Rachel L. Palmieri and Donna D. Ignatavicius
Care of Patients with Problems of the Central Nervous System
The Spinal Cord
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
9 Perform a comprehensive health assessment of the patient with a spinal cord injury.
10 Assess the patient with spinal cord health problems for mobility, gait, strength, and sensation.
12 Identify precautions to prevent injury when moving a patient with a spinal cord problem.
13 Apply knowledge of pathophysiology when caring for a patient having autonomic dysreflexia.
14 Explain the clinical manifestations and management options associated with spinal cord tumors.
15 Explain the pathophysiology of multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS).
16 Explain the role of drug therapy in managing patients with spinal cord problems.

http://evolve.elsevier.com/Iggy/
Animation: Spinal Cord Structure
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Concept Map: Multiple Sclerosis
Key Points
Review Questions for the NCLEX® Examination
The spinal cord and its nerves play a major role in maintaining a person’s needs for mobility and sensation. This chapter focuses on back pain, spinal cord injuries and tumors, and diseases that affect the spinal cord, such as multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS). These health problems share a common characteristic of impaired mobility associated with decreased motor function. As a result, the patient’s ability to perform ADLs is often affected. Sensory function also may be impaired, either temporarily or permanently. The spinal cord itself may be damaged, or the spinal nerves leading from the cord to the extremities may be affected. In some cases, both the spinal cord and the nerves are involved.
Back Pain
Back pain is one of the most common reasons for visiting a health care provider. Disabling low back pain is the single greatest cause of injury in the working population. The lumbosacral (lower back) and cervical (neck) vertebrae are most commonly affected because these are the areas where the vertebral column is the most flexible. Acute back pain is usually self-limiting. If the pain continues for 3 months or if repeated episodes of pain occur, the patient has chronic back pain.
Lumbosacral Back Pain (Low Back Pain)
Pathophysiology
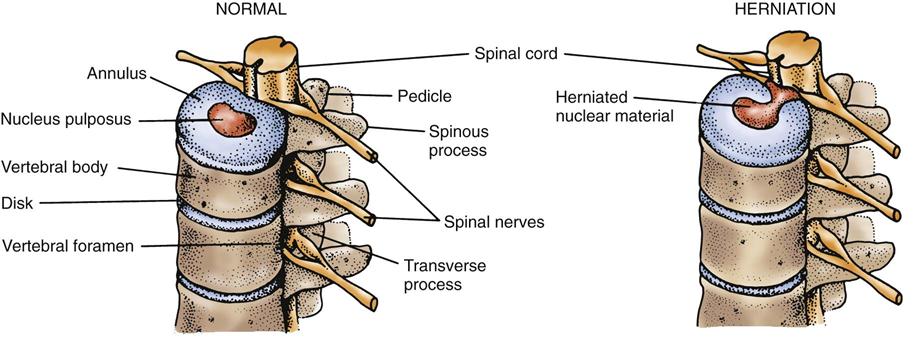
Lumbosacral back pain, referred to as low back pain (LBP), is more common than cervical pain. Acute pain is caused by muscle strain or spasm, ligament sprain, disk (also spelled “disc”) degeneration (osteoarthritis), or herniation of the nucleus pulposus from the center of the disk. Herniated disks occur most often between the fourth and fifth lumbar vertebrae (L4-5) but may occur at other levels. A bulging or herniated nucleus pulposus (HNP) in the lumbosacral area can press on the adjacent spinal nerve (usually the sciatic nerve), causing severe burning or stabbing pain down into the leg or foot (Fig. 45-1). The specific area of pain depends on the level of herniation. Painful muscle spasms of the affected leg also may occur.
In addition to pain, numbness and tingling may be felt in the affected leg because spinal nerves have both motor and sensory fibers. The HNP may press on the spinal cord itself, causing leg weakness and bowel and bladder dysfunction. Sacral spinal nerves are part of the reflex system for the bowel and bladder. They also contain parasympathetic nerve fibers, which help control bowel and bladder function.
Back pain may also be caused by spondylolysis, a defect in one of the vertebrae usually in the lumbar spine. Spondylolisthesis occurs when one vertebra slips forward on the one below it, often as a result of spondylolysis. This problem causes pressure on the nerve roots, leading to pain in the lower back and into the buttocks. Pain or numbness may also occur in the leg and foot. Spinal stenosis, a narrowing of the spinal canal, nerve root canals, or intervertebral foramina is typically seen in people older than 50 years. This narrowing may be caused by infection, trauma, herniated disk, and arthritis and disk degeneration. Most adults older than 50 years have some degree of degenerative disk disease although they may not be symptomatic.
