Donna D. Ignatavicius
Care of Patients with Esophageal Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
6 Perform focused assessments for patients with esophageal health problems.
7 Apply knowledge of pathophysiology to anticipate complications of GERD.
8 Plan how to teach patients with GERD about drug therapy.
10 Apply knowledge of pathophysiology to recognize complications of esophageal surgical procedures.
11 Plan community-based care for patients diagnosed with esophageal cancer.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The esophagus moves partially digested food from the mouth to the stomach. If food cannot reach the stomach, the patient cannot meet the human need for nutrition. Nutrients in food are necessary for normal body cell function. Common problems of the esophagus that can interfere with digestion and nutrition are caused by inflammation, structural defects or obstruction, and cancer. Patient-centered collaborative care requires dietary and lifestyle changes, as well as medical and surgical therapies.
Gastroesophageal Reflux Disease
Pathophysiology
Gastroesophageal reflux disease (GERD) is the most common upper GI disorder in the United States. It occurs most often in middle-aged and older adults but can affect people of any age. GERD occurs as a result of reflux (backward flow) of GI contents into the esophagus. The incidence of GERD is increasing throughout the world (Chait, 2010).
Reflux produces symptoms by exposing the esophageal mucosa to the irritating effects of gastric or duodenal contents, resulting in inflammation. A person with acute symptoms of inflammation is often described as having reflux esophagitis, which may be mild or severe (McCance et al., 2010).
The reflux of gastric contents into the esophagus is normally prevented by the presence of two high-pressure areas that remain contracted at rest. A 1.2-inch (3-cm) segment at the proximal end of the esophagus is called the upper esophageal sphincter (UES). Another small portion at the gastroesophageal junction (near the cardiac sphincter) is called the lower esophageal sphincter (LES). The function of the LES is supported by its anatomic placement in the abdomen, where the surrounding pressure is significantly higher than in the low-pressure thorax. Sphincter function is also supported by the acute angle (angle of His) that is formed as the esophagus enters the stomach.
The most common cause of GERD is excessive relaxation of the LES, which allows the reflux of gastric contents into the esophagus and exposure of the esophageal mucosa to acidic gastric contents. Nighttime reflux tends to cause prolonged exposure of the esophagus to acid because the supine position decreases peristalsis and the benefit of gravity. Although controversial, Helicobacter pylori may contribute to reflux as well (McCance et al., 2010).
A person having reflux may be asymptomatic and not aware that reflux is occurring. However, the esophagus has only limited resistance to the damaging effects of the acidic GI contents. The pH of acid secreted by the stomach ranges from 1.5 to 2.0, whereas the pH of the distal esophagus is normally neutral (6.0 to 7.0).
Refluxed material is returned to the stomach by a combination of gravity, saliva, and peristalsis. The inflamed esophagus cannot eliminate the refluxed material as quickly as a healthy one, and therefore the length of exposure increases with each reflux episode. Hyperemia (increased blood flow) and erosion (ulceration) occur in the esophagus in response to the chronic inflammation. Gastric acid and pepsin injure tissue. Minor capillary bleeding often occurs with the erosion, but hemorrhage is rare.
During the process of healing, the body may substitute Barrett’s epithelium (columnar epithelium) for the normal squamous cell epithelium of the lower esophagus. Although this new tissue is more resistant to acid and therefore supports esophageal healing, it is considered premalignant. It is associated with an increased risk for cancer in patients with prolonged GERD. The fibrosis and scarring that accompany the healing process can produce esophageal stricture (narrowing of the esophageal opening). The stricture leads to progressive difficulty in swallowing. Uncontrolled esophageal reflux also creates a risk for other serious complications, such as hemorrhage and aspiration pneumonia. GERD may be one of the causes of adult-onset asthma, laryngitis, and dental decay. It has also been associated with cardiac disease.
