder control | ||
| Separation anxiety (screams when the mother leaves) | ||
| School age | 2.5–4 years | Increased vocabulary, uses sentences |
| Alternates feet on steps | ||
| Copies circles and lines | ||
| Builds a tower of blocks | ||
| Concepts of causality, time, and numbers begin | ||
| Body image develops | ||
| Role plays | ||
| Enculturation begins | ||
| Development of conscience begins | ||
| Fears loss of body integrity | ||
| 5–12 years | Vision matures by age 6 years | |
| First baby tooth is lost at age 6 years; all permanent teeth except final molars are in by age 12 years | ||
| Develops peer relationships | ||
| Enjoy activities, groups, and teams | ||
| Morality develops | ||
| Cognitive development: concepts of time and space, reversibility, conservation, parts and whole | ||
| Can classify objects in more than one way | ||
| Reading and spelling and math concepts develop | ||
| Puberty begins: age 9 years for girls; age 11 years for boys | ||
| Sense of industry | ||
| Adolescence | 13–19 years | Secondary sex characteristics develop |
| Attains adult growth | ||
| Adjusts to body changes | ||
| Menses begin | ||
| Abstract thought develops | ||
| Develops an identity | ||
| Fantasizes role in different situations | ||
| Increased sexual interests | ||
| Increased peer influences |
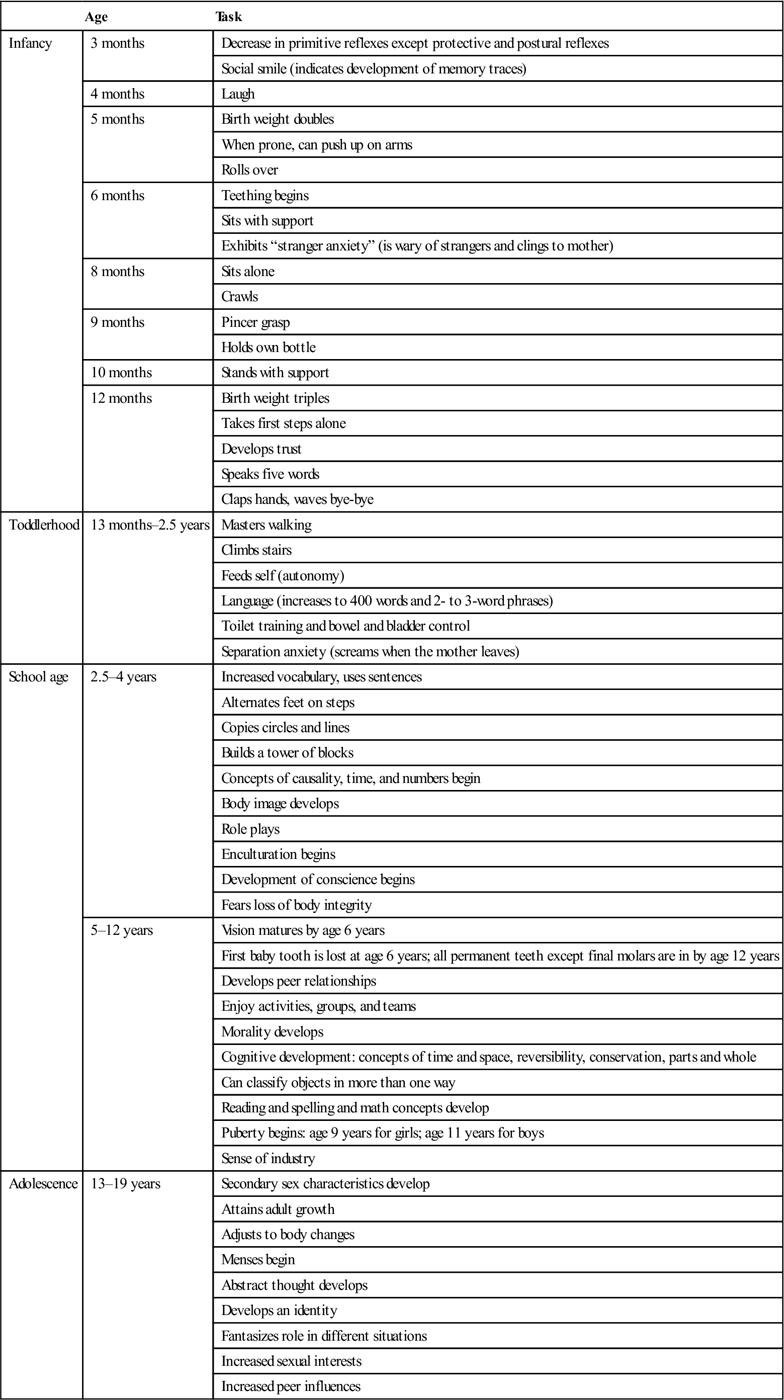
Compiled from: Hockenberry, M. J., & Wilson, D. (2010). Wong’s nursing care of infants and children (9th ed.). St. Louis: Mosby.
Duvall’s eight stages for families based on age and school placement of the oldest child are generally accepted as the foundation for family development theory. Four stages affect families with children younger than 18 years of age: stages II through V. These stages include families with infants and toddlers (stage II), preschoolers (stage III), school-aged children (stage IV), and adolescents (stage V). Critics of this model note that these stages were developed for two-parent families and are neither appropriate nor accurate for other family constellations, for families who have a child with a chronic condition, or for some cultural groups (see Chapter 10). Contemporary family structures extend well beyond the nuclear family. Many children live within a blended family structure or some structure other than the nuclear family with their own two parents (Neville & Henrickson, 2009; U. S. Census Bureau, 2010). Single-parent, grandparent, and same-gender parent arrangements occur more commonly now than ever before. Values of affection and moral responsibility, rather than biology alone, bond contemporary families (Ward & Hisley, 2009).
Developmental tasks for the early childbearing family (stage II) include the development of parenting skills, new communication patterns, and tasks related to time and energy management. Parents and grandparents adjust to their new roles, and the infant is integrated into the family unit (Hockenberry & Wilson, 2010).
Families often decide about the size of their family while their first child is at the preschool age. Preschool can have separation issues for both parent and child. Children commonly experience illnesses that require alternative care arrangements for working parents. Family stresses may stem from these and other issues. At this stage, children identify with same-gender parents; therefore, seeking caregivers of the child’s same gender is ideal.
Parents of school-age children adjust to influences of a third party (the school) and must adapt to the impact of the child’s peers and teachers. During this stage child’s tasks center on school achievement, while parents continue to develop satisfying marital relationships. Adolescents deal with increasing autonomy and independence, while parents return to their own marital and career issues along with concern for the older generation (Hockenberry & Wilson, 2010). Adolescents’ psychosocial developmental tasks may conflict with family developmental tasks. For example, the adolescents’ psychosocial task to seek role identity conflicts with the parental family task to take responsibility for children needs. With the many types of family constellations experienced by children in the community, strict adherence to a nuclear family developmental framework offers a flawed approach to family assessment.
Community health nursing is family health nursing. Nurses facilitate communication among family members and support endeavors to meet family and individual needs. Parenting is a learned not an innate skill and each developmental stage raises new concerns for parents. As parents learn to address these issues, they grow along with their children.
Cultural/Ethnic Influences on Health Care
Community health care nurses aim to provide culturally competent care in a global health environment with increasing population diversity (see Chapter 10). Home and community care must be appropriate and acceptable to the culture to be successful (see the Ethics in Practice box).
Child-rearing traditions vary. Breast-feeding, introducing solids, and toileting customs have cultural influences (Hockenberry & Wilson, 2010). Knowing child care cultural practices and identifying key family decision makers help nurses plan interventions that incorporate all persons responsible for childcare. Chapter 10 includes a broader discussion of the influences of culture. Expected behavior of children varies from one culture to another (Barnett et al., 2010). Community health nurses plan care based on communities’ attitudes toward children and their culturally accepted age-expected behaviors.
Common health needs of children
Health Promotion and Disease Prevention
Private health insurance and governmental funding agencies give priority to individual treatment and preexisting conditions and are not likely to have a family-oriented focus on health promotion and disease prevention. As health care reform initiatives continue, greater emphasis on health promotion and disease prevention may evolve. Community health nurses could provide the leadership necessary to promote health and prevent diseases among families. Nurses can contribute to empirical research to evaluate cost savings evidenced by prevention measures and early interventions that decrease morbidity and mortality. When these efforts produce cost savings, health care insurers and managed care organizations are more likely to permit these preventive measures as standard protocol.
Screening, education, counseling, and anticipatory guidance facilitate health maintenance, health promotion, and wellness. Families with newborn infants have numerous health-promotion and primary prevention needs such as well-child care (e.g., bathing, feeding, holding, diapering) and interpretation of an infant’s communication cues. In addition, parents are learning to adjust to their new roles (Edelman & Mandle, 2010; Hockenberry & Wilson, 2010). Parents need information about normal growth and development and the promotion of physical, psychosocial, and cognitive development throughout childhood. Knowing age-appropriate developmental tasks, implementing age-appropriate stimulation (Table 27-2), and managing common childhood physical health problems (Table 27-3) help parents cope with the changes that occur. Community health nurses also help families recognize the importance of preventive health care (immunizations and well-child care checkups) for health maintenance and early problem identification.
Table 27-2
Age-Appropriate Play Activities
| Infancy—Interaction primarily between caregiver and baby | |
| Rocking, cuddling, touching, massaging, singing, talking to infant: hanging brightly colored objects; looking in mirror; “people watching” Music, floor time with toys in reach | |
• 4 months | “Busy box” on the side of the crib or a “cradle gym” across the top to encourage reaching out |
• 6 months | Toys, plastic cups, pot lids, spoons, clutch ball, squeaky toys, water and water play (always supervised) |
• 9 months | Teething toys, toys that make noise when moved, boxes, large books, toys that can be pushed when crawling |
| Blocks, stacking cups, baby-safe cars, dolls, books, singing, cuddling, reading | |
| Toddler—Observes others at play but little cooperative play yet | Filling and dumping containers, stacking blocks, reading, singing, toys that can be carried, pushed, thrown, or dropped or can aid in walking |
| Preschool—Play becomes more interactive | Gross motor activities like riding a tricycle, playing ball, painting, stringing beads, arts and crafts, guessing games, puzzles, reading, fantasy play |
| School age—Play is a social experience | Collections, games, group activities, bikes, skates, sports, reading |
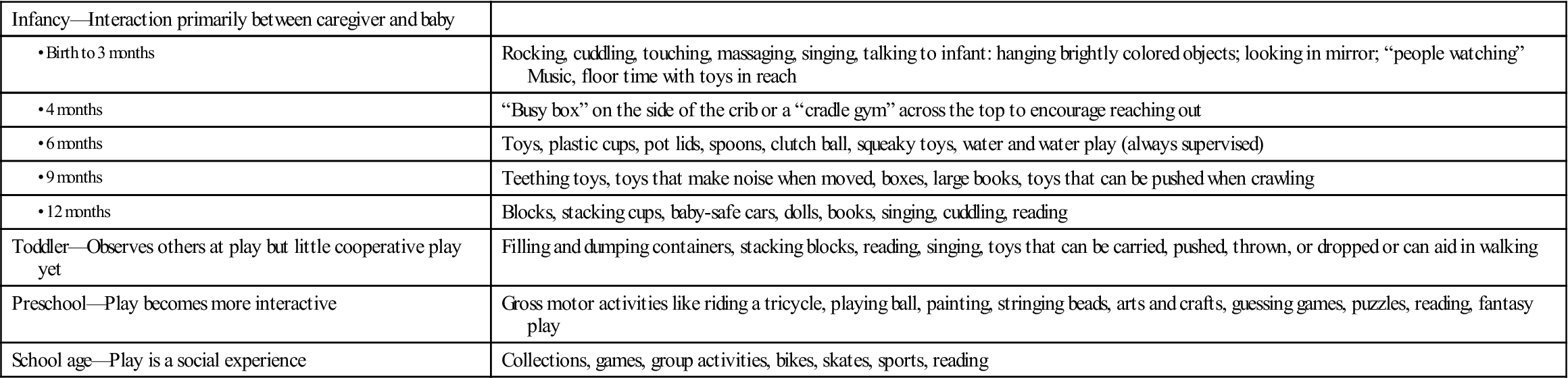
Compiled from: Hockenberry, M. J., & Wilson, D. (2010). Wong’s nursing care of infants and children (9th ed.). St. Louis, Missouri: Mosby
Table 27-3
Common Health Problems in Young Children
| Problem | Comments | Interventions |
| Teething | Begins around age 6 months when lower central incisors arrive Molars arrive during toddlerhood Caries develop mostly during preschool and school age | |
| Bottle mouth syndrome | Results from sleeping with juice-filled or milk-filled bottle and having long-term contact between the nipple and the teeth | |
| Toddler does not begin to speak | ||
| Iron deficiency anemia | Child’s iron supply from birth is depleted by age 4 to 6 months | |
| Temper tantrums | Common and normal during toddlerhood | |
| Streptococcal pharyngitis | ||
| Urinary tract infections | May be related to poor hygiene, fecal contamination, or sexual abuse | |
| Diaper rash | ||
| Constipation | Defined as hard consistency to the stools; not related to straining or grunting during defecation | 1. Increase liquids in the diet. 2. Add karo syrup (1 tsp to 3 oz of formula or milk). 5. Use a bulb syringe to remove nasal mucus. Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