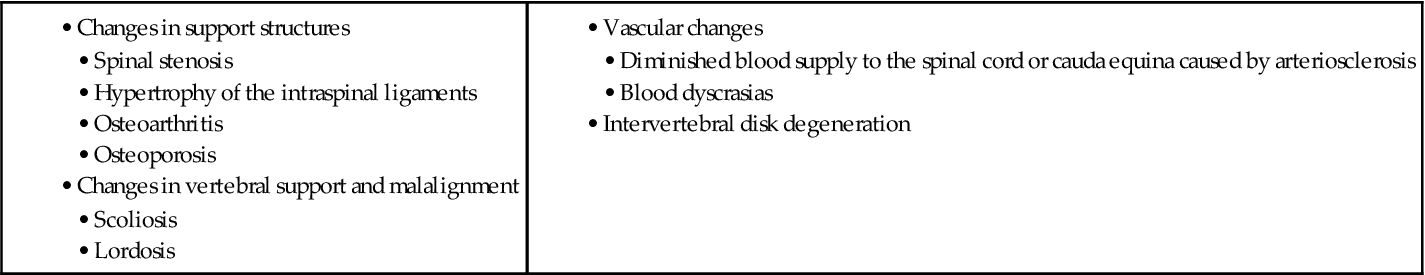
Acute back pain usually results from injury or trauma. The patient typically hyperflexes or twists the back during a vehicular crash, or the injury occurs when the patient lifts a heavy object. Obesity places increased stress on the back muscles and can cause back pain. Smoking has been linked to disk degeneration, possibly caused by constriction of blood vessels that supply the spine. Congenital spinal conditions and scoliosis can also lead to back discomfort. Older adults are at high risk for both acute and chronic LBP. Petite, Euro-American women are at high risk for vertebral compression fractures from osteoporosis, which cause severe pain and decreased mobility. Chart 45-1 provides a list of specific factors that can cause low back pain in the older adult. Vertebral compression fractures are discussed in detail in Chapter 54.
Health Promotion and Maintenance
Many of the problems related to acute back pain can be prevented by recognizing the cause of back pain and taking appropriate preventive measures. For example, good posture, proper lifting techniques, and exercise can significantly decrease the incidence of low back pain. Nurses and other direct care staff members who move and lift patients are at a very high risk for LBP.
The U.S. Occupational Safety and Health Administration (OSHA) mandated that all industries develop and implement a plan to decrease musculoskeletal injuries among their workers. One way to meet this requirement is to develop an ergonomic plan for the workplace. Ergonomics is an applied science in which the workplace is designed to increase worker comfort (thus reducing injury) while increasing efficiency and productivity. An example is equipment design for office furniture that can help reduce back injuries. Chart 45-2 summarizes various ways to help prevent LBP.
Patient-Centered Collaborative Care
Assessment
Physical Assessment/Clinical Manifestations
The patient’s primary concern is continuous pain. Some patients have so much pain that they walk in a stiff, flexed posture, or they may be unable to bend at all. They may walk with a limp, indicating possible sciatic nerve impairment. Walking on the heels or toes often causes severe pain in the affected leg, the back, or both.
Conduct a complete pain assessment as discussed in Chapter 5. Record the patient’s current pain score, as well as the worst and best score since the pain began. Ask if pain occurs or gets worse at night or during rest. Determine if a recent injury to the back has occurred. It is not unusual for the patient to say “I just turned around and felt my back go out.”
Inspect the patient’s back for vertebral alignment and for tenderness and swelling caused by muscle spasm. Painful muscle spasms in the back and affected leg are common because the compressed nerve becomes inflamed and irritates nearby muscle tissue. Patients report stabbing, continuous pain in the muscle closest to the affected disk. They often describe a sharp, burning posterior thigh or calf pain that may radiate to the ankle or toes along the path of one or more spinal nerves. Pain usually does not extend the entire length of the limb. Patients may also report the same type of pain in the middle of one buttock. The pain is often aggravated by sneezing, coughing, or straining. Driving a vehicle is particularly painful.
Ask whether paresthesia (tingling sensation) or numbness is present in the involved leg. Both extremities may be checked for sensation by using a pin or paper clip and a cotton ball for comparison of light and deep touch. The patient may feel sensation in both legs but may experience a stronger sensation on the unaffected side. Those with severe problems may lose both bowel and bladder control from sacral spinal nerve involvement.
If the sciatic nerve is compressed, severe pain occurs when the patient’s leg is held straight and lifted upward. Foot, ankle, and leg weakness may accompany lower back pain. To complete the neurologic assessment, evaluate the patient’s muscle tone and strength. Muscles in the extremity or lower back can atrophy as a result of severe chronic back pain. The patient has difficulty with movement, and certain movements create more pain than others.