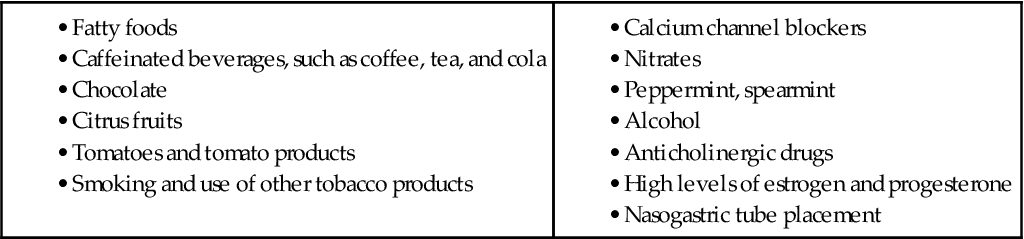
Gastric distention caused by eating very large meals or delayed gastric emptying predisposes the patient to reflux. A number of individual factors, including certain foods and drugs, influence the function of the LES (Table 57-1). Smoking and alcohol also weaken the tone of the LES.
Patients who have a nasogastric tube also have decreased esophageal sphincter function. The tube keeps the cardiac sphincter open and allows acidic contents from the stomach to enter the esophagus. Other factors that increase intra-abdominal and intragastric pressure (e.g., pregnancy, wearing tight belts or girdles, bending over, ascites) overcome the gastroesophageal pressure gradient maintained by the LES and allow reflux to occur. Many patients with obstructive sleep apnea report frequent episodes of GERD. People with hiatal hernias often have reflux because the upper portion of the stomach protrudes through the diaphragm into the thorax to allow acid to reach the esophagus (see later discussion of hiatal hernia).
Overweight and obese patients are at an increased risk for the disease. Increased weight increases intra-abdominal pressure, which contributes to reflux of stomach contents into the esophagus.
Patient-Centered Collaborative Care
Assessment
Ask the patient about a history of heartburn or atypical chest pain associated with the reflux of GI contents. Ask whether he or she has been newly diagnosed with asthma or has experienced morning hoarseness or pneumonia. These symptoms are suggestive of severe reflux reaching the pharynx or mouth or pulmonary aspiration.
Physical Assessment/Clinical Manifestations
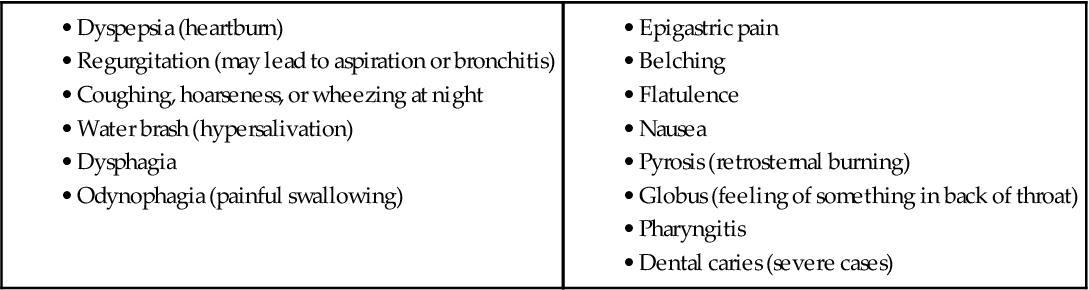
The clinical manifestations of reflux vary in severity, depending on the patient (Chart 57-1). Dyspepsia, also known as “heartburn,” and regurgitation are the main symptoms of GERD. The pain is described as a substernal burning sensation that tends to move up and down the chest in a wavelike fashion. Because heartburn might not be viewed as a serious concern, patients may delay seeking treatment. If the heartburn is severe, the pain may radiate to the neck or jaw or may be referred to the back. The pain typically worsens when the patient bends over, strains, or lies down. Patients may come to the emergency department (ED) fearing that they are having a myocardial infarction (“heart attack”).
With severe GERD, the pain occurs after each meal and lasts for 20 minutes to 2 hours. Patients usually obtain prompt relief by drinking fluids, taking antacids, or maintaining an upright posture.
Regurgitation (backward flow into the throat) of food particles or fluids is common. The patient feels warm fluid traveling up the throat without nausea. If the fluid reaches the level of the pharynx, he or she notes a sour or bitter taste in the mouth. This problem can even occur in an upright position. The danger of aspiration is increased if regurgitation occurs when the patient is lying down.
Eructation (belching), flatulence (gas), and bloating after eating are other common manifestations. Nausea and vomiting rarely occur, and unplanned weight loss is not common.
Assess for crackles in the lung, which can be an indication of associated aspiration. Assess the patient for coughing, hoarseness, or wheezing at night. Bronchitis may occur in those who have long-term regurgitation.
