Tami Kathleen Little
Care of Patients with Vascular Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Physiological Integrity
4 Explain the pathophysiology of arteriosclerosis and atherosclerosis.
5 Interpret essential laboratory data related to risk for atherosclerosis.
6 Discuss the role of nutrition therapy in the management of patients with arteriosclerosis.
7 Describe the differences between essential and secondary hypertension.
8 Develop a collaborative plan of care for a patient with essential hypertension.
11 Identify when venous thromboembolism (VTE) and complications of VTE occur.
12 Plan nursing interventions to help prevent VTE.
13 Describe the nurse’s role in monitoring patients who are receiving anticoagulants.
14 Monitor for complications of vascular surgery.
15 Perform a focused vascular assessment.
16 Compare assessment findings associated with Raynaud’s phenomenon and Buerger’s disease.

http://evolve.elsevier.com/Iggy/
Animation: Abdominal Aortic Aneurysm
Animation: Physiology of Blood Pressure
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Concept Map: Hypertension
Key Points
Review Questions for the NCLEX® Examination
The peripheral vascular system is essential for transporting blood to and from distal tissues in the extremities. When peripheral blood vessels are diseased or damaged, especially in the legs, arterial blood flow is impaired, preventing distal areas like the feet from being adequately perfused and oxygenated. The result can be ischemia and necrosis (cell death). Venous disease causes blood to back up into the distal areas and can lead to edema and thromboses (clots) that can be become emboli, a life-threatening complication.
Arteriosclerosis and Atherosclerosis
Pathophysiology
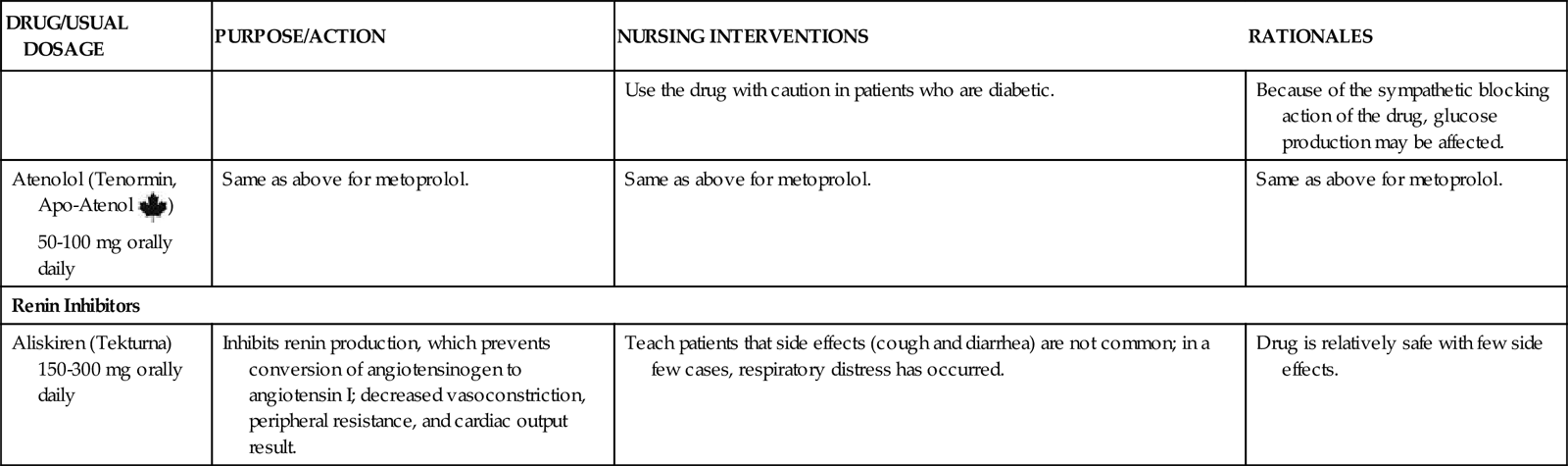
Arteriosclerosis is a thickening, or hardening, of the arterial wall that is often associated with aging. Atherosclerosis, a type of arteriosclerosis, involves the formation of plaque within the arterial wall and is the leading risk factor for cardiovascular disease. Usually the disease affects the larger arteries, such as coronary artery beds; aorta; carotid and vertebral arteries; renal, iliac, and femoral arteries; or any combination of these.
The exact pathophysiology of atherosclerosis is not known, but the condition is thought to occur from blood vessel damage that causes an inflammatory response (see the discussion of inflammation in Chapter 19) (Fig. 38-1). After the vessel becomes inflamed, a fatty streak appears on the intimal surface (inner lining) of the artery. Through the process of cellular proliferation, collagen migrates over the fatty streak, forming a fibrous plaque. The fibrous plaque is often elevated and protrudes into the vessel lumen, partially or completely obstructing blood flow through the artery. Plaques are either stable or unstable. Unstable plaques are prone to rupture and are often clinically silent until they rupture (McCance et al., 2010).
In the final stage, the fibrous plaques become calcified, hemorrhagic, ulcerated, or thrombosed and affect all layers of the vessel. The rate of progression of the process may be influenced by genetic factors; certain chronic diseases (e.g., diabetes mellitus); and lifestyle habits, including smoking, eating habits, and level of exercise.
When stable plaque ruptures, thrombosis (blood clot) and constriction obstruct the vessel lumen, causing inadequate perfusion and oxygenation to distal tissues. Unstable plaque rupture causes more severe damage. After the rupture occurs, the exposed underlying tissue causes platelet adhesion and rapid thrombus formation. The thrombus may suddenly block a blood vessel, resulting in ischemia and infarction (e.g., myocardial infarction) (McCance et al., 2010).
Endothelial (intimal) injury of the major arteries of the body can be caused by many factors. Elevated levels of lipids (fats) like low-density lipoprotein cholesterol (LDL-C) and decreased levels of high-density lipoprotein cholesterol (HDL-C) can cause chemical injuries to the vessel wall. (Chapter 35 discusses lipids in detail.) Chemical injury can also be caused by elevated levels of toxins in the bloodstream, which may occur with renal failure or by carbon monoxide circulating in the bloodstream from cigarette smoking. The vessel wall can be weakened by the natural process of aging or by diseases such as hypertension.
Genetic predisposition and diabetes have a major effect on the development of atherosclerosis. Some patients have familial hyperlipidemia, an elevation of serum lipid levels. In these people, the liver makes excessive cholesterol and other fats. However, some people with hereditary atherosclerosis have a normal blood cholesterol level. The reason for the development and progression of plaque in these patients is not understood (McCance et al., 2010).
Adult patients with severe diabetes mellitus of any age frequently have premature and severe atherosclerosis from microvascular damage. The premature atherosclerosis occurs because diabetes promotes an increase in LDL-C and triglycerides (lipids) in plasma. In addition, arterial damage may result from the effect of hyperglycemia.