Other information that may indicate more serious neurologic problems includes a history of fever and chills, recurrent skin or urinary tract infections, progressive motor and sensory loss, and difficulty with urination or having a bowel movement (due to involvement of sacral nerves). Patients older than 50 years and those with osteoporosis, immunosuppression, long-term use of steroids, or IV drug abuse require more thorough diagnostic studies.
Diagnostic Assessment
Imaging studies for patients who report mild nonspecific back pain may not be done depending on the nature of the pain. Patients with severe or progressive neurologic deficits or who are thought to have other underlying conditions (e.g., cancer, infection) require complete diagnostic assessment. X-rays of the spine are important to exclude fracture, spondylosis, or neoplasm as the causative agent. Flexion-extension views can be very useful to show instability of the spine. The imaging studies of choice are magnetic resonance imaging (MRI) or computerized tomography (CT) scanning. The MRI is usually the first test of choice because it is noninvasive. A CT myelogram is done when a better delineation of the bony anatomy and the specific nerve root involvement is needed. For patients having surgery, some physicians request a diskogram of the affected disk, especially when the level of the injury is not certain.
Electro-diagnostic testing, such as electromyography (EMG) and nerve-conduction studies, may help distinguish motor neuron diseases from peripheral neuropathies and radiculopathies (spinal nerve root involvement). These tests are especially useful in chronic diseases of the spinal cord or associated nerves. Chapter 43 describes these tests in more detail.
Interventions
Management of patients with back pain varies with the severity and chronicity of the problem. Most patients with acute LBP need only a short-term treatment regimen. The health care provider starts with conservative measures. If these are unsuccessful, surgery may be needed. Some patients have continuous or intermittent chronic pain that must be managed for an extended period, perhaps for their entire lives.
Nonsurgical Management
Nonsurgical conservative management of LBP includes positioning, drug therapy, physical therapy, and weight control.
Acute Low Back Pain.
The Williams position is typically more comfortable and therapeutic for the patient with LBP from a bulging or herniated disk. In this position, the patient lies in the semi-Fowler’s position with a pillow under the knees to keep them flexed or sits in a recliner chair. This position relaxes the muscles of the lower back and relieves pressure on the spinal nerve root. Most patients also find that they need to change position frequently. Prolonged standing, sitting, or lying down increases back pain. If the patient must stand for a long time for work or other reason, shoe insoles or special floor pads may help decrease pain.
A firm mattress or a backboard placed under a soft mattress may provide back support for some patients. A flat position is sometimes helpful for the patient with a muscle injury. However, a flat position may aggravate the pain caused by disk trauma or disease.
The health care provider prescribes acetaminophen, muscle relaxants, and NSAIDs for acute LBP. Opioid analgesics are no more effective than nonsteroidal analgesics and should be avoided if at all possible. If they must be used, the course of therapy should be short to prevent adverse drug events. Short-term oral steroids in tapering doses may be prescribed for some patients to rapidly reduce inflammation.
Some patients may need an epidural injection for pain relief. A corticosteroid and an anesthetic are injected to reduce inflammation in the affected area. During a facet joint injection, fluoroscopy is used to insert a needle into the epidural space surrounding the facet and a corticosteroid is injected to coat the nerve roots and outside lining of the joints.
Chronic Low Back Pain.
Patients having chronic low back pain may require an antiepileptic drug (AED) such as gabapentin (Neurontin) or oxcarbazepine (Trileptal) to treat neuropathic (chronic nerve) pain. The health care provider teaches the patient and/or family to start the patient on a low dose. The dose is gradually titrated until pain relief is achieved, the dose is not greater than the provider recommends, and the patient does not experience side effects. Patients should be monitored very carefully for symptoms of hyponatremia (low serum sodium), including generalized skeletal muscle weakness, headache, dizziness, and diarrhea. For older adults, observe for or teach family members to observe for falls due to dizziness and weakness, especially as the drug is increased.
For some patients, an AED is only partially effective for relieving back pain. The health care provider may add a tricyclic antidepressant, such as amitriptyline (Elavil, Levate ![]() ) or desipramine (Norpramin, Pertofrane
) or desipramine (Norpramin, Pertofrane ![]() ), to the drug regimen.
), to the drug regimen.
Some patients with back pain may have temporary relief from heat or cold application. Heat increases blood flow to the affected area and promotes the healing of injured nerves. Moist heat from heat packs or hot towels applied for 20 to 30 minutes at least four times per day is often recommended. Hot showers or baths may also be beneficial, although there is insufficient data to support the use of superficial heat/cold applications for low back pain (van Middelkoop et al., 2011).
The physical therapist (PT) may provide deep heat therapy, such as ultrasound treatments and diathermy. Some patients may receive phonophoresis, which is the application of a topical drug (e.g., lidocaine, hydrocortisone) followed by continuous ultrasound for 10 minutes. Iontophoresis is a similar procedure in which a small electrical current and dexamethasone are typically used. Both procedures push the medication into the subcutaneous tissue and provide longer-lasting pain relief.
The physical therapist also works with the patient to develop an individualized exercise program. The type of exercises prescribed depends on the location and nature of the injury and the type of pain. The patient does not begin exercises until acute pain is reduced by other means. Several specific exercises for LBP are listed in Chart 45-3. A systematic review of 37 studies showed that there is low quality evidence for the effectiveness of exercise for low back pain (van Middelkoop et al., 2011). Water therapy combined with exercise is helpful for some patients with chronic pain. The water also provides muscle resistance during exercise to prevent atrophy.
Weight control may help reduce chronic lower back pain by decreasing the strain on the vertebrae caused by excess weight. If the patient’s weight exceeds the ideal by more than 10%, caloric restriction is recommended. Health care providers must be sensitive when reinforcing the need for patients to lose weight to prevent or to lessen chronic back pain. Positive reinforcement and self-esteem building are integral to the nutrition plan.
Complementary and Alternative Therapies.
The patient may find that nontraditional and complementary therapies provide short-term pain relief. Patients with low back muscle injuries or mild nerve involvement may find relief of pain from chiropractic therapies. The purpose of spinal manipulative therapy (SMT) is to promote alignment and prevent or treat pressure on nerve roots.
Imagery, acupuncture, music therapy, and herbal medicines are examples of other possible pain relief therapies for acute and chronic pain. Rubinstein et al. (2010) conducted a systematic review of research on the effectiveness of complementary and alternative medicine for chronic back pain. They concluded that acupuncture and herbal therapies provide short-term pain relief but spinal manipulation was not as effective. Chapters 2 and 5 describe most of these modalities in detail.
Surgical Management
Surgery is usually performed if conservative measures fail to relieve back pain or if neurologic deficits continue to progress. An orthopedic surgeon and/or neurosurgeon perform these surgeries. Two major types of surgery are used depending on the severity and exact location of pain: minimally invasive surgery (MIS) and conventional open surgical procedures. MIS is not done if the disk is pressing into the spinal cord (central cord involvement).
Preoperative Care.
Preoperative care for the patient preparing for lumbar surgery is similar to that for any patient undergoing surgery (see Chapter 16). Teach the patient about postoperative expectations, including:
• Techniques to get into and out of bed
• Sensations, such as numbness and tingling, that may occur in the affected leg or in both legs
Many patients are discharged to home within 23 hours or the next day after surgery. Therefore, before surgery, teach family members or other caregiver how to assist the patient and what restrictions the patient must follow at home.
A bone graft is done if the patient has a spinal fusion. The surgeon explains from where the bone for grafting will be obtained. The patient’s own bone is used whenever possible, but additional bone from a bone bank may be needed. The surgeon provides verbal and written information about the type and the source of bone for surgery. Be sure that the patient signs an informed consent form before surgery. While the bone graft heals, the patient may wear a back orthotic device for 4 to 6 weeks after surgery, but this is not common practice today. Provide information about the importance of wearing the brace as instructed during the healing process, how to take it off and put it on while maintaining spinal alignment, and how to clean it.
Operative Procedures.
Minimally invasive surgeries (MISs) have the advantage of being associated with less muscle injury, decreased blood loss, and decreased postoperative pain. The primary advantage of these surgical procedures is a shortened hospital stay and the possibility of an ambulatory (same-day) procedure. Spinal cord and nerve complications are also less likely. Several specific procedures are commonly performed.
A local anesthetic is given for the microscopic (or surgical) endoscopic diskectomy (MED) or percutaneous endoscopic diskectomy (PED). The surgeon uses x-ray fluoroscopy to insert an endoscope (arthroscope) next to the affected disk. A special cutting tool or laser probe is threaded through the cannula for removal or destruction of the disk pieces that are compressing the nerve root. A newer procedure combines the PED with laser thermodiskectomy to also shrink the herniated disk before removal. Inpatient hospitalization is not necessary for this procedure.
A microdiskectomy involves microscopic surgery directly through a 1-inch incision. This procedure allows easier identification of anatomic structures, improved precision in removing small fragments, and decreased tissue trauma and pain.
Laser-assisted laparoscopic lumbar diskectomy combines a laser with modified standard disk instruments inserted through the laparoscope using an umbilical (“belly button”) incision. The procedure may be used to treat herniated disks that are bulging but do not involve the vertebral canal. The primary risks of this surgery are infection and nerve root injury. The patient is typically discharged in 23 hours but may go home sooner.
The most common conventional open procedures are diskectomy, laminectomy, and spinal fusion. These procedures involve a surgical incision to expose anatomic landmarks for extensive muscle and soft-tissue dissection. Major complications include nerve injuries, diskitis (disk inflammation), and dural tears (tears in the dura covering the spinal cord).
As the name implies, a diskectomy is removal of a herniated disk. A laminectomy involves removal of part of the laminae and facet joints to obtain access to the disk space. When repeated laminectomies are performed or the spine is unstable, the surgeon may perform a spinal fusion (arthrodesis) to stabilize the affected area. Chips of bone are removed, typically from the iliac crest, or obtained from donor bone and are grafted between the vertebrae for support and to strengthen the back. Metal implants (usually titanium pins, screws, plates, or rods) may be required to ensure the fusion of the spine. Before closing, the surgeon may give an intrathecal (spinal) or epidural dose of long-acting morphine (Duramorph) to decrease postoperative pain.
Interbody cage fusion is a newer spinal implant. A cagelike device is implanted into the space where the disk was removed. Bone graft tissue is packed around the device. As with instrumentation and fusion, the bone graft grows into and around the cage and creates a stable spine at that level.
An adjunct for patients for whom fusion may be difficult is the placement of an implantable direct current stimulation (DCS) device to promote bone fusion. External bone stimulators may also be effective for healing bone fusions.
Postoperative Care.
Postoperative care depends on the type of surgery that was performed. In the postanesthesia care unit (PACU), vital signs and level of consciousness are monitored frequently, the same as for any surgery. Best practices for PACU nursing care are discussed in Chapter 18.
Minimally Invasive Surgery.
Patients go home the same day or the day after surgery with a Band-Aid or Steri-Strips over their small incision. Those having a microdiskectomy may also have a clear or gauze dressing over the bandage. Most patients notice less pain immediately after surgery, but mild oral analgesics are needed for pain control while nerve tissue heals over the next few weeks. In collaboration with the health care provider and physical therapist, teach the patient to follow the prescribed exercise program, which begins immediately after discharge. Patients should start walking routinely every day. Complications of MIS are rare.
Conventional Open Surgery.
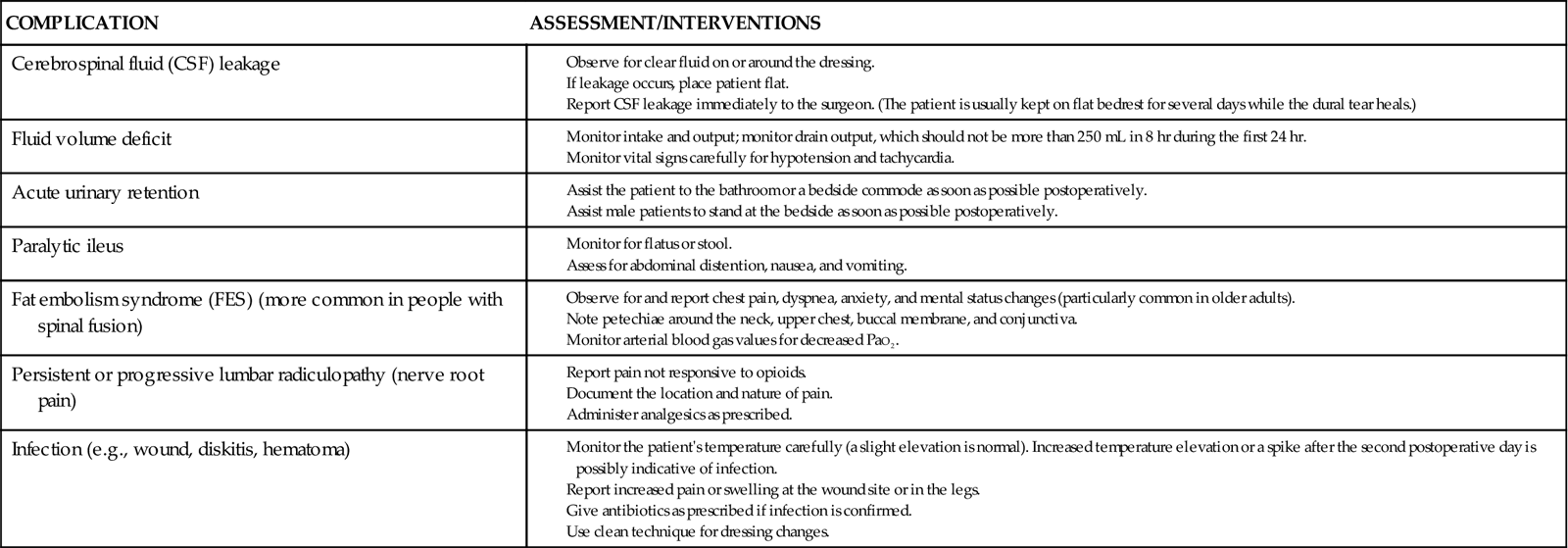
Early postoperative nursing care focuses on preventing and assessing complications that might occur in the first 24 to 48 hours (Chart 45-4). As for any patient undergoing surgery, take vital signs at least every 4 hours during the first 24 hours to assess for fever and for hypotension, which could indicate bleeding or severe pain. Perform a neurologic assessment every 4 hours. Of particular importance are movement, strength, and sensation in the extremities.