A reflex salivary hypersecretion known as water brash occurs in response to reflux. Water brash is different from regurgitation. The patient reports a sensation of fluid in the throat, but unlike with regurgitation, there is no bitter or sour taste.
Chronic GERD can cause dysphagia (difficulty swallowing). Dysphagia usually indicates a narrowing of the esophagus because of stricture or inflammation. Assess the patient for:
• Whether dysphagia occurs when ingesting solids, liquids, or both
• Whether dysphagia is intermittent or occurs with each swallowing effort
Odynophagia (painful swallowing) can also occur with chronic GERD, but it is rare in people with uncomplicated reflux disease. Severe and long-lasting chest pain may be present if spasms occurring in the esophagus cause the muscle to contract with excess force. The resulting pain can be agonizing and may last for hours.
Other manifestations include chronic cough that occurs mostly at night or when the patient is lying down, asthma, and atypical chest pain. Cough and symptoms of asthma occur when refluxed acid is spilled over into the tracheobronchial tree. Atypical chest pain is thought to be caused by stimulation of pain receptors in the esophageal wall and by esophageal spasm. This type of chest pain can mimic angina and needs to be carefully distinguished from cardiac pain.
Diagnostic Assessment
The most accurate method of diagnosing GERD is 24-hour ambulatory esophageal pH monitoring. This test involves placing a small catheter through the nose into the distal esophagus. The patient is asked to keep a diary of activities and symptoms, and the pH is continuously monitored and recorded. Ambulatory pH monitoring is especially useful in diagnosing patients with atypical symptoms. A wireless monitoring device may be used to promote patient comfort.
Esophagogastroduodenoscopy (EGD) is useful in diagnosing or evaluating reflux esophagitis or in monitoring complications such as Barrett’s esophagus. This test requires the use of moderate sedation during the procedure, and patients must have someone accompany them home after recovery. During the procedure, tissue samples can be obtained for biopsy and strictures can be dilated (see Chapter 55).
Although not as common, esophageal manometry, or motility testing, may be performed when the diagnosis is uncertain. Water-filled catheters are inserted in the patient’s nose or mouth and slowly withdrawn while measurements of LES pressure and peristalsis are recorded. When used alone, manometry is not sensitive or specific enough to establish a diagnosis of GERD.
Interventions
Nonsurgical Management
The purpose of treatment for GERD is to relieve symptoms, treat esophagitis, and prevent complications such as strictures or Barrett’s esophagus. For most patients, GERD can be controlled by nutrition therapy, lifestyle changes, and drug therapy. The most important role of the nurse is patient and family education. Teach the patient that GERD is a chronic disorder that requires ongoing management. The disease should be treated more aggressively in older adults (Chait, 2010).
Nonpharmacologic Interventions.
Nutrition therapy is used to relieve symptoms in patients with relatively mild GERD. Ask about the patient’s basic meal patterns and food preferences. Coordinate with the dietitian, patient, and family about how to adapt to changes in eating that may decrease reflux symptoms.
Teach the patient to limit or eliminate foods that decrease LES pressure, such as chocolate, alcohol, fatty foods (especially fried), caffeine, and carbonated beverages. The patient should also restrict spicy and acidic foods (e.g., orange juice, tomatoes) until esophageal healing can occur, because these foods irritate the inflamed tissue and cause heartburn. Peppermint may also aggravate symptoms.
Large meals increase the volume of and pressure in the stomach and delay gastric emptying. Therefore remind the patient to eat four to six small meals each day rather than three large ones. Encourage patients to eat no food for at least 3 hours before going to bed. Reflux episodes are most damaging at night. Patients may have the most difficulty restricting evening snacks. Advise the patient to eat slowly and chew thoroughly to facilitate digestion and prevent eructation (belching).
The control of GERD involves lifestyle changes to promote health and control reflux (Chart 57-2). Teach the patient to elevate the head by 6 to 12 inches for sleep to prevent nighttime reflux. This can be done by placing blocks under the head of the bed or by using a large, wedge-style pillow instead of a standard pillow.