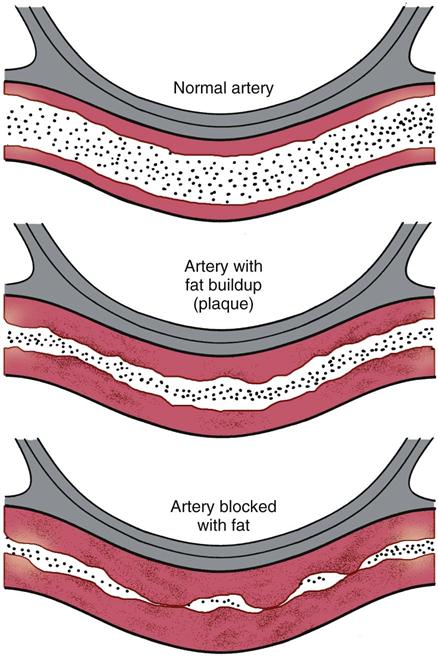
Other factors are indirectly related to atherosclerosis development. A list of risk factors is found in Table 38-1.
TABLE 38-1
RISK FACTORS FOR ATHEROSCLEROSIS
HDL-C, High-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
It is not known exactly how many people have atherosclerosis, but small plaques are almost always present in the arteries of young adults. The incidence can be better quantified by assessing the number of cardiovascular diseases (CVDs) that result from atherosclerosis. An estimated 81 million U.S. adults have one or more types of CVD. Coronary artery disease affects 16 million people, and stroke affects another 6 million. About half of those with CVD are older than 60 years, and many more are middle-aged (American Heart Association [AHA], 2010). The number of people affected by atherosclerosis is likely to increase as the population ages, especially as many of the 79 million “baby boomers” turn 60.
Patient-Centered Collaborative Care
Assessment
Physical Assessment/Clinical Manifestations
The assessment of a patient with atherosclerosis includes a complete cardiovascular assessment because associated heart disease is often present. Because of the high incidence of hypertension in patients with atherosclerosis, assess the blood pressure in both arms.
Palpate pulses at all of the major sites on the body, and note any differences. Palpate each carotid artery separately to prevent blocking blood flow to the brain! Also feel for temperature differences in the lower extremities, and check capillary filling. Prolonged capillary filling (>3 seconds in young to middle-aged adults; >5 seconds in older adults) generally indicates poor circulation, although this indicator is not the most reliable indicator of perfusion. An extremity in a person with severe atherosclerotic disease may be cool or cold with a diminished or absent pulse.
Many patients with vascular disease have a bruit in the larger arteries, which can be heard with a stethoscope or Doppler probe. A bruit is a turbulent, swishing sound, which can be soft or loud in pitch. It is heard as a result of blood trying to pass through a narrowed artery. A bruit is considered abnormal, but it does not indicate the severity of disease. Bruits often occur in the carotid, aortic, femoral, and popliteal arteries.
Laboratory Assessment
Patients with atherosclerosis often have elevated lipids, including cholesterol and triglycerides. Total serum cholesterol levels should be below 200 mg/dL. Elevated cholesterol levels are confirmed by HDL and LDL measurements. Increased low-density lipoprotein cholesterol (LDL-C) (“bad” cholesterol) levels indicate that a person is at an increased risk for atherosclerosis. Low high-density lipoprotein cholesterol (“good” cholesterol) (HDL-C) levels also indicate an increased risk. A desirable LDL-C level is one below 100 mg/dL for healthy people and below 70 mg/dL for those diagnosed with CVD or who are diabetic. A desirable HDL-C level is 40 mg/dL or above (Pagana & Pagana, 2010).
Triglyceride level may also be elevated with atherosclerosis and is an emerging lipid risk factor by the classic Adult Treatment Panel Report No. 3 (ATP III) released by the National Heart, Lung, and Blood Institute (National Cholesterol Education Program, 2002). A level of 150 mg/dL or above indicates hypertriglyceridemia. Women should have a level below 135 mg/dL (Pagana & Pagana, 2010). Elevated triglycerides are considered a marker for other lipoproteins. They also suggest metabolic syndrome, which increases the risk for coronary heart disease (see Table 40-1 and discussion in Chapter 40).
Interventions
Atherosclerosis progresses for years before clinical manifestations occur. Adults who are at risk for the disease can often be identified through cholesterol screening and history. Because of the high incidence in the United States, low-risk people 20 years of age and older are advised to have their total serum cholesterol level evaluated at least once every 5 years. More frequent measurements are suggested for people with multiple risk factors and those older than 40 years.
People with multiple risk factors are grouped into high-risk patient categories termed “coronary heart disease equivalents.” These groups include:
People within these groups are at the same risk level as those who already have vascular disease. Testing and management recommendations from the National Cholesterol Education Program (NCEP) and ATP guidelines have a major preventive focus for people with multiple risk factors.
Interventions for patients with atherosclerosis or those at high risk for the disease focus on lifestyle changes. Teach patients about the need to make daily changes by avoiding or minimizing modifiable risk factors. Modifiable risk factors are those that can be changed or controlled by the patient, such as smoking, weight management, and exercise. Nutrition is one of the most important parts of the risk-reduction plan. Chapter 40 describes how to manage modifiable risk factors in detail in the Health Promotion and Maintenance section, p. 831. If lipoprotein levels do not improve after lifestyle changes, the health care provider may prescribe drug therapy to lower cholesterol and/or triglycerides.
Nutrition Therapy
The Nutrition Committee of the American Heart Association (AHA) established dietary guidelines to promote healthy dietary habits as a strategy to reduce the risk for cardiovascular disease. The guidelines, revised in 2006, focus on the need to achieve and maintain a healthy weight and make appropriate food choices. Although most research focuses on individual nutrients or foods, the AHA guidelines aim to improve overall diet to ensure nutrient adequacy and energy balance (Lichtenstein et al., 2006). The AHA recommends that people consume a variety of nutritious foods including fruits, vegetables, whole grains, fat-free and low-fat dairy products, and lean meats. Specific AHA guidelines to decrease the risk for cardiovascular disease include minimizing fat and cholesterol intake. Chapter 63 describes the most recent U.S. government dietary guidelines, which include increasing daily vegetables and decreasing dairy food fats.
To decrease serum cholesterol level, a total fat intake of less than 30% of total calories should be consumed. Less than 10% of total caloric intake should be from saturated fat, up to 10% of total calories should be from polyunsaturated fat, and 10% to 15% should come from monounsaturated fat. Cholesterol intake should also be less than 300 mg daily.
In collaboration with the dietitian as needed, teach the patient about the types of fat content in food. Meats and eggs contain mostly saturated fats and are high in cholesterol. Recommend canola (rapeseed) oil (rich in monounsaturated fat) and safflower and sunflower oil (rich in polyunsaturated oils) over highly saturated oils such as palm or coconut oil.
The focus of cholesterol management is an aggressive approach to lowering LDL-C values and raising HDL-C levels. Having an LDL-C value of less than 100 mg/dL is optimal; values of 100 to 129 mg/dL are near or less than optimal. Patients with LDL-C values of 130 to 159 mg/dL (borderline high) are advised to follow a fat-modified diet and regular exercise regimen and increase omega-3 fatty acids in their diet or as a supplement. Increased fiber of 25 to 35 g in the daily diet is also recommended. In collaboration with the dietitian, teach patients with LDL-C values of 160 mg/dL or greater (high or very high) to follow a more structured nutritional plan aimed at decreasing saturated fat and cholesterol and, if appropriate, promoting weight loss.
For high-risk people, such as those with high cholesterol, diabetes, or CVD, the AHA recommends the NCEP Therapeutic Lifestyle Changes (TLC) diet, which outlines appropriate medical nutrition therapy. Recommendations include obtaining a patient’s baseline serum cholesterol level and then retesting 6 and 12 weeks after the initial nutritional intervention. If the cholesterol level has not significantly decreased, the patient may be referred to a dietitian for instruction on the NCEP–TLC diet, which limits saturated fat to less than 7% of total calories and cholesterol to less than 200 mg/day.
Drug Therapy
For patients with elevated total and LDL-C levels that do not respond adequately to dietary intervention, the health care provider prescribes one or more lipid-lowering agents (Table 38-2). Drug choice depends on the serum lipid levels. Because most of these drugs can produce major side effects, they are generally given only when nonpharmacologic management has been unsuccessful.
TABLE 38-2
COMMONLY USED DRUGS FOR ATHEROSCLEROSIS
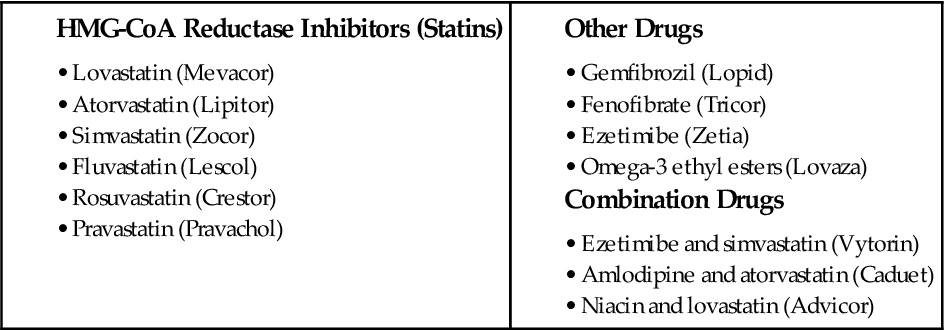
A class of drugs known as 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins) successfully reduces total cholesterol in most patients when used for an extended period. These drugs are also referred to as antihyperlipoproteinemics. Examples include lovastatin (Mevacor), simvastatin (Zocor), and atorvastatin (Lipitor), which lower both LDL-C and triglyceride levels.
A different type of lipid-lowering agent, ezetimibe (Zetia), may be used in place of or in combination with statin-type drugs. This drug inhibits the absorption of cholesterol through the small intestine. Vytorin is a combination drug containing ezetimibe and simvastatin. This drug works two ways—by reducing the absorption of cholesterol and by decreasing the amount of cholesterol synthesis in the liver. Other statin combinations have been developed to improve lipid levels, such as Advicor, a combination of niacin and lovastatin. Aspirin and pravastatin are combined as Pravigard. Amlodipine (Norvasc) and atorvastatin are combined as Caduet to decrease blood pressure while decreasing triglycerides (TGs), increasing HDL, and lowering LDL. Combining drugs may improve adherence for the patient who is often taking multiple drugs.
Complementary and Alternative Therapy
Nicotinic acid or niacin (Niaspan), a B vitamin, may lower LDL-C and very-low-density lipoprotein (VLDL) cholesterol levels and increase HDL-C levels in some patients. It is used as a single agent or in combination with an acid-binding resin drug or a statin. Low doses are recommended because many patients experience flushing and a very warm feeling all over. Higher doses can result in an elevation of hepatic enzymes.
Lovaza (omega-3 ethyl esters) is approved by the Food and Drug Administration (FDA) as an adjunct to diet to reduce TGs that are greater than 500 mg/dL. This drug also decreases plaque growth and inflammation and reduces clot formation (Harris et al., 2008).
Hypertension
Pathophysiology
According to the Seventh Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, hypertension is a systolic blood pressure at or above 140 mm Hg and/or a diastolic blood pressure at or above 90 mm Hg in people who do not have diabetes mellitus. Patients with diabetes and heart disease should have a blood pressure below 130/90 (Joint National Committee, 2003). The Eighth JNC report, due to be released by the U.S. National Institutes of Health in Spring 2012, may likely recommend different values and classifications of patients who are hypertensive.
Mechanisms That Influence Blood Pressure
The systemic arterial pressure is a product of cardiac output (CO) and total peripheral vascular resistance (PVR). Cardiac output is determined by the stroke volume (SV) multiplied by heart rate (HR) (CO = SV × HR). Control of peripheral vascular resistance (i.e., vessel constriction or dilation) is maintained by the autonomic nervous system and circulating hormones, such as norepinephrine and epinephrine. Consequently, any factor that increases peripheral vascular resistance, heart rate, or stroke volume increases the systemic arterial pressure. Conversely, any factor that decreases peripheral vascular resistance, heart rate, or stroke volume decreases the systemic arterial pressure.
Stabilizing mechanisms exist in the body to exert an overall regulation of systemic arterial pressure and to prevent circulatory collapse. Four control systems play a major role in maintaining blood pressure:
• The arterial baroreceptor system
• Regulation of body fluid volume
• The renin-angiotensin/aldosterone system
Arterial baroreceptors are found primarily in the carotid sinus, aorta, and wall of the left ventricle. They monitor the level of arterial pressure and counteract a rise in arterial pressure through vagally mediated cardiac slowing and vasodilation with decreased sympathetic tone. Therefore reflex control of circulation elevates the systemic arterial pressure when it falls and lowers it when it rises. Why baroceptor control fails in hypertension is not clear (McCance et al., 2010).
Changes in fluid volume also affect the systemic arterial pressure. For example, if there is an excess of sodium and/or water in a person’s body, the blood pressure rises through complex physiologic mechanisms that change the venous return to the heart, producing a rise in cardiac output. If the kidneys are functioning adequately, a rise in systemic arterial pressure produces diuresis (excessive voiding) and a fall in pressure. Pathologic conditions change the pressure threshold at which the kidneys excrete sodium and water, thereby altering the systemic arterial pressure.