Carefully check the patient’s ability to void. Pain and a flat position in bed make voiding difficult, especially for men. An inability to void may indicate damage to the sacral spinal nerves, which control the detrusor muscle in the bladder. Opioid analgesics have also been associated with difficulty voiding. The patient with a diskectomy or laminectomy typically gets out of bed with assistance on the evening of surgery, which may help with voiding.
Pain control may be achieved with patient-controlled analgesia (PCA) with morphine. The route is changed to oral administration after the patient is able to take fluids or the next morning.
Empty the surgical drain, usually a Jackson-Pratt or Hemovac, and record the amount of drainage every 8 hours. The surgeon usually removes the drain in 24 to 36 hours.
Correct turning of the patient in bed is especially important. Teach the patient to log roll every 2 hours from side to back and vice versa. In log rolling, the patient turns as a unit while his or her back is kept as straight as possible. A turning sheet may be used for obese patients. Either turning method may require additional assistance, depending on how much the patient can assist and on his or her weight. Instruct the patient to keep his or her back straight when getting out of bed. He or she should sit in a straight-back chair with the feet resting comfortably on the floor.
Teach the patient to deep breathe every 2 hours to prevent atelectasis (alveolar collapse) and pneumonia. Until the patient can ambulate independently, he or she wears graduated compression stockings, sequential compression devices (SCDs), or pneumatic compression boots (PCBs) to prevent deep vein thrombosis (DVT) and possible pulmonary emboli. Older adults are especially likely to develop these complications of immobility.
When a spinal fusion is performed in addition to a laminectomy, more care is taken with mobility and positioning. The nurse or unlicensed assistive personnel (UAP) assist with log rolling the patient every 2 hours. For the conventional fusion, inspect both the iliac and spinal incision dressings for drainage and make sure they are intact. Remind the patient to avoid prolonged sitting or standing.
Community-Based Care
The patient with back pain who does not undergo surgery is typically managed at home. If back surgery is performed, the patient is usually discharged to home with support from family or significant others. For older adults without a community support system, a short-term stay in a nursing home or transitional care unit may be needed. Collaborate with the case manager or discharge planner, patient, and family to determine the most appropriate placement.
Home Care Management
Inform the patient and family members or significant other that the patient should have a firm mattress to provide support for the entire vertebral column. A bed board or large piece of plywood placed under a soft mattress may suffice. After conventional open back surgery, the patient may be limited in the number of times he or she is allowed to climb stairs each day. However, daily walking is encouraged. The patient can usually return to work in 4 to 6 weeks, depending on the nature of the job and the extent and type of surgery. Some patients may not return for 3 to 6 months if their jobs are physically strenuous. Weight that may be lifted is initially limited to 5 pounds. The amount is gradually increased as healing occurs. Driving is not permitted for several weeks until the surgeon re-evaluates the patient.
Patients having any of the MIS procedures may resume normal activities within a few days up to 3 weeks after surgery, depending on the specific procedure that was done and the condition of the patient. He or she may take a shower on the third or fourth day after surgery. Teach the patient to remove the outer clear or gauze dressing, if any is in place, but leave the Steri-Strips in place for removal by the surgeon or until they fall off. Instruct the patient to contact the surgeon immediately if clear drainage seeps from the incision. Clear drainage usually indicates a meningeal tear and cerebrospinal fluid is leaking.
Teaching for Self-Management
The patient with an acute episode of back pain typically returns to his or her usual activities but may fear a recurrence. Remind the patient that he or she may never have another episode if caution is used. However, continuous or repeated pain can be frustrating and tiring. Encourage the patient and family members to plan short-term outcomes and take steps toward recovering slowly.
After surgery, in collaboration with the physical therapist, instruct the patient to:
The physical therapist reviews and demonstrates the principles of body mechanics and muscle-strengthening exercises. The patient is then asked to demonstrate these principles (Chart 45-5). Formal physical therapy usually begins about 2 weeks after surgery. Teach the patient the importance of keeping all appointments and following the prescribed exercise plan.
The health care provider may want the patient to continue taking anti-inflammatory drugs and muscle relaxants. Remind the patient and family about the possible side effects of drugs and what to do if they occur.
In a few patients, back surgery is not successful. This situation, referred to as failed back surgery syndrome (FBSS), is a complex combination of organic, psychological, and socioeconomic factors. Repeated surgical procedures often discourage these patients, who must continue pain management after multiple operations. Nerve blocks, implantable neurostimulators, and other chronic pain management modalities may be needed on a long-term basis.
Ziconotide (Prialt) is a drug used for severe chronic back pain and FBSS and is given by intrathecal (spinal) infusion with a surgically implanted pump. It is the first available drug in a new class called N-type calcium channel blockers (NCCBs). NCCBs seem to selectively block calcium channels on those nerves that usually transmit pain signals to the brain. Ziconotide is also used for patients with cancer, acquired immune deficiency syndrome (AIDS), and unremitting pain from other nervous system disorders.
Health Care Resources
Assist the patient in identifying support systems (e.g., family, church groups, clubs) after back surgery or FBSS. For example, a spouse may help the patient with exercises or perform the exercises with the patient. Members of a church group may help run errands and do household chores.
The patient with back pain may continue physical therapy on an ambulatory basis after discharge. For unresolved pain, the patient may be referred to pain specialists or clinics, which are usually found in large metropolitan hospitals. A case manager may be assigned to the patient to help with resource management and utilization.
Cervical Neck Pain
Pathophysiology
Cervical neck pain most often results from a bulging or herniation of the nucleus pulposus (HNP) in an intervertebral disk. As seen in Fig. 45-1, the disk tends to herniate laterally where the annulus fibrosus is weakest and the posterior longitudinal ligament is thinned. The result is spinal nerve root compression with resulting motor and sensory manifestations, typically in the neck, upper back (over the shoulder), and down the affected arm. The disk between the fifth and sixth cervical vertebrae (C5-6) is affected most often.
If the disk does not herniate, nerve compression may be caused by osteophyte (bony spur) formation from osteoarthritis. The osteophyte presses on the intervertebral foramen, which results in a narrowing of the disk and pressure on the nerve root. As with sciatic nerve compression, the patient with cervical nerve compression may have either continuous or intermittent chronic pain. When the disk herniates centrally, pressure on the spinal cord occurs.
Cervical pain—acute or chronic—may also occur from muscle strain, ligament sprain resulting from aging, poor posture, lifting, tumor, rheumatoid arthritis, osteoarthritis, or infection. The typical history of the patient includes a report of pain when moving the neck, which radiates to the shoulder and down the arm. The pain may interrupt sleep and may be accompanied by a headache or numbness and tingling in the affected arm. To determine the exact cause of the pain, a number of diagnostic tests may be used, including:
Patient-Centered Collaborative Care
Conservative treatment for acute neck pain is the same as described for low back pain except the exercises focus on the shoulders and neck. The physical therapist teaches the patient the correct techniques for performing “shoulder shrug,” “shoulder squeeze,” and “seated rowing.” If these treatments do not work, some health care providers prescribe a soft collar to stabilize the neck, especially at night. Using the collar longer than 10 days leads to increased pain and decreased muscle strength and range of motion. For that reason, some health care providers do not recommend collars for cervical disk problems.
If conservative treatment is ineffective, surgery may be required, most often using a conventional open surgical approach. A neurosurgeon usually performs this surgery because of the complexity of the nerves and other structures in that area of the spine. Depending on the cause and the location of the herniation, either an anterior or posterior approach is used. An anterior cervical diskectomy and fusion (ACDF) is commonly performed. The patient is fitted with a large neck brace before surgery. Routine preoperative and postoperative care is the same as described in Chapters 16 and 18.
Chart 45-6 summarizes best practices for postoperative care and discharge planning. Complications of ACDF can occur from the brace or the surgery itself. The initial brace is worn for 4 to 6 weeks, depending on the patient. When it is removed, a soft collar is worn for several more weeks, or longer if needed. Potential complications of the anterior surgical approach can be found in Chart 45-7.
Some patients may be candidates for minimally invasive surgery (MIS), such as percutaneous cervical diskectomy through an endoscope, with or without laser thermodiskectomy to shrink the herniated portion of the disk. The care for these patients is very similar to that for the patient with low back pain who has MIS (see discussion of surgical management of patients with low back pain on p. 963).