Teach the patient to sleep in the right side-lying position to decrease the effects of nighttime episodes of reflux. Nighttime reflux is extremely common, and infrequent swallowing in combination with a supine position impairs esophageal clearance. Smoking and alcohol cause decreased LES pressure. Explore the possibility and methods for smoking cessation, and make appropriate referrals. Ask the patient about his or her use of alcoholic beverages. If appropriate, assist the patient in finding alcohol-cessation programs.
Assist the patient in examining approaches to weight reduction. Decreasing intra-abdominal pressure often reduces reflux symptoms. Teach the patient to avoid wearing constrictive clothing, lifting heavy objects or straining, and working in a bent-over or stooped position. Emphasize that these general adaptations are an essential and effective part of disease management and can produce prompt results in uncomplicated cases.
Obese patients often have obstructive sleep apnea, as well as GERD. Those who receive continuous positive airway pressure (CPAP) treatment report improved sleeping and decreased episodes of reflux at night. See Chapter 31 for a discussion of CPAP.
Some drugs lower LES pressure and cause reflux, such as oral contraceptives, anticholinergic agents, sedatives, NSAIDs (e.g., ibuprofen), nitrates, and calcium channel blockers. The possibility of eliminating those drugs causing reflux should be explored with the health care provider.
Drug Therapy.
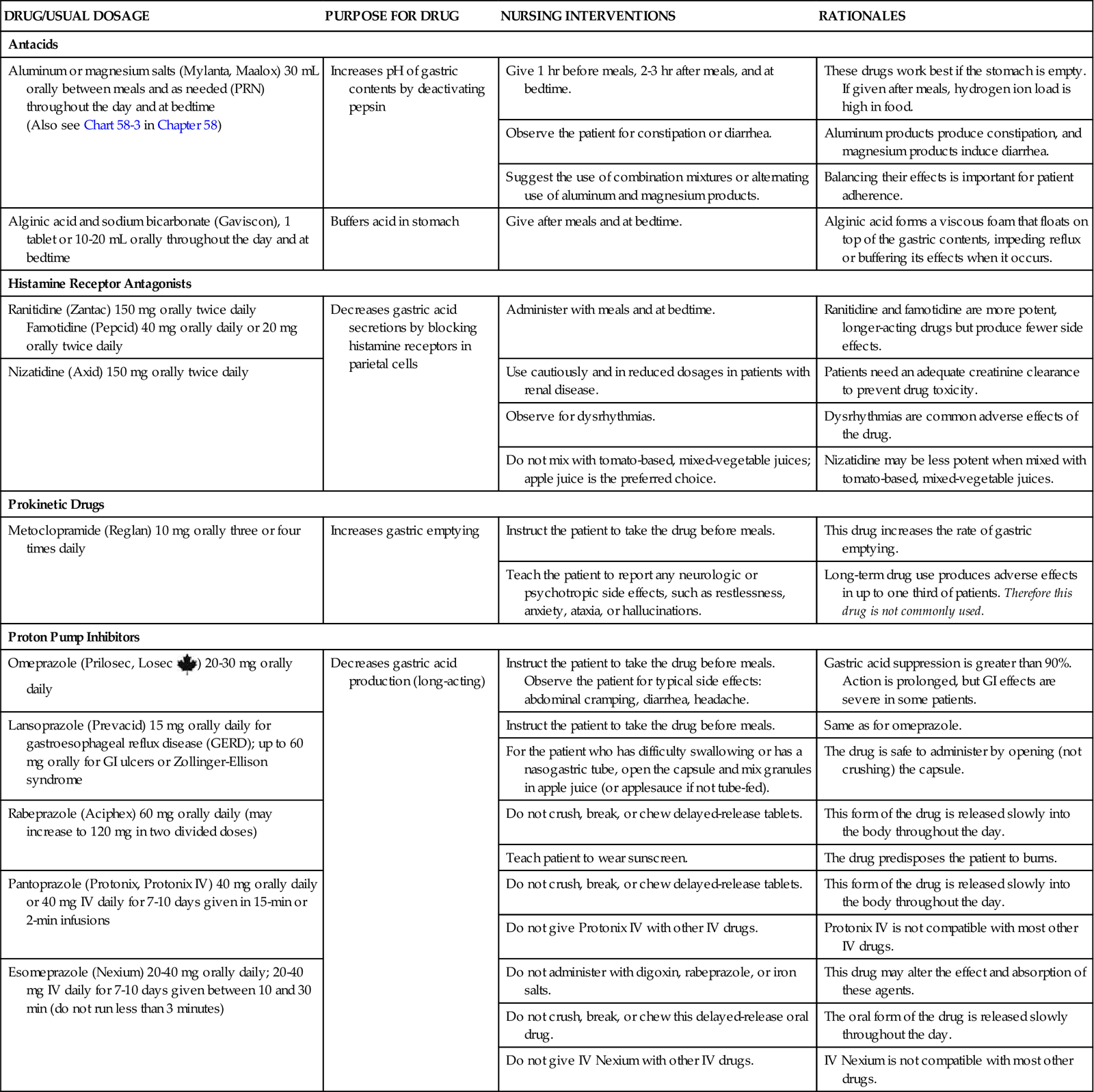
Drug therapy for GERD management includes three major types—antacids, histamine blockers, and proton pump inhibitors. These drugs have one or more of these functions (Chart 57-3):
In uncomplicated cases of GERD, antacids may be effective for occasional episodes of heartburn. Antacids act by elevating the pH level of the gastric contents, thereby deactivating pepsin. They are not helpful in controlling frequent symptoms because their length of action is too short and their nighttime effectiveness is minimal. These drugs also increase LES pressure and therefore are not given for long-term use.