The renin-angiotensin-aldosterone system also regulates blood pressure (see discussion in Chapter 13). The kidney produces renin, an enzyme that acts on angiotensinogen (a plasma protein substrate) to split off angiotensin I, which is converted by an enzyme in the lung to form angiotensin II. Angiotensin II has strong vasoconstrictor action on blood vessels and is the controlling mechanism for aldosterone release. Aldosterone then works on the collecting tubules in the kidneys to reabsorb sodium. Sodium retention inhibits fluid loss, thus increasing blood volume and subsequent blood pressure.
Inappropriate secretion of renin may cause increased peripheral vascular resistance in patients with hypertension. When the blood pressure is high, renin levels should decrease because the increased renal arteriolar pressure usually inhibits renin secretion. However, for most people with essential hypertension, renin levels remain normal.
The process of vascular autoregulation, which keeps perfusion of tissues in the body relatively constant, appears to be important in causing hypertension. However, the exact mechanism of how this system works is poorly understood.
Classifications of Hypertension
In 2003 the JNC made significant changes in classifying blood pressure in adults. The classification for “normal” adult blood pressure is less than 120 mm Hg systolic and less than 80 mm Hg diastolic. Adults with a blood pressure (BP) of 120 to 139 mm Hg systolic or 80 to 89 mm Hg diastolic, considered “normal” under previous guidelines, are classified as prehypertensive. These patients need lifestyle changes to prevent cardiovascular complications (Table 38-3). The relationship between hypertension and cardiovascular events is direct and independent of other risk factors. The higher the patient’s blood pressure is, the greater the chance for coronary, cerebral, renal, and peripheral vascular disease.
TABLE 38-3
| CLASSIFICATION | BLOOD PRESSURE MEASUREMENT | BLOOD PRESSURE READINGS |
| Normal | Systolic and diastolic | <120 mm Hg <80 mm Hg |
| Prehypertension | Systolic or diastolic | 120-139 mm Hg 80-89 mm Hg |
| Stage 1: Hypertension | Systolic or diastolic | 140-159 mm Hg 90-99 mm Hg |
| Stage 2: Hypertension | Systolic or diastolic | ≥160 mm Hg ≥100 mm Hg |
From Joint National Committee. (2003). The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 03-5233. Bethesda, MD: National Heart, Lung, and Blood Institute.
Control of hypertension has resulted in major decreases in cardiovascular morbidity and mortality. The Healthy People 2020 campaign includes a number of objectives related to hypertension to decrease cardiovascular mortality (Table 38-4).
TABLE 38-4
MEETING HEALTHY PEOPLE 2020 OBJECTIVES
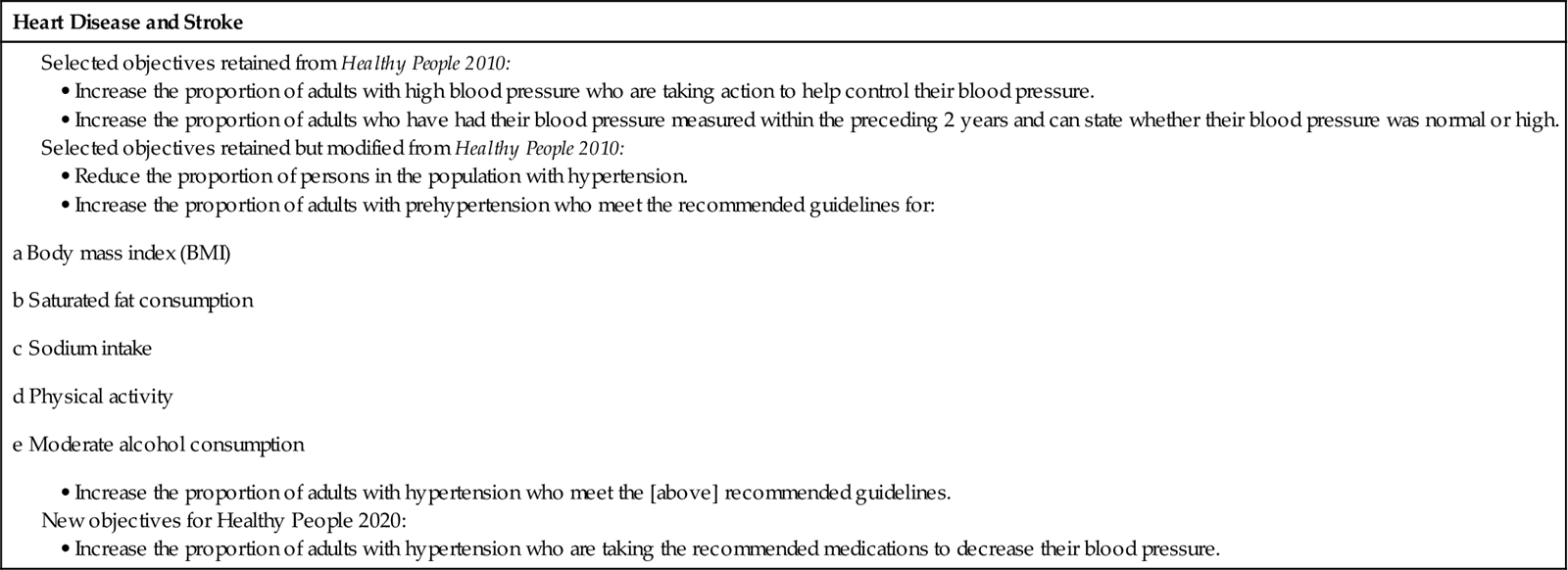
Data from www.healthypeople.gov/2020.
Hypertension can be essential (primary) or secondary (Table 38-5). Essential hypertension is the most common classification. Sustained BP elevation in patients with essential hypertension results in damage to vital organs by causing medial hyperplasia (thickening) of the arterioles. As the blood vessels thicken and perfusion decreases, body organs are damaged. These changes can result in myocardial infarctions, strokes, peripheral vascular disease (PVD), or renal failure.
TABLE 38-5
Essential (Primary) | Secondary |
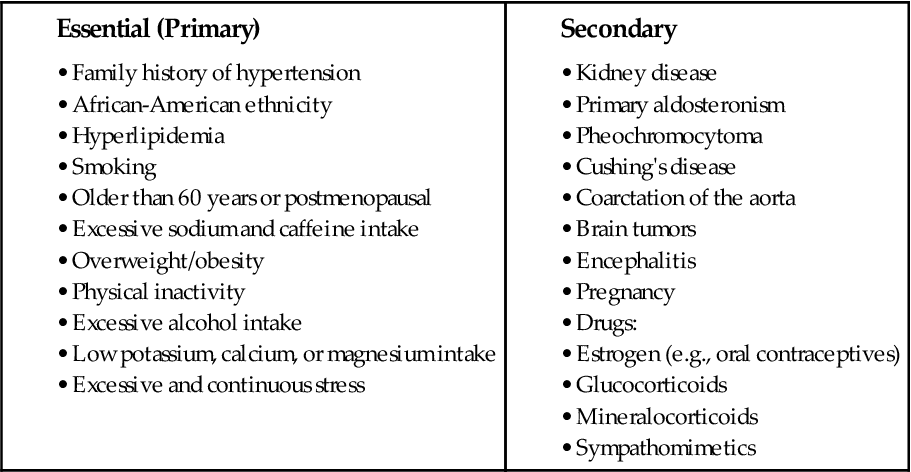
Specific disease states and drugs can increase a person’s susceptibility to hypertension. A person with this type of elevation in blood pressure has secondary hypertension.
Isolated systolic hypertension (ISH) is a major health threat, especially for older adults. It is defined as a systolic BP (SBP) reading at or above 140 with a diastolic BP (DBP) below 90. For years, emphasis was placed on the diastolic BP (DBP) reading and attempts were made to lower this number to under 80. However, as people age, the systolic BP (SBP) becomes more significant because it is a better indicator than DBP of risk for heart disease and stroke. Research has shown that DBP rises until age 55 years and then declines, whereas SBP continues to rise. New research demonstrates a significant association between isolated systolic hypertension and peripheral vascular disease (Safar et al., 2009). In older adults, isolated systolic hypertension is the most common form of hypertension.
Malignant hypertension is a severe type of elevated blood pressure that rapidly progresses. A person with this health problem usually has symptoms such as morning headaches, blurred vision, and dyspnea and/or symptoms of uremia (accumulation in the blood of substances ordinarily eliminated in the urine). Patients are often in their 30s, 40s, or 50s with their systolic blood pressure greater than 200 mm Hg. The diastolic blood pressure is greater than 150 mm Hg or greater than 130 mm Hg when there are pre-existing complications. Unless intervention occurs promptly, a patient with malignant hypertension may experience renal failure, left ventricular failure, or stroke.
Etiology and Genetic Risk
Essential hypertension can develop when a patient has any one or more of the risk factors listed in Table 38-5.
Renal disease is one of the most common causes of secondary hypertension. Hypertension can develop when there is any sudden damage to the kidneys. Renovascular hypertension is associated with narrowing of one or more of the main arteries carrying blood directly to the kidneys, known as renal artery stenosis (RAS). Many patients have been able to reduce the use of their antihypertensive drugs when the narrowed arteries are dilated through angioplasty with stent placement. All patients requiring three or four categories of antihypertensive drugs at high doses should be screened for RAS.
Dysfunction of the adrenal medulla or the adrenal cortex can also cause secondary hypertension. Adrenal-mediated hypertension is due to primary excesses of aldosterone, cortisol, and catecholamines. In primary aldosteronism, excessive aldosterone causes hypertension and hypokalemia (low potassium levels). It usually arises from benign adenomas of the adrenal cortex. Pheochromocytomas originate most commonly in the adrenal medulla and result in excessive secretion of catecholamines, resulting in life-threatening high blood pressure. In Cushing’s syndrome, excessive glucocorticoids are excreted from the adrenal cortex. The most common cause of Cushing’s syndrome is either adrenocortical hyperplasia or adrenocortical adenoma.
Drugs that can cause secondary hypertension include estrogen, glucocorticoids, mineralocorticoids, sympathomimetics, cyclosporine, and erythropoietin. The use of estrogen-containing oral contraceptives is likely the most common cause of secondary hypertension in women. Drugs that cause hypertension are discontinued to reverse this problem.
Incidence/Prevalence
One in every three American adults has high blood pressure or is being treated for hypertension (AHA, 2010). The disease shortens life expectancy. A higher percentage of men than women have hypertension until age 45 years. From 45 to 54 years, women have a slightly higher percentage of hypertension than men. After age 54 years, women have a much higher percentage of the disease (AHA, 2010). The causes for these differences are not known.
Health Promotion and Maintenance
Teach patients ways to decrease risk factors for hypertension, which are the same as those for coronary artery disease (CAD). Risk factor prevention and lifestyle changes are discussed in Chapter 40.
Patient-Centered Collaborative Care
Assessment
History
During history taking, review the patient’s risk factors for hypertension. Collect data on the patient’s age; ethnic origin or race; family history of hypertension; average dietary intake of calories, sodium- and potassium-containing foods, and alcohol; and exercise habits. Also assess any past or present history of kidney or cardiovascular disease and current use of drug therapy or illicit drugs.
Physical Assessment/Clinical Manifestations
When a diagnosis of hypertension is made, most people have no symptoms. However, patients may experience headaches, facial flushing (redness), dizziness, or fainting as a result of the elevated blood pressure. Obtain blood pressure readings in both arms. Two or more readings may be taken at each visit (Fig. 38-2). Some patients have high blood pressure due to anxiety associated with visiting a health care provider. Be sure to take an accurate blood pressure by using an appropriate-size cuff. Anderson et al. (2010) found that forearm blood pressure measurements are as accurate as upper arm blood pressures, especially in patients who are obese. In ambulatory care settings, such as clinics and office practices, wrist blood pressure measurements can be used.
To detect postural (orthostatic) changes, take readings with the patient in the supine (lying) or sitting position and at least 2 minutes later when standing. Orthostatic hypotension is a decrease in blood pressure (20 mm Hg systolic and/or 10 mm Hg diastolic) when the patient changes position from lying to sitting.
Funduscopic examination of the eyes to observe vascular changes in the retina is done by a skilled practitioner. The appearance of the retina can be a reliable index of the severity and prognosis of hypertension.
Physical assessment is helpful in diagnosing several conditions that produce secondary hypertension. The presence of abdominal bruits is typical of patients with renal vascular disease. Tachycardia, sweating, and pallor may suggest a pheochromocytoma (adrenal medulla tumor). Coarctation of the aorta is evidenced by elevation of blood pressure in the arms, with normal or low blood pressure in the lower extremities. Femoral pulses are also delayed or absent.
Psychosocial Assessment
Assess for psychosocial stressors that can worsen hypertension and affect the patient’s ability to adhere to treatment. Evaluate job-related, economic, and other life stressors, as well as the patient’s response to these stressors. Some patients may have difficulty coping with the lifestyle changes needed to control hypertension. Be sure to assess past coping strategies.
Diagnostic Assessment
Although no laboratory tests are diagnostic of essential hypertension, several laboratory tests can assess possible causes of secondary hypertension. Kidney disease can be diagnosed by the presence of protein, red blood cells, pus cells, and casts in the urine; elevated levels of blood urea nitrogen (BUN); and elevated serum creatinine levels. The creatinine clearance test directly indicates the glomerular filtration ability of the kidneys. The normal value is 107 to 139 mL/min for men and 87 to 107 mL/min for women (Pagana & Pagana, 2010). Decreased levels indicate kidney disease.
Urinary test results are positive for the presence of catecholamines in patients with a pheochromocytoma (tumor of the adrenal medulla). An elevation in levels of serum corticoids and 17-ketosteroids in the urine is diagnostic of Cushing’s disease.
No specific x-ray studies can diagnose hypertension. Routine chest radiography may help recognize cardiomegaly (heart enlargement).
An electrocardiogram (ECG) determines the degree of cardiac involvement. Left atrial and ventricular hypertrophy is the first ECG sign of heart disease resulting from hypertension. Left ventricular remodeling can be detected on the 12-lead ECG (see Chapter 40 for discussion of remodeling).
Analysis
The priority problems for patients with hypertension are:
Planning and Implementation
Health Teaching
Planning: Expected Outcomes.
The patient with hypertension is expected to verbalize his or her individualized plan of care for hypertension (see the Concept Map on Hypertension on p. 779).
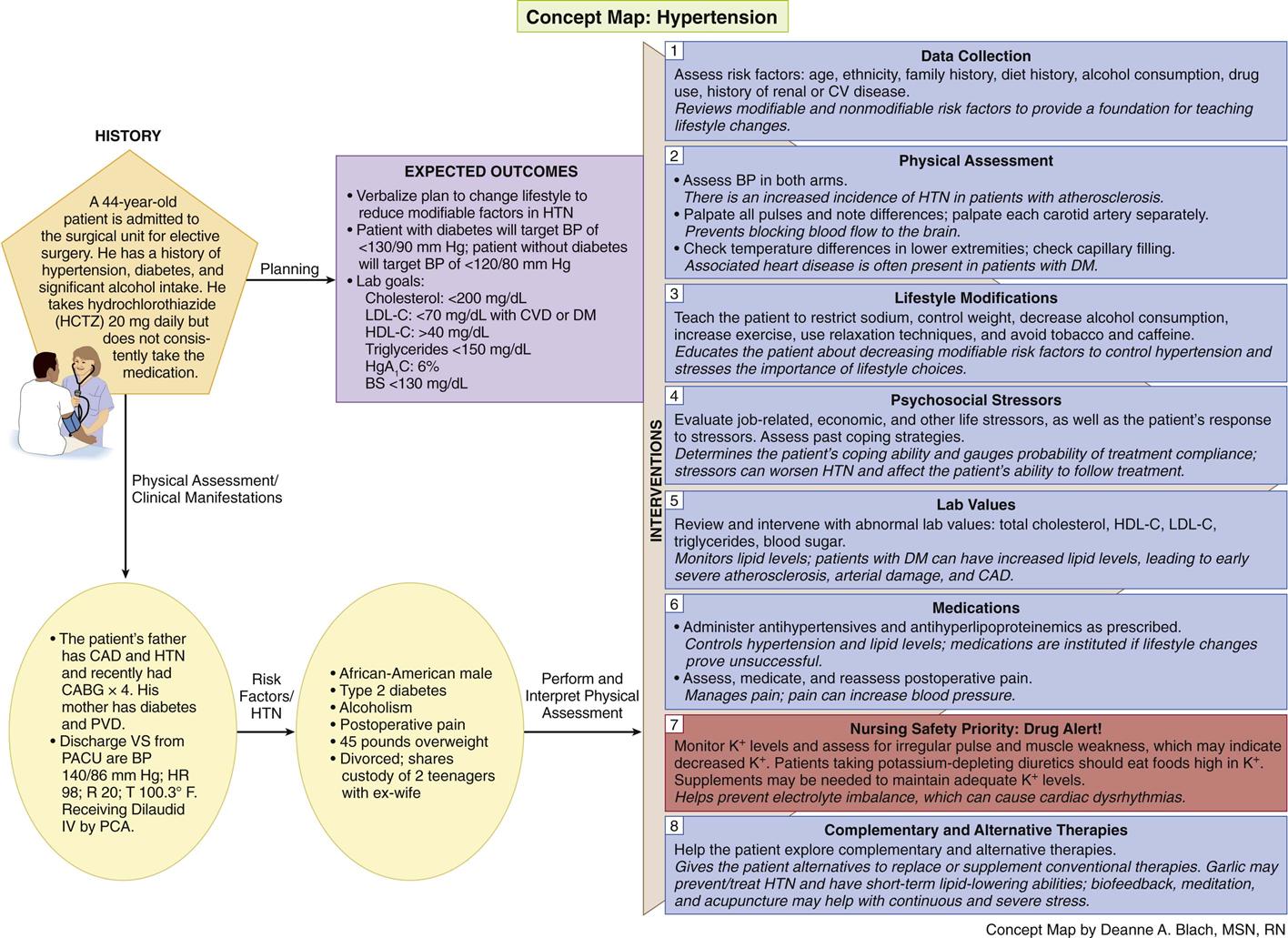
Interventions.
Lifestyle changes are considered the foundation of hypertension control. If these changes are unsuccessful, the health care provider considers the use of antihypertensive drugs. There is no surgical treatment for essential hypertension. However, surgery may be indicated for certain causes of secondary hypertension, such as renal vascular disease, coarctation of the aorta, and pheochromocytoma.
Lifestyle Changes.
In collaboration with the health care team, teach the patient to:
• Restrict sodium intake in the diet
• Reduce weight, if overweight or obese
• Use relaxation techniques to decrease stress
Strategies to help patients make these changes are discussed in Chapter 40.
Complementary and Alternative Therapies.
Garlic has been used for centuries for a number of health problems, but evidence to support its use to prevent hypertension is controversial. Evidence by consensus and case reports does support garlic’s cholesterol-lowering ability and its ability to decrease blood pressure in patients with hypertension (National Center for Complementary and Alternative Medicine, 2010). Teach patients to check with their health care provider before starting garlic or any herbal therapy because of possible side effects and interactions with other herbs, foods, or drugs. Garlic can affect the liver and cause bleeding in some patients, especially if they have invasive procedures such as surgery.
Some patients have also had success with biofeedback, meditation, and acupuncture as part of their overall management plan. These methods may be most useful as adjuncts for patients who experience continuous and severe stress.
Drug Therapy.
Drug therapy is individualized for each patient, with consideration given to culture, age, other existing illness, severity of blood pressure elevation, and cost of drugs and follow-up. Once-a-day drug therapy is best, especially for the older adult, because the more doses required each day, the higher the risk that a patient will not follow the treatment regimen. However, many patients with hypertension need two or more drugs to adequately control blood pressure.
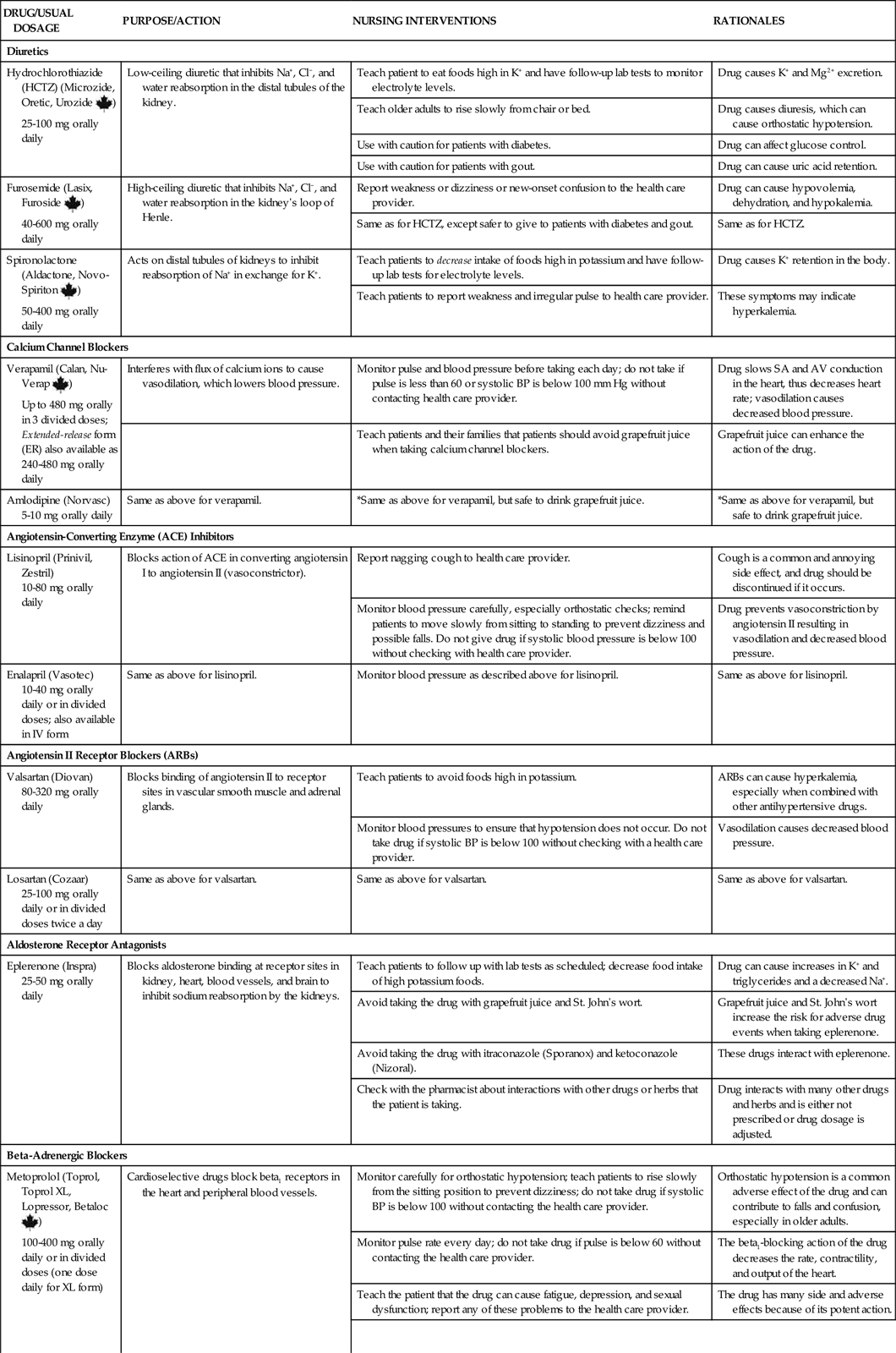
In the largest hypertensive trial done to date, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), the use of diuretics has been practically unmatched in preventing the cardiovascular complications of hypertension. Calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, and aldosterone receptor antagonists may also be given. Examples of commonly used drug classes for hypertension are listed in Chart 38-1.
Diuretics.
Diuretics are the first type of drugs for managing hypertension (Cranwell-Bruce, 2008). Three basic types of diuretics are used to decrease blood volume and lower blood pressure in order of how commonly they are prescribed:
• Thiazide (low-ceiling) diuretics, such as hydrochlorothiazide (HydroDIURIL, Microzide, Oretic, Urozide ![]() ), inhibit sodium, chloride, and water reabsorption in the distal tubules while promoting potassium, bicarbonate, and magnesium excretion. However, they decrease calcium excretion, which helps prevent kidney stones and bone loss (Cranwell-Bruce, 2008). Because of the low cost and high effectiveness of thiazide-type diuretics, they are usually the drugs of choice for patients with uncomplicated hypertension. These drugs can be prescribed as a single agent or in combination with other classes of drugs.
), inhibit sodium, chloride, and water reabsorption in the distal tubules while promoting potassium, bicarbonate, and magnesium excretion. However, they decrease calcium excretion, which helps prevent kidney stones and bone loss (Cranwell-Bruce, 2008). Because of the low cost and high effectiveness of thiazide-type diuretics, they are usually the drugs of choice for patients with uncomplicated hypertension. These drugs can be prescribed as a single agent or in combination with other classes of drugs.
Frequent voiding caused by any type of diuretic may interfere with daily activities. Teach patients to take their diuretic in the morning rather than at night to prevent nocturia.
Other Antihypertensive Drugs.
Calcium channel blockers such as verapamil hydrochloride (Calan, Nu-Verap ![]() ) and amlodipine (Norvasc) lower blood pressure by interfering with the transmembrane flux of calcium ions. This results in vasodilation, which decreases blood pressure. These drugs also block SA and AV node conduction, resulting in a decreased heart rate. Calcium channel blockers are most effective in older adults and African Americans (Cranwell-Bruce, 2008).
) and amlodipine (Norvasc) lower blood pressure by interfering with the transmembrane flux of calcium ions. This results in vasodilation, which decreases blood pressure. These drugs also block SA and AV node conduction, resulting in a decreased heart rate. Calcium channel blockers are most effective in older adults and African Americans (Cranwell-Bruce, 2008).
A newer calcium channel blocker, clevidipine butyrate (Cleviprex), is available only in IV form and must be administered using an infusion pump. This drug is indicated when oral therapy is not possible and is most often used for hypertensive urgency or severe hypertension. The most common side effects are headache and nausea. Monitor the patient’s blood pressure frequently to check for hypotension. A dosage increase of 1 to 2 mg/hr generally produces an additional 2- to 4-mm Hg decrease in systolic blood pressure.
Angiotensin-converting enzyme (ACE) inhibitors, also known as the “pril” drugs, are also used as single or combination agents in the treatment of hypertension. These drugs block the action of the angiotensin-converting enzyme as it attempts to convert angiotensin I to angiotensin II, one of the most powerful vasoconstrictors in the body. This action also decreases sodium and water retention and lowers peripheral vascular resistance, both of which lower blood pressure. ACE inhibitors include captopril (Capoten), lisinopril (Prinivil, Zestril), and enalapril (Vasotec). The most common side effect of this group of drugs is a nagging, dry cough. Teach patients to report this problem to their health care provider as soon as possible. If a cough develops, the drug is discontinued.
Angiotensin II receptor antagonists, also called angiotensin II receptor blockers (ARBs) or the -sartan drugs, make up a group of drugs that selectively block the binding of angiotensin II to receptor sites in the vascular smooth muscle and adrenal tissues by competing directly with angiotensin II but not inhibiting ACE (Cranwell-Bruce, 2008). Examples of drugs in this group are candesartan (Atacand), valsartan (Diovan), and losartan (Cozaar). ARBs can be used alone or in combination with other antihypertensive drugs. These drugs are excellent options for patients who report a nagging cough associated with ACE inhibitors. In addition, these drugs do not require initial adjustment of the dose for older adults or for any patient with renal impairment. Like the ACEs, the ARBs are not as effective in African Americans unless these drugs are taken with diuretics or another category such as a beta blocker or calcium channel blocker (AHA, 2010).
Aldosterone receptor antagonists block the hypertensive effect of the mineralocorticoid hormone aldosterone. Aldosterone increases sodium reabsorption by the kidney and is a significant contributor to hypertension, cardiac and vascular remodeling, and heart failure. Eplerenone (Inspra) lowers blood pressure by blocking aldosterone binding at the mineralocorticoid receptor sites in the kidney, heart, blood vessels, and brain. Generally well tolerated, eplerenone has dose-related adverse effects of hypertriglyceridemia, hyponatremia, and hyperkalemia. Using ACE inhibitors or ARBs at the same time increases the risk for hyperkalemia. Therefore monitor potassium levels carefully, initially every 2 weeks for the first few months and then monthly thereafter.
Beta-adrenergic blockers, identified by the ending -olol, are categorized as cardioselective (working only on the cardiovascular system) and non-cardioselective. Cardioselective beta blockers, affecting only beta-1 receptors, may be prescribed to lower blood pressure by blocking beta receptors in the heart and peripheral vessels. By blocking these receptors, the drugs decrease heart rate and myocardial contractility. Teach patients about common side effects of beta blockers, including fatigue, weakness, depression, and sexual dysfunction. The potential for side effects depends on the “selective” blocking effects of the drug. Atenolol (Tenormin, Apo-Atenol ![]() ), bisoprolol (Zebeta), and metoprolol (Lopressor, Toprol, Toprol-XL, Betaloc
), bisoprolol (Zebeta), and metoprolol (Lopressor, Toprol, Toprol-XL, Betaloc ![]() ) are commonly used cardioselective beta blockers for hypertension.
) are commonly used cardioselective beta blockers for hypertension.
Patients with diabetes who take beta blockers may not have the usual manifestations of hypoglycemia because the sympathetic nervous system is blocked. The body’s responses to hypoglycemia such as gluconeogenesis may also be inhibited by certain beta blockers.
Beta blockers are the drug of choice for hypertensive patients with ischemic heart disease (IHD) because the heart is the most common target of end-organ damage with hypertension. If this drug is not tolerated, a long-acting calcium channel blocker can be used. In patients with unstable angina or myocardial infarction (MI), beta blockers or calcium channel blockers should be used initially in combination with ACE inhibitors or ARBs, with addition of other drugs if needed to control the blood pressure. Best practice for controlling hypertension in post–myocardial infarction (MI) patients includes a combination therapy of beta blockers, ACE inhibitors or ARBs (not as common), and aldosterone antagonists plus intense management of lipids and the use of aspirin. Low-dose aspirin should be considered only once the blood pressure is controlled because of the increased risk for hemorrhagic stroke in patients with uncontrolled hypertension. Patients who are prehypertensive may also benefit from low-dose daily aspirin (Hermida et al., 2009).
Renin inhibitors are effective for mild to moderate hypertension. Aliskiren (Tekturna) is an example and can be used alone or with a thiazide diuretic. Renin is an enzyme produced in the kidneys that causes vasoconstriction, increases peripheral resistance, and increases cardiac output. The result is an increase in blood pressure. Renin inhibitors prevent renin from producing this action. Side effects are minimal and not common, although respiratory distress may occur.
Central alpha agonists act on the central nervous system, preventing reuptake of norepinephrine and resulting in lower peripheral vascular resistance and blood pressure. Clonidine (Catapres) is most commonly used in this drug classification and is usually given as a transdermal patch, providing control of blood pressure for as long as 7 days. Side effects include sedation, postural hypotension, and impotence. This group of drugs is not indicated for first-line management of hypertension but may be added for selected patients.
Alpha-adrenergic antagonists, such as prazosin (Minipress), doxazosin (Cardura), and terazosin (Hytrin), dilate the arterioles and veins. These drugs can lower blood pressure quickly, but their use is limited because of frequent and bothersome side effects.
Promoting Adherence to the Plan of Care
Planning: Expected Outcomes.
The patient with hypertension is expected to adhere to the plan of care, including making necessary lifestyle changes.
Interventions.
Patients who require medications to control essential hypertension usually need to take them for the rest of their lives. Some patients stop taking them because they have no symptoms and have troublesome side effects.
In the hospital setting, collaborate with the pharmacist, as needed, to discuss the outcomes of therapy with the patient, including potential side effects. Assist the patient in tailoring the therapeutic regimen to his or her lifestyle and daily schedule.
Patients who do not adhere to antihypertensive treatment are at a high risk for target organ damage and hypertensive urgency or crisis (causes organ damage, such as kidney or heart [target organs]) (Chart 38-2). Patients in hypertensive crisis are admitted to critical care units, where they receive IV antihypertensive therapy such as nitroprusside (Nipride), nicardipine (Cardene IV), fenoldopam (Corlopam), or labetalol (Normodyne). These drugs act quickly as vasodilators to decrease blood pressure (BP). When the patient’s blood pressure stabilizes, oral antihypertensive drugs are given (Horne & Gordon, 2009).