Caring for Mothers and Babies
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe how to meet the safety and security needs of infants and children.
• Identify the signs and symptoms of illness in infants.
• Explain how to help mothers with breast-feeding.
• Describe 3 forms of baby formulas.
• Explain how to bottle-feed babies.
• Describe how to give cord care.
• Describe the purposes of circumcision, needed observations, and the required care.
• Explain how to bathe infants.
• Explain why infants are weighed.
• Describe the care needed by mothers after childbirth.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Mothers and newborns usually have short hospital stays. Some need home care after discharge. The mother or baby may need home care because of:
• Complications before or after childbirth
• Needing help with other young children
• A multiple birth (twins, triplets, and so on)
Babies depend on others for basic needs—physical, safety and security, and love and belonging. A review of growth and development will help you care for babies (Chapter 11).
Safety and Security
Babies cannot protect themselves. They need to feel safe and secure. They feel secure when warm and when wrapped and held snugly. Babies cry to communicate. They cry when wet, hungry, hot or cold, tired, uncomfortable, or in pain. To promote safety and security, respond to their cries—feed them, change diapers as needed, comfort them, talk to them, and so on.
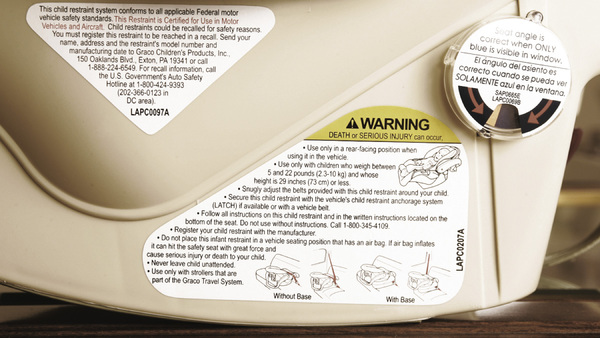
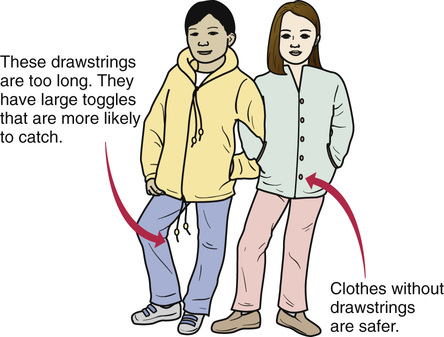
Follow the infant safety measures in Box 52-1. Follow the measures in Chapters 13 and 14 to protect children from burns, poisoning, choking and suffocation, and falls. Also see Appendix D, p. 877.
See Focus on Long-Term Care and Home Care: Safety and Security, p. 802.
Crib Safety
Cribs and crib linens present safety hazards. They can strangle and suffocate the baby. Mattresses, linens, and bumper pads pose many dangers.
• The mattress is covered with a crib sheet. The crib sheet fits snugly.
• Only fitted crib sheets that fit snugly are used. Sheets for larger beds are not used.
• Sheets are not used if they are frayed, worn, or have loose threads or stitching.
Report any hazard to the nurse.
See Focus on Long-Term Care and Home Care: Crib Safety.
Sudden Unexpected Infant Death
Sudden unexpected infant death (SUID) is any sudden and unexpected death in an infant younger than 1 year old. The death may be explained or unexplained. The most common causes of SUID are:
Crib and sleep safety help prevent sudden infant death. See Box 52-1. Lay babies on their backs for sleep. These measures also reduce the risk.
Regular wellness visits are important for infant and child health. Vaccines may protect against sudden infant death.
The mother’s health during pregnancy affects the baby’s risk. Women should receive regular prenatal care. Prenatal care is the health care a woman receives while pregnant. Mothers must avoid smoking, alcohol, and illegal drug use during pregnancy.
Signs and Symptoms of Illness
Babies can become ill quickly. Signs and symptoms may be sudden. You must be very alert. Report any of the signs and symptoms in Box 52-2 at once. Be alert to any change in the baby’s behavior—sleep pattern, cry, appetite, or activity.
Tell the nurse when a sign or symptom began. You may need to measure the baby’s temperature, pulse, and respirations (Chapter 29). The nurse tells you what temperature site to use—tympanic, rectal, temporal artery, or axillary. Apical pulses are taken on infants and young children.
Helping Mothers Breast-Feed
Breast-feeding (nursing) is feeding a baby milk from the mother’s breasts.
• The baby can feed at the mother’s breast.
• The mother can pump milk from her breasts. The baby is fed breast-milk from a bottle.
Babies usually breast-feed every 2 to 3 hours during the first month (8 to 12 times a day). They are fed on demand. That is, they are fed when hungry, not on a schedule. Breast-milk is digested faster than formula. Therefore nursing is needed more often.
Babies nurse for a short time the first few days (5 to 10 minutes at each breast). Eventually nursing time takes 10 to 20 minutes at each breast. The rate varies for each baby.
A feeding ends when:
Nurses help new mothers learn to breast-feed and about breast care. Tell the nurse if the mother or baby is having problems nursing.
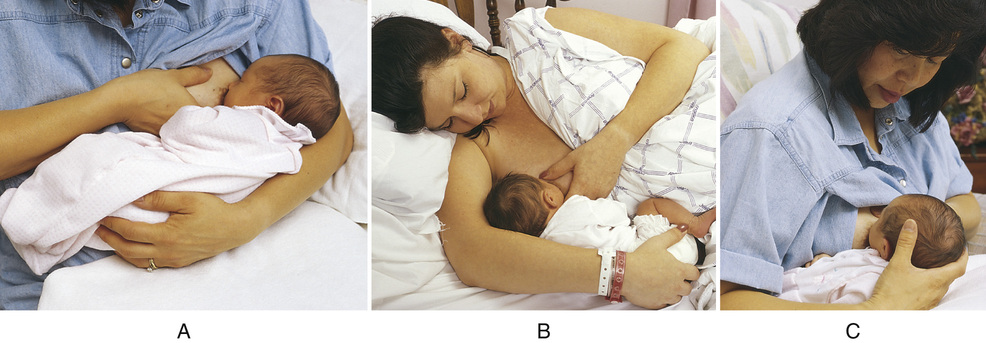
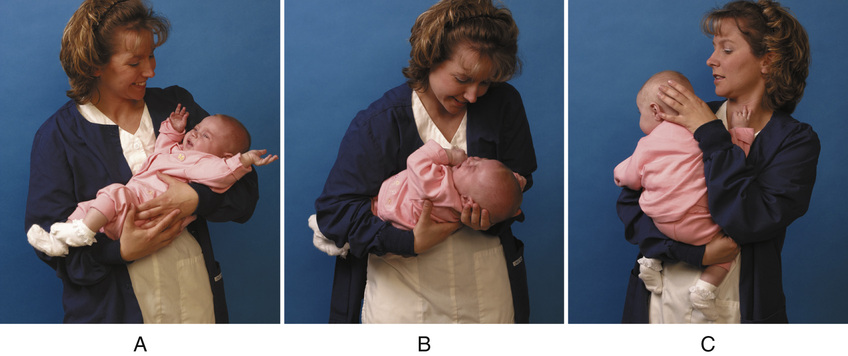
Mothers may need help getting ready to nurse. They may need help with hand-washing and positioning. Provide for privacy and make sure the call light is within reach before leaving the room. Follow the care plan and the measures in Box 52-3.
See Focus on Long-Term Care and Home Care: Helping Mothers Breast-Feed, p. 806.
Bottle-Feeding Babies
Babies who are not breast-fed use formula. The doctor prescribes the formula. It provides the nutrients the infant needs.
Formula comes in 3 forms.
• Ready-to-feed. Ready to use, it is poured from the can into a baby bottle (Fig. 52-11). The can may have more than 1 feeding. Refrigerate the can after opening it. Use the contents within 24 hours.
• Powdered. Container directions tell how much powder and water to use.
• Liquid concentrate. Container directions tell you how much liquid and water to use.
Bottles are prepared 1 at a time or in batches for the whole day. To prepare a bottle:
• Boil water as directed by the nurse.
• Follow the container directions carefully. Measure exact amounts.
• Pour the correct amount of water and formula into the bottle.
• Gently shake or swirl the bottle to mix.
• Dry the outside of the bottle.
• Cap extra bottles (Fig. 52-12). Store them in the refrigerator. Use stored bottles within 24 hours.

 Cleaning Baby Bottles
Cleaning Baby Bottles
Protect the baby from infection. Baby bottles, caps, nipples, and other items must be as clean as possible. Disposable equipment is used in hospitals. Reusable equipment is common in homes. It is carefully washed in hot, soapy water or in a dishwasher. Complete rinsing is needed to remove all soap. Some bottles have plastic liners that are discarded after 1 use.
See Focus on Long-Term Care and Home Care: Cleaning Baby Bottles.
See Promoting Safety and Comfort: Cleaning Baby Bottles.
See procedure: Cleaning Baby Bottles, p. 808.




 inches apart—the width of a soda can. The baby’s head can get caught between larger spaces, causing suffocation and death.
inches apart—the width of a soda can. The baby’s head can get caught between larger spaces, causing suffocation and death. of an inch above the end-panels. This prevents the baby’s clothing from getting caught on the corner posts.
of an inch above the end-panels. This prevents the baby’s clothing from getting caught on the corner posts.