Antacids containing aluminum hydroxide or magnesium hydroxide may be used. Maalox and Mylanta consist of a combination of these two agents. Patients often tolerate them better because they produce fewer side effects, such as constipation and diarrhea. Teach the patient to take the antacid 1 hour before and 2 to 3 hours after each meal. Some antacids are prepared as double-strength (DS) suspensions or tablets. The advantage of DS preparations is that a smaller amount of the drug is required. For example, 30 mL of regular Mylanta equals 15 mL of Mylanta-II (DS preparation).
Gaviscon, a combination of alginic acid and sodium bicarbonate, is often a very effective drug for GERD. It forms a thick foam that floats on top of the gastric contents and theoretically decreases the incidence of reflux. If reflux occurs, the foam enters the esophagus first and buffers the acid in the refluxed material. Remind the patient to take this drug when food is in the stomach.
Histamine receptor antagonists, commonly called histamine blockers, such as famotidine (Pepcid), ranitidine (Zantac), and nizatidine (Axid), decrease acid. With low-dose forms of these drugs available over the counter (OTC) and widely advertised for heartburn, many patients self-medicate before seeking professional assistance from their health care provider. When patients who have self-medicated with OTC preparations have uncontrolled symptoms, the health care provider usually prescribes a higher dose.
Ranitidine and the other preparations are long acting, allowing less-frequent dosing. They also appear to produce fewer side effects and may be safe for long-term use. Although these drugs do not affect the occurrence of reflux directly, they do reduce gastric acid secretion, improve symptoms, and promote healing of inflamed esophageal tissue.
Proton pump inhibitors (PPIs), such as omeprazole (Prilosec), rabeprazole (Aciphex), pantoprazole (Protonix), and esomeprazole (Nexium), are the main treatment for more severe GERD. Some PPIs are available as OTC drugs. These agents provide effective, long-acting inhibition of gastric acid secretion by affecting the proton pump of the gastric parietal cell. PPIs reduce gastric acid secretion and can be given in a single daily dose. If once-a-day dosing fails to control symptoms, twice-daily dosing may be used. A newer PPI, omeprazole/sodium bicarbonate (Zegerid), is the first immediate-release PPI and is designed for short-term use. Another newer PPI, dexlansoprazole (Kapidex), is a dual-release (delayed-release) drug that is available in several dosages but tends to be associated with more side and adverse effects than some of the other PPIs.
Some PPIs, such as Nexium and Protonix, may be administered in IV form for short-term use to treat or to prevent stress ulcers that can result from surgery. PPIs promote rapid tissue healing, but recurrence is common when the drug is stopped. Long-term use may mask reflux symptoms, and stopping the drug determines if reflux has been resolved. Long-term use may also cause community-acquired pneumonia and GI infections.
Research has also found that long-term use of proton pump inhibitors may increase the risk for hip fracture, especially in older adults. PPIs can interfere with calcium absorption and protein digestion and therefore reduce available calcium to bone tissue. Decreased calcium makes bones more brittle and likely to fracture, especially as people age (Chait, 2010).