Spinal Cord Injury
Medical-surgical nurses do not usually care for a patient with an acute spinal cord injury (SCI). However, a patient may be admitted to a medical-surgical unit for complication of the injury or other medical conditions. Caring for a patient with an SCI requires a patient-centered collaborative approach and involves nearly every health care team member to help meet the patient’s expected outcomes.
Despite increased awareness and newer treatments for SCI, the effects of spinal trauma cannot be reversed. However, research continues to find ways to decrease the devastating effects of paralysis. A combination approach of cell transplant, growth of new neurons, drug therapy, and surgery may be the key to restoring some if not all of the patient’s lost motor and sensory function.
Pathophysiology
Loss of motor function (mobility), sensation, reflex activity, and bowel and bladder control often result from an SCI. In addition, the patient may experience significant behavior and emotional problems as a result of changes in body image, role performance, and self-concept.
The SCIs are classified as complete or incomplete. A complete spinal cord injury is one in which the spinal cord has been severed or damaged in a way that eliminates all innervation below the level of the injury. Injuries that allow some function or movement below the level of the injury are described as an incomplete spinal cord injury. Incomplete injuries are more common than complete SCIs.
Mechanisms of Injury
When enough force is applied to the spinal cord, the resulting damage causes many neurologic deficits. Sources of force include direct injury to the vertebral column (fracture, dislocation, and subluxation [partial dislocation]) or penetrating trauma from violence (gunshot or knife wounds). Although in some cases the cord itself may remain intact, at other times the cord undergoes a destructive process caused by a contusion (bruise), compression, laceration, or transaction (severing of the cord, either complete or incomplete) (Nayduch, 2010).
The causes of SCI can be divided into primary and secondary mechanisms of injury. Four primary mechanisms may result in an SCI:
Penetrating injuries to the cord may also occur.
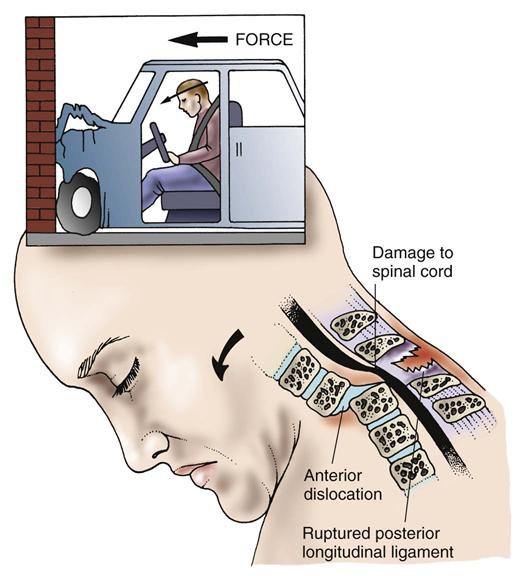
A hyperflexion injury occurs when the head is suddenly and forcefully accelerated (moved) forward, causing extreme flexion of the neck (Fig. 45-2). This type of injury often occurs in head-on vehicle collisions and diving accidents. Flexion injury to the lower thoracic and lumbar spine may occur when the trunk is suddenly flexed on itself, such as occurs in a fall on the buttocks. The posterior ligaments can be stretched or torn, or the vertebrae may fracture or dislocate. Either process may damage the spinal cord, causing hemorrhage, edema, and necrosis.
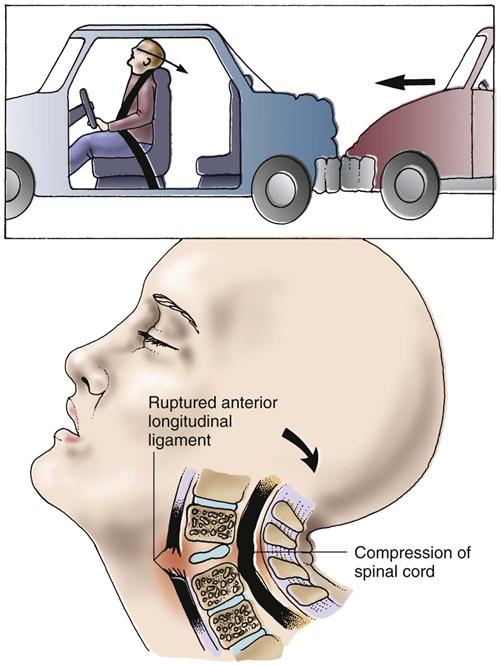
Hyperextension injuries occur most often in vehicle collisions in which the vehicle is struck from behind or during falls when the patient’s chin is struck (Fig. 45-3). The head is suddenly accelerated and then decelerated. This stretches or tears the anterior longitudinal ligament, fractures or subluxates the vertebrae, and perhaps ruptures an intervertebral disk. As with flexion injuries, the spinal cord may easily be damaged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree