Central Nervous System Stimulants
Objectives
• Explain the effects of stimulants on the central nervous system (CNS).
• Compare attention deficit/hyperactivity disorder and narcolepsy.
• Differentiate the action of drugs used for attention deficit/hyperactivity disorder and narcolepsy.
• Contrast the common side effects of amphetamines, anorexiants, analeptics, doxapram, and caffeine.
• Compare the pharmacology of drugs used in the treatment of migraine headaches.
• Apply the nursing process for the patient taking CNS stimulants.
• Apply the nursing process for the patient taking doxapram (Dopram).
Key Terms
amphetamines, p. 285
analeptics, p. 288
anorexiants, p. 288
attention deficit/hyperactivity disorder, p. 285
central nervous system, p. 284
cluster headaches, p. 285
dependence, p. 284
migraine headaches, p. 285
narcolepsy, p. 285
neurotransmitters, p. 285
tolerance, p. 284
Numerous drugs can stimulate the central nervous system (CNS), which involves the brain and spinal cord that regulates body functions. Medically approved use of CNS stimulants is limited to the treatment of attention deficit/hyperactivity disorder (ADHD) in children, narcolepsy, and the reversal of respiratory distress. The major group of CNS stimulants includes amphetamines and caffeine, which stimulate the cerebral cortex of the brain; analeptics and caffeine, which act on the brainstem and medulla to stimulate respiration; and anorexiants such as diethylpropion, which are thought to suppress appetite by stimulating the satiety center in the hypothalamic and limbic areas of the brain. Amphetamines and related anorexiants are greatly abused. Long-term use of amphetamines can produce psychological dependence or tolerance, a condition in which larger and larger doses of a drug are needed to reproduce the initial response. These medications are recommended for short-term use only (up to 12 weeks). Gradually increasing a drug dose and then abruptly stopping the drug may result in depression and withdrawal symptoms.
Drugs used to treat migraine and cluster headaches include analgesics, ergot alkaloids, and selective serotonin1 receptor agonists (triptans). Migraine headaches generally cause severe throbbing pain. They are often preceded by an aura (visual, smells, tingling, vertigo warning). The cause is not definitive but is thought to be due to changes in the brainstem, which activates the trigeminal nerve. Low serotonin levels may also be involved by triggering the trigeminal system to release neuropeptides, which cause pain. Triggering factors for migraines include certain foods (beer, red wine, aged cheese, chocolate, caffeine, monosodium glutamate), skipping meals, intense physical exertion, female hormonal changes, bright lights, stress, weather changes, and certain medications (oral contraceptives, vasodilators). The cause of cluster headaches is unknown, but they are generally considered to be caused by the hypothalamus activating the trigeminal nerve. These headaches recur 1 to 3 times per day in a period lasting from approximately 2 weeks to 3 months. Cluster headaches do not typically have triggers, but once a cluster headache begins, alcohol, nicotine, and nitroglycerin immediately lead to a severe headache.
Pathophysiology
Attention deficit/hyperactivity disorder (ADHD) might be caused by a dysregulation of the transmitters serotonin, norepinephrine, and dopamine. ADHD occurs primarily in children, usually before the age of 7 years, and may continue through the teenage years. In some cases, it may not be identified until early adulthood. The incidence of ADHD is three to seven times more common in boys than in girls. Characteristic behaviors of the various types of ADHD include inattentiveness, inability to concentrate, restlessness (fidgety), hyperactivity (excessive and purposeless activity), inability to complete tasks, and impulsivity.
The child with ADHD may display poor coordination, and there may be abnormal electroencephalographic (EEG) findings. Intelligence is usually not affected, but learning disabilities are often present. This disorder has also been called minimal brain dysfunction, hyperactivity in children, hyperkinesis, and hyperkinetic syndrome with learning disorder. Some professionals state that ADHD is often incorrectly diagnosed, resulting in many children receiving unnecessary treatment for months or years.
Narcolepsy is characterized by falling asleep during normal waking activities such as driving a car or talking with someone. Sleep paralysis, the condition of muscle paralysis that is normal during sleep, usually accompanies narcolepsy and affects the voluntary muscles. The narcoleptic is unable to move and may collapse.
Amphetamines
Amphetamines stimulate the release of neurotransmitters—norepinephrine and dopamine—from the brain and sympathetic nervous system (peripheral nerve terminals). Amphetamines ordinarily cause euphoria and alertness, but they can also cause sleeplessness, restlessness, tremors, and irritability. Cardiovascular problems such as increased heart rate, palpitations, cardiac dysrhythmias, and increased blood pressure can result from continuous use of amphetamines.
The half-life of amphetamines varies from 4 to 30 hours. Amphetamines are prescribed for narcolepsy and in some cases for ADHD, when amphetamine-like drugs are ineffective. Amphetamine (Adderall) has been effective for controlling ADHD. Dextroamphetamine (Dexedrine) and methamphetamine (Desoxyn) may also be prescribed for some ADHD patients.
Side Effects and Adverse Reactions
Amphetamines can cause adverse effects in the central nervous system and the cardiovascular, gastrointestinal (GI), and endocrine systems. Side effects and adverse reactions include restlessness, insomnia, tachycardia, hypertension, heart palpitations, dry mouth, anorexia, weight loss, diarrhea, constipation, and impotence.
Amphetamine-Like Drugs for ADHD and Narcolepsy
Methylphenidate (Ritalin) and dexmethylphenidate (Focalin), classed as amphetamine-like drugs, are given to increase a child’s attention span and cognitive performance (e.g., memory, reading) and to decrease impulsiveness, hyperactivity, and restlessness. Methylphenidate is also used to treat narcolepsy. There may be potential abuse of methylphenidate; thus it is classified as a controlled-substance schedule (CSS) II drug. Prototype Drug Chart 20-1 illustrates the pharmacokinetics, pharmacodynamics, and therapeutic effects of methylphenidate in the treatment of ADHD and narcolepsy. Amphetamine and amphetamine-like drugs should not be taken in the evening or before bedtime, because insomnia may result.
Modafinil (Provigil) is another drug prescribed for narcolepsy. It increases the amount of time patients with narcolepsy feel awake. Its mechanism of action is not fully known.
Methylphenidate is the most frequently prescribed drug used to treat ADHD. Table 20-1 lists the amphetamines and amphetamine-like drugs and their dosages, uses, and considerations.
TABLE 20-1
AMPHETAMINES AND AMPHETAMINE-LIKE DRUGS
| GENERIC (BRAND NAME) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Amphetamines | ||
| amphetamine sulfate (Adderall, Adderall XR) CSS II | Narcolepsy: A: PO: 5-60 mg/d in divided doses; max: 60 mg/d C: 6-12 y: PO: 5 mg q.d. or b.i.d., increase 5 mg/d weekly until desired response ADHD: C: >12 y: 5 mg b.i.d., increase 10 mg/d weekly until desired response C: 6-12 y: PO: 2.5 mg/d, increase 5 mg/d weekly until desired response; max: 40 mg/d | For narcolepsy, ADHD. Dosage should be minimal to control symptoms in ADHD. CNS and cardiac toxicity may occur. Pregnancy category: C; PB: UK;  : 10 h : 10 h |
| dextroamphetamine sulfate (Dexedrine) CSS II | ADHD: C: 3-5 y: PO: 2.5 mg/d or b.i.d. C: 6-12 y: PO: 5 mg/d or b.i.d., max: 40 mg/d | Uses similar to amphetamines. Has been used for weight loss and narcolepsy. May cause psychosis, aggression, and cardiac events. May cause sudden death in patients with structural cardiac abnormalities. Pregnancy category: C; PB: UK;  : 10-12 h : 10-12 h |
| lisdexamfetamine dimesylate (Vyvanse) CSS II | ADHD: A/C: >12 y: PO: 30 mg/d in morning, may increase 10-20 mg/d weekly, max: 70 mg/d | For ADHD. May cause anorexia, insomnia, headache, and irritability. May cause psychosis, aggression, and cardiac events. May cause sudden death in patients with structural cardiac abnormalities. Pregnancy category: C; PB: UK;  : 10-12 h : 10-12 h |
| Amphetamine-Like Drugs | ||
| methylphenidate HCl (Ritalin) CSS II | See Prototype Drug Chart 20-1. | |
| modafinil (Provigil) CSS IV | A: PO: 200 mg/d in the morning Older adults: PO: 100 mg/d in the morning | For narcolepsy. Does not disrupt nighttime sleep. Common side effects include headache, nausea, diarrhea, and nervousness. Pregnancy category: C; PB: 60%;  : 15 h : 15 h |
| dexmethylphenidate (Focalin) | Immediate-release A and C: >6 y: PO: 2.5 mg b.i.d.; increase 2.5-5 mg/d at weekly intervals; max: 20 mg/d Extended-release: A: PO: 10 mg/d, may increase 10 mg/wk; max: 40 mg/d C: >6: PO: 5 mg/d, may increase 5 mg/wk; max: 30 mg/d | For ADHD. May cause psychosis, aggression, and cardiac events. May cause sudden death in patients with structural cardiac abnormalities. Pregnancy category: C; PB: UK;  : 2.2 h : 2.2 h |
| armodafinil (Nuvigil) | A and C: >16 y: PO: 150-250 mg q.d. in morning | For narcolepsy. Pregnancy category: C; PB: 60%;  : 15 h : 15 h |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 : 1.3-7.7 h
: 1.3-7.7 h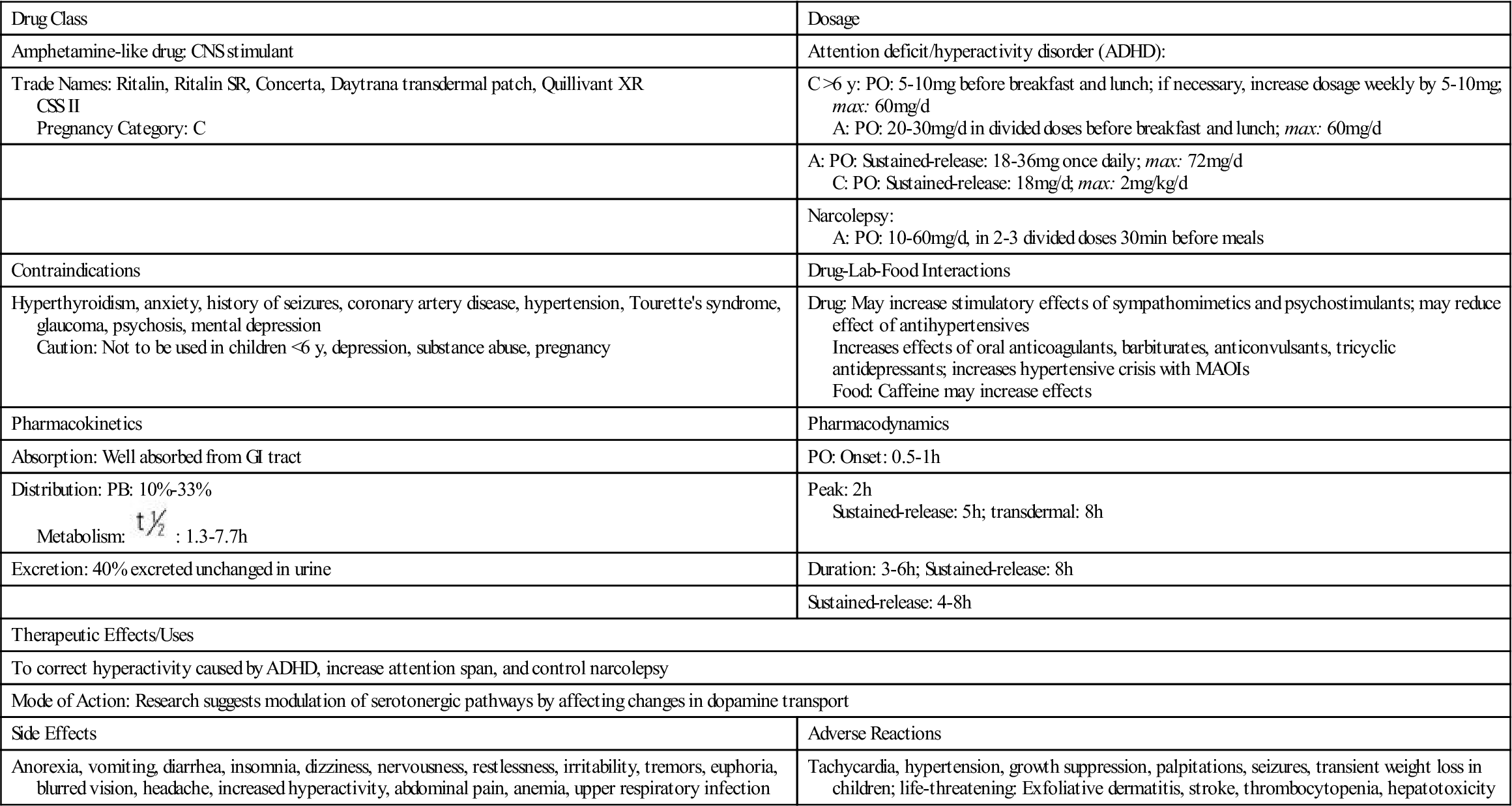
 , half life; UK, unknown; y, year.
, half life; UK, unknown; y, year.