Endoscopic Therapies.
In the past 15 years, several noninvasive endoscopic procedures have been approved for severe GERD. Two techniques used are the Stretta procedure and endoluminal gastroplication. These nonsurgical methods are becoming more popular and may often replace surgery for GERD when other measures are not effective. Patients who are very obese or have severe symptoms may not be candidates for these procedures.
In the Stretta procedure, the physician applies radiofrequency (RF) energy through the endoscope using needles placed near the gastroesophageal junction. The RF energy decreases vagus nerve activity, thus reducing discomfort for the patient. This nonsurgical procedure has also been approved for patients with Barrett’s esophagus (Bulsiewicz & Shaheen, 2011).
In the gastroplication procedure, the physician tightens the LES through the endoscope using sutures near the sphincter. Chart 57-4 outlines discharge instructions for endoscopic therapies.
The advantages of endoscopic therapies compared with surgery include:
• Use of light or moderate sedation (rather than general anesthesia)
• Ambulatory care procedure (rather than an inpatient stay)
• Short procedure (45 minutes versus several hours)
• 1 to 2 days absence from work (rather than 2 to 3 weeks)
• No antibiotics and lower complication rate, including fewer deaths
Surgical Management
A very small percentage of patients with GERD require anti-reflux surgery. It is usually indicated for otherwise healthy patients who have failed to respond to medical treatment or have developed complications related to GERD. Various surgical procedures may be used through conventional open techniques or laparoscope.
Laparoscopic Nissen fundoplication (LNF) is a minimally invasive surgery (MIS) and is the gold standard for surgical management. A discussion of this procedure can be found in the next section (Hiatal Hernia) in the Surgical Management discussion. Patients who have surgery are encouraged to continue following the basic anti-reflux regimen of antacids and nutritional therapy because the rate of recurrence is high.
Hiatal Hernia
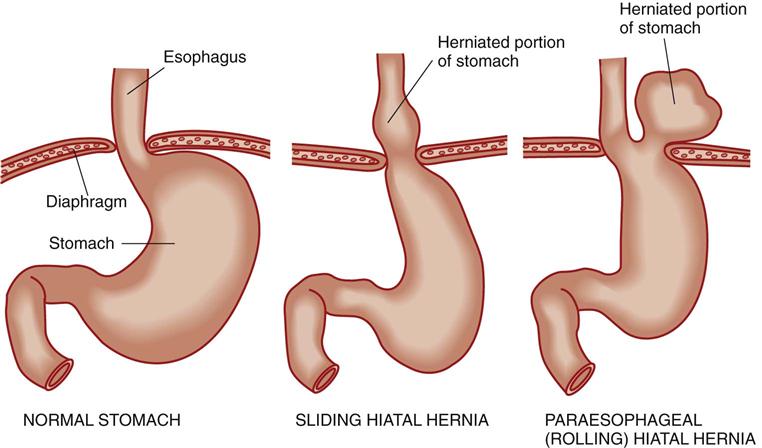
Hiatal hernias, also called diaphragmatic hernias, involve the protrusion of the stomach through the esophageal hiatus of the diaphragm into the chest. The esophageal hiatus is the opening in the diaphragm through which the esophagus passes from the thorax to the abdomen. Most patients with hiatal hernias are asymptomatic, but some may have daily symptoms similar to those with GERD (McCance et al., 2010).
Pathophysiology
The two major types of hiatal hernias are sliding hernias and paraesophageal (rolling) hernias. Sliding hernias are the most common type. The esophagogastric junction and a portion of the fundus of the stomach slide upward through the esophageal hiatus into the chest, usually as a result of weakening of the diaphragm (Fig. 57-1). The hernia generally moves freely and slides into and out of the chest during changes in position or intra-abdominal pressure. Although volvulus (twisting) and obstruction do occur rarely, the major concern for a sliding hernia is the development of esophageal reflux and its complications (see Gastroesophageal Reflux Disease section earlier in this chapter). The development of reflux is related to chronic exposure of the lower esophageal sphincter (LES) to the low pressure of the thorax, which significantly reduces the effectiveness of the LES. Symptoms associated with decreased LES pressure are worsened by positions that favor reflux, such as bending or lying supine. Coughing, obesity, and ascites also increase reflux symